Skills and simulation are core components of a midwife's development, and are implemented both in pre-registration and post-registration curriculum programmes, professional standards and embedded in everyday clinical practice. It is imperative to recognise the similarities and differences between skills and simulation, and how focus on these learning strategies can emphasise experiential learning and the promotion of reflection (Berragan, 2011).
The International Confederation of Midwives (2021) state that midwifery has a ‘unique body of knowledge, skills and professional attitudes drawn from disciplines shared by other health professions, such as science and sociology but practised by midwives within a professional framework of autonomy, partnership, ethics and accountability’. This demonstrates that midwives have a unique set and combination of skills in which to provide safe, effective and outcome-driven care, protecting the normal physiological processes of pregnancy and birth in an ever-increasing complex world.
When referring to midwifery skills, the Nursing and Midwifery Council's (2019a; 2019b) standards for education and training, and standards for midwives define these in multiple sections both individually and combined. Skills can be clinical or non-clinical. Take for example ‘domain 6’, the midwife as a skilled practitioner ie specific antenatal, intrapartum and postnatal skills, communication skills, digital skills, professional skills, clinical skills, interpersonal skills and leadership skills. All of these specific and diverse skills underpin the role of the midwife in the 21st century (see Figure 1).
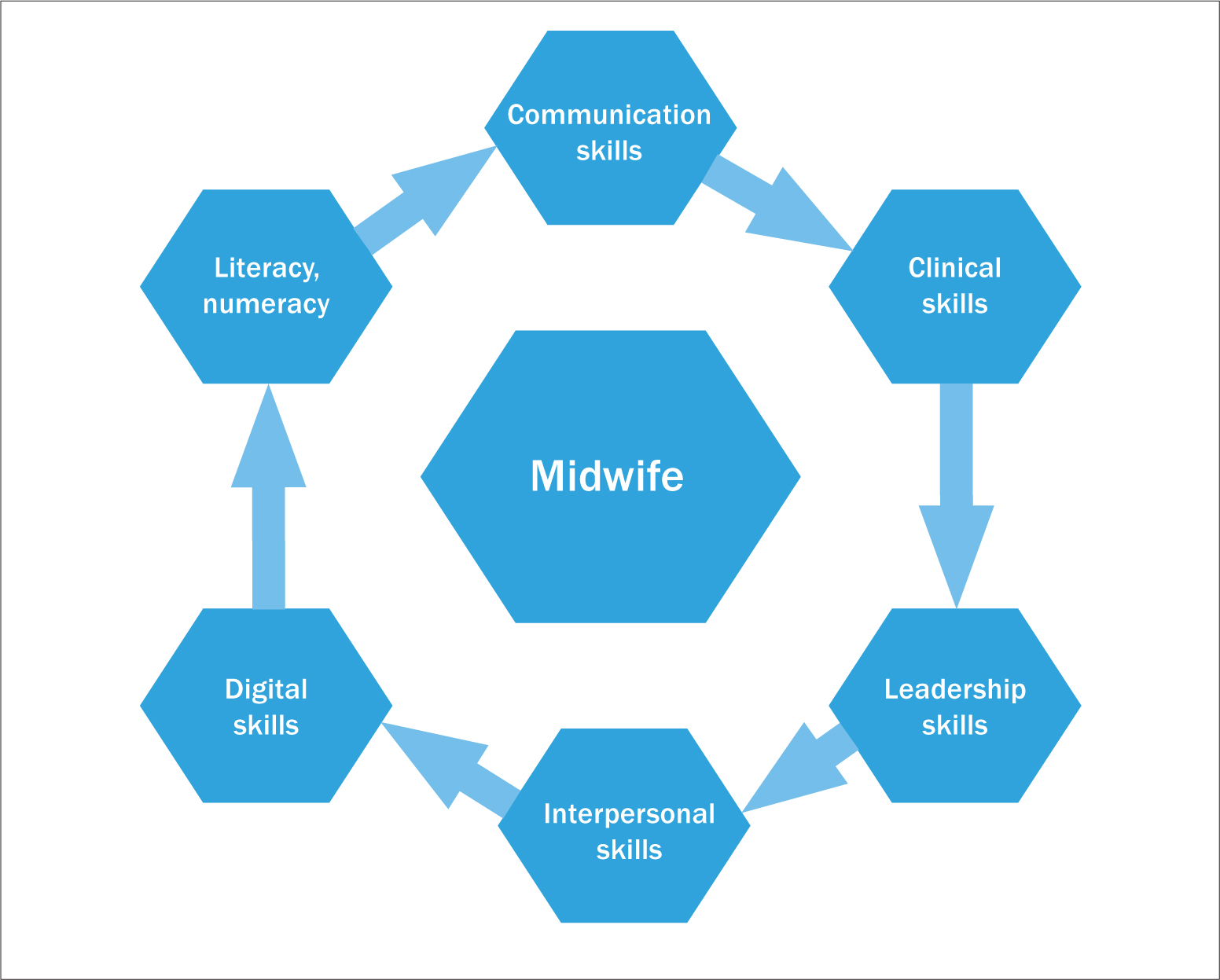 Figure 1. A simulation of combined midwifery skills in the 21st century
Figure 1. A simulation of combined midwifery skills in the 21st century
Research has shown that introducing skills and simulation at undergraduate level can create links between theory and practice by applying individual and combined skills, both clinical and non-clinical, which results in a direct impact on clinical practice (Cooper, 2012).
