The way in which healthcare organisations respond and learn following patient safety incidents has been repeatedly highlighted as a cause for concern. Getting that right has never been as important as it is at the time of a national pandemic. Where things have had to adapt and change rapidly, new and unforeseen problems can arise.
In addition, ‘maternity scandals’ are increasingly being reported, where thousands of families have been impacted by substandard care, leading to tragic and life-changing outcomes (Buchanan, 2020; Ng, 2020). It comes as no surprise that a ‘focus on learning and best practice’ is listed as one of the five key drivers for delivering safer maternity care as part of the national maternity safety ambition and action plan (Department of Health, 2017). Learning from investigations and learning from best practice were cited as components leading to better care. In the Morecambe Bay Investigation, Dr Kirkup CBE reported ‘missed opportunities’, where future harm could have been prevented if good investigations, learning lessons, and positive action had taken place (Kirkup, 2015).
Nationally reported shortcomings
Earlier this year, the Care Quality Commission (2020) published a briefing document aimed to improve maternity safety, which highlighted ‘a lack of investigation and learning when things go wrong’. The Royal College of Obstetricians and Gynaecologists (2018) report, Each Baby Counts, highlighted significant variability in the quality of local maternity investigations, the lack of family involvement, and the tendency to blame individuals rather than fully seeking to understand and address systemic issues. When reviewing local investigations, MBRRACE-UK stated that nearly half (43%) were found to be of poor quality (Draper et al, 2017). The Better Births report called for a ‘national standardised investigation process when things go wrong’ and highlighted a lack of national training as a concern (Cumberlege, 2016).
Mind the gap
Although many organisations have worked to improve how they respond and learn from adverse events, there clearly remains a need to provide better training and support in this area.
In the Mind the Gap report, Baby Lifeline (2018) found that ‘learning from risk’ was mandatory for midwives in three-quarters of trusts (75%), but less for other staff groups; around half of trusts (52%)mandated it for obstetricians and around a third (36%) for obstetric anaesthetists. Where it was provided, it was evaluated in less than two-thirds of trusts (65%) and was mostly delivered in-house (90%). On average, the annual duration of the training was under two hours. Furthermore, what was covered as part of that training varied between trusts (Figure 1).
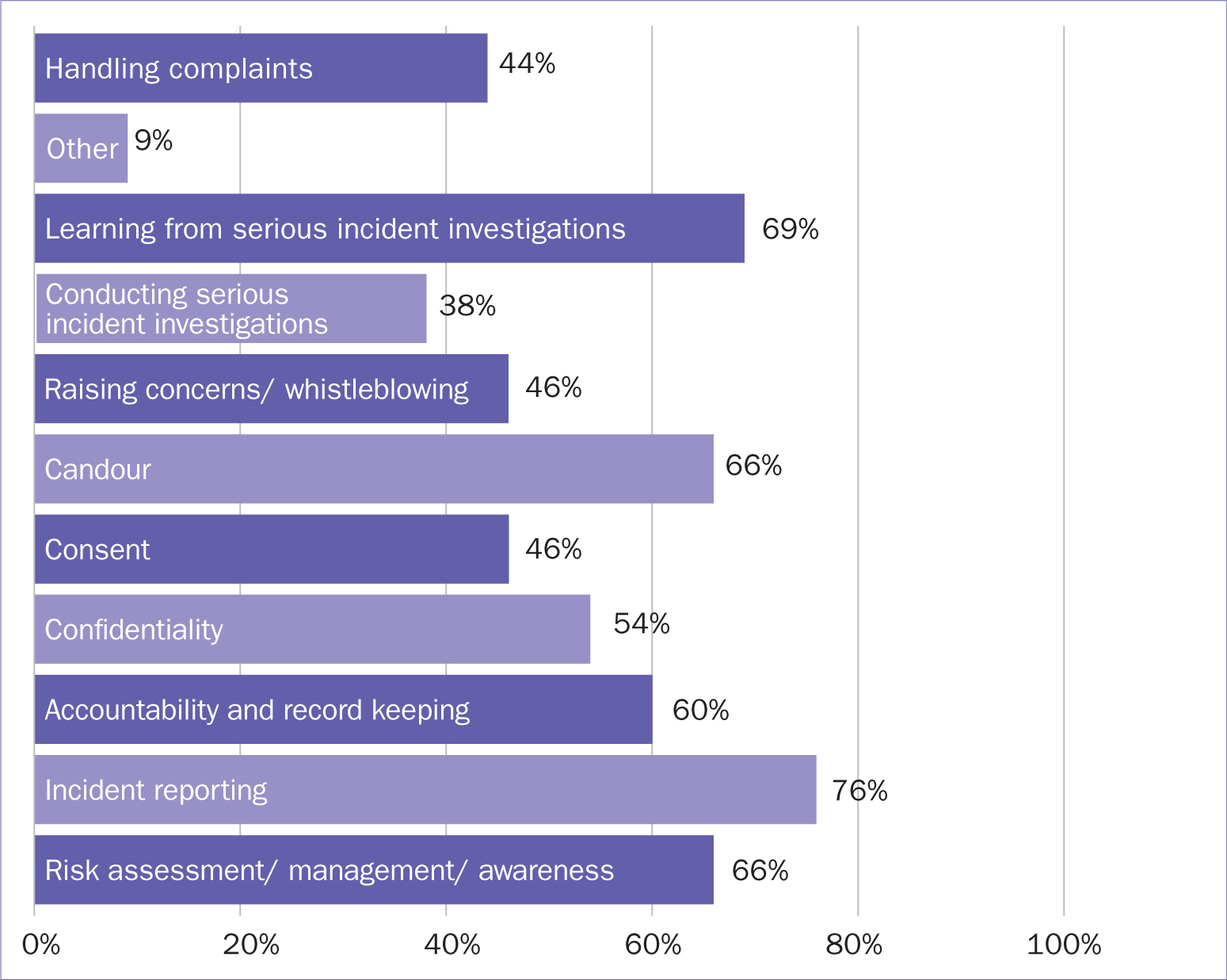 Figure 1. Reported content within learning from risk, patient experience, clinical incidents/governance, and professionalism (% of trusts).
Figure 1. Reported content within learning from risk, patient experience, clinical incidents/governance, and professionalism (% of trusts).
Baby Lifeline's response
In response, Baby Lifeline developed a two-day course: Learning from Adverse Events in Maternity Services, which was piloted in February of this year.
The course was developed with leading experts from NHS Improvement and NHS Resolution, to provide delegates with crucial training in areas where a need for improvement has been repeatedly identified, including investigation methodology and approach, family engagement, treating staff fairly in line with ‘just culture’ principles, report writing and developing effective improvement actions.
Improvements
As part of the evaluation of the training, confidence and empowerment are measured as well as delegate satisfaction.
- 97% of delegates ‘agreed’ or ‘strongly agreed’ that the course was relevant to their learning objectives
- 100% of delegates rated the quality of education good, very good, or excellent, with over half rating it as ‘excellent’
- 100% of delegates stated that the course will effectively influence their practice, with 93% stating that they intended to modify their practice in a minor or major way
- 94% of delegates stated that they ‘agreed’ or ‘strongly agreed’ that they were confident in key areas following the course; whereas, prior to it was less than two-thirds
- One delegate reported that she ‘really enjoyed this and definitely want to go back to “change” things’.
Baby Lifeline has now expanded its work in this area and developed a five-day course with Cranfield University, which will give delegates a ‘Foundation in Healthcare Incident Investigation’ from the university. In addition, it has been designed to be delivered online, in recognition of the current pandemic.
The partnership with the world-renowned ‘Safety and Accident Investigation Centre’ at the university will plug a detrimental gap in healthcare training and aims to improve how services appropriately respond to adverse events. The course will be piloted in January of next year.
‘I really enjoyed this and definitely want to go back to “change” things’
Conclusion
Learning and responding when things go wrong has been cited as a key component to improving patient safety in maternity care; however, many external investigations into poor care have found deficiencies in this area. Baby Lifeline also found that training nationally varied in its content, attendance, and evaluation. Baby Lifeline is working with specialists to plug this detrimental gap and improve how maternity services respond when things go wrong, ultimately improving patient safety.