While most studies have concentrated on evaluating the experience of qualified professionals, there is a growing body of evidence that demonstrates the advantages of embedding high fidelity skills and simulation training within undergraduate programmes. The field is progressing rapidly with more frequent use of not only role play but using artificial intelligence, virtual reality simulators, and other innovations in technology enhanced learning. These combinations of practical-based skills and digital software and hardware innovations bring midwifery practice into the 21st century and will enable students to develop into qualified practitioners ready to practise safely and effectively using a combination of theory, and evidence-based techniques and skills.
There are many definitions of simulation, or simulation-based education/learning pertinent to health and care. Professor DM Gaba, in his article, ‘The future vision of simulation in healthcare’ (2004) states that ‘simulation is a technique – not a technology – to replace or amplify real experiences with guided experiences that evoke or replicate substantial aspects of the real world in a fully interactive manner’.
Simulation, therefore, can be defined as practising and implementing core midwifery skills within an appropriate environment. It seeks to mirror the clinical reality of care (McKenna et al, 2011; Cooper, 2012). By creating an artificial representation of a real-world practice scenario that supports student development and assessment through experiential learning with the opportunity for repetition, feedback, evaluation and reflection can improve safety by enhancing knowledge, behaviours and skills.
The World Health Organization (2018) ‘Simulation in nursing and midwifery education’ and the HEE (2018) ‘Standards framework for simulation-based education’ promote simulation as a positive, active learning pedagogy that benefits students, educators and professionals and local and wider communities and healthcare organisations.
This approach aligns to a spiral curriculum by enabling students to move through Benners level of competence framework (1984) to transition from novice to expert (see Figure 2). Evidence demonstrates that this approach leads to deeper schematic learning using experiential learning and reflexivity (Berragon, 2010) and can be applied from the beginning of a learner's journey through to ongoing expert practice and competence. A pilot study (Cioffi et al, 2005) investigated the effects of a simulation strategy on the clinical decision-making process compared to lecture-based formats. Results showed that the simulation group demonstrated higher clinical information management and decision-making (Cioffi et al, 2005).
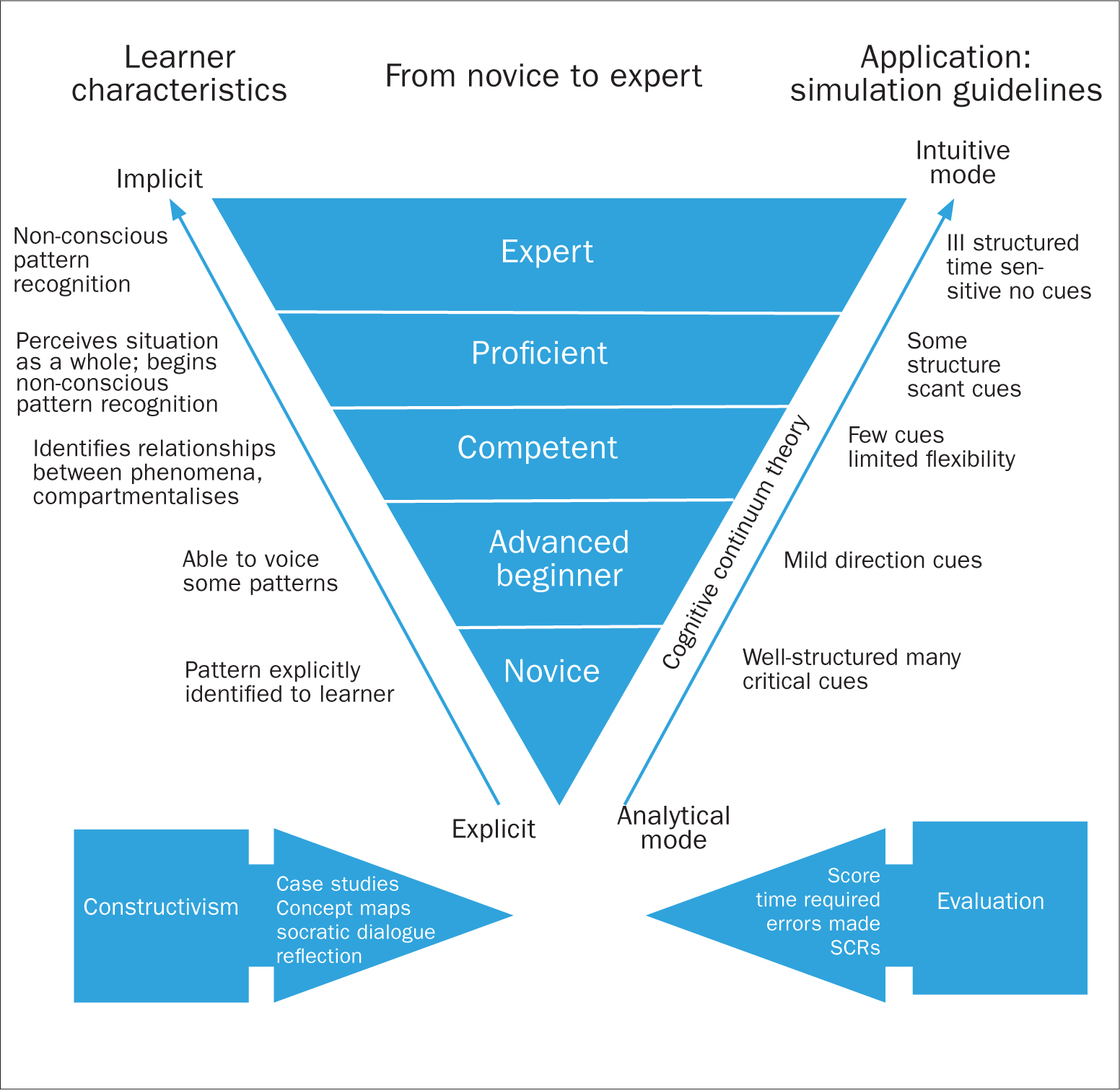 Figure 2. A framework for promoting excellence and power in clinical practice (Based on Benner, 1984 from Novice to expert.
Figure 2. A framework for promoting excellence and power in clinical practice (Based on Benner, 1984 from Novice to expert.
Effective simulation training for undergraduates and postgraduates requires extensive preparation to implement a realistic and effective clinical scenario and debriefing is necessary following a simulated training session to review any positive or negative aspects of the learning experience (Kirkham, 2018). Simulation training assists students to reflect on their experiences and what they have learnt otherwise known as reflection-in-action. An effective simulated training session should assist students to practise clinical techniques in a safe environment, understand the consequences of their actions and practise what they have learnt.
Interprofessional working is an expected part of registered practice and considered an essential part of the continued professional development of clinicians (National Maternity Review, 2016). By using simulation training in practice using a mixed multidisciplinary team human factors can also be considered, which include non-technical skills, such as leadership, communication, teamwork, decision-making and situational awareness (White, 2012). They are defined as the interactions between people and a system which in a healthcare context refers to the processes and procedures that dictate how care is delivered in an organisation (Norris, 2009; Reid and Bromiley, 2012).
Embedding and providing opportunities for regular practice of midwifery skills and simulation throughout a midwife's training and career will enable progression to ‘expert’ in the field enabling increased safety and quality of maternity care to women and families.


