The first few months’ experiences of a newly qualified midwife's first post have an impact on the individual's confidence and the overall quality of the maternity service offered to the women and their families (Kitson-Reynolds, 2010, unpublished; Kitson-Reynolds et al, 2014). van der Putten (2008) describes it as a critical period when newly graduated midwives undergo significant adjustments to become effective team members in order to be accepted into an already established team (Kitson-Reynolds, 2010, unpublished). When successful, induction packages, integration to a new team and preceptorship programmes have been shown to have a positive effect on the retention of staff (Boon et al, 2005; Levett-Jones and Fitzgerald, 2005) and are a recommendation of the Midwifery 2020 report (Department of Health (DH), 2010a). The DH (2008) concluded that a ‘foundation’ preceptorship period at the start of a career would support the practitioner on the start of their novice-to-expert journey (Benner, 1984). Consequently, the DH published guidance on the development of effective preceptorship programmes for all health professionals. This publication (DH, 2010b) stated that preceptorship programmes re-assert the need for robust systems to be in place as it is recognised that the first few weeks into a new role is a time of vulnerability for the newly qualified midwife, and attrition nationally from the profession within the first 5 years is high (DH, 2010a). The Midwifery 2020 report (DH, 2010a: 8) states that there are many health-care practitioners accessing ‘well-established preceptorship schemes’ currently with benefit to both individuals and service provision.
The Centre for Workforce Intelligence (CFWI) (2013) forecast workforce for maternity services to 2016 based on 31 761 (in 2011) midwives registered on the Nursing and Midwifery Council (NMC) professional register and of these, 26 992 being employed within the NHS (Health and Social Care Information Centre, 2014), an increase of 1.6% on the previous year. There will be a requirement to utilise skill-mix further to ensure a sustainable workforce of the future (CFWI, 2013) that is fit-for-purpose and addresses deficits and recommendations highlighted in both the Francis (2013) and Willis (2015) reports and the Morecambe Bay (Kirkup, 2015) findings. Future staffing projections consider an increase in the numbers of non-registered staff over time (CFWI, 2013) thus affecting the skill mix and potential outcomes on patient safety (Freund et al, 2015). While there continues to be a political drive to ensure one-to-one care in labour by a trained midwife in a birth location of the woman's choice and suitability (DH, 2010b), employers strive to increase quality of delivery through smarter working and being economically savvy. The future may see further increases in the numbers of maternity support workers employed to undertake a greater level of responsibility, which is commensurate with the Willis (2015) recommendations. Retirement is generally flexible due to changes in the law (NHS Business Services Authority, 2011) meaning midwives may remain as part of the workforce for longer or retire and return on a part-time basis (CFWI, 2013). At the same time, higher education institutions (HEI) and local commissioners strategically consider local workforce planning (Health Education England, 2015). One implication to the changing role and workload of the midwife indicates a trend whereby increasing numbers of women, who are booking, are identified as having health risks, which may lead to higher risks through prenatal, birth and postnatal complications. This needs to be a consideration for educators especially in relation to the clinical skills required at the point of registration and beyond (Intercollegiate Maternal Critical Care Sub-Committee of the Obstetric Anaesthetist Association, 2015). All of which may have an impact on the newly qualified midwife's experience and support.
Following phenomenological research findings (Kitson-Reynolds, 2010, unpublished; Kitson-Reynolds et al, 2014) where two final interpretive themes described the meaning of ‘becoming a midwife’, a task and development group was convened with the aim of considering how the transition from student midwife to newly qualified midwife could be enhanced for all concerned. Transition to ‘becoming’ a registered midwife starts on day one of the student journey and aims to limit the crisis of reality shock (Kramer, 1974) that newly qualified midwives experience surrounding the change of responsibility upon qualification (Kitson-Reynolds, 2010, unpublished). This is a fundamental difference in concept to the DH (2008) document where it is implied that ‘becoming’ starts at the point of registration as a novice. The ‘transition project’ aims to enable newly qualified midwives to work towards post-registration competencies as they progress and achieve through their induction training and preceptorship year.
Current local education provision
In the UK, midwifery students predominantly embark on a 156-week, 3-year, preparation programme to gain graduate status as well as entry to the midwives part of the NMC professional register (NMC, 2009). Typically, year one students are locally exposed to elements of low-risk antenatal, intrapartum and postnatal care within integrated community and hospital teams, stand-alone and co-located birth centres and case-load held placements. They work alongside clinical mentors to begin to plan and deliver individualised care with women and their families. During the second year, students work within the hospital settings with a high-risk focus. Students are required to reflect on how a main hospital ward environment is managed to ensure safety by considering acuity, staffing, planning and prioritising workloads. By the end of a clinical hospital-based placement it is expected that they lead, plan and deliver care to a bay of women and their neonates while being overseen by a named mentor. Students are expected to be involved with drug rounds, taking telephone referrals and transfers as well as general telephone queries. The third year consolidates all experiences and further drives understanding of impending responsibility, autonomy, advocacy and accountability, while promoting the ‘normalisation’ of birth and improving birth outcomes (Royal College of Midwives, 2014). Undertaking and consolidating the ‘drug round’ experience as a student is expected (NMC, 2009), thus becoming more independent, confident and competent with performing this role as a newly qualified midwife.
Contextualising the ‘transition project’
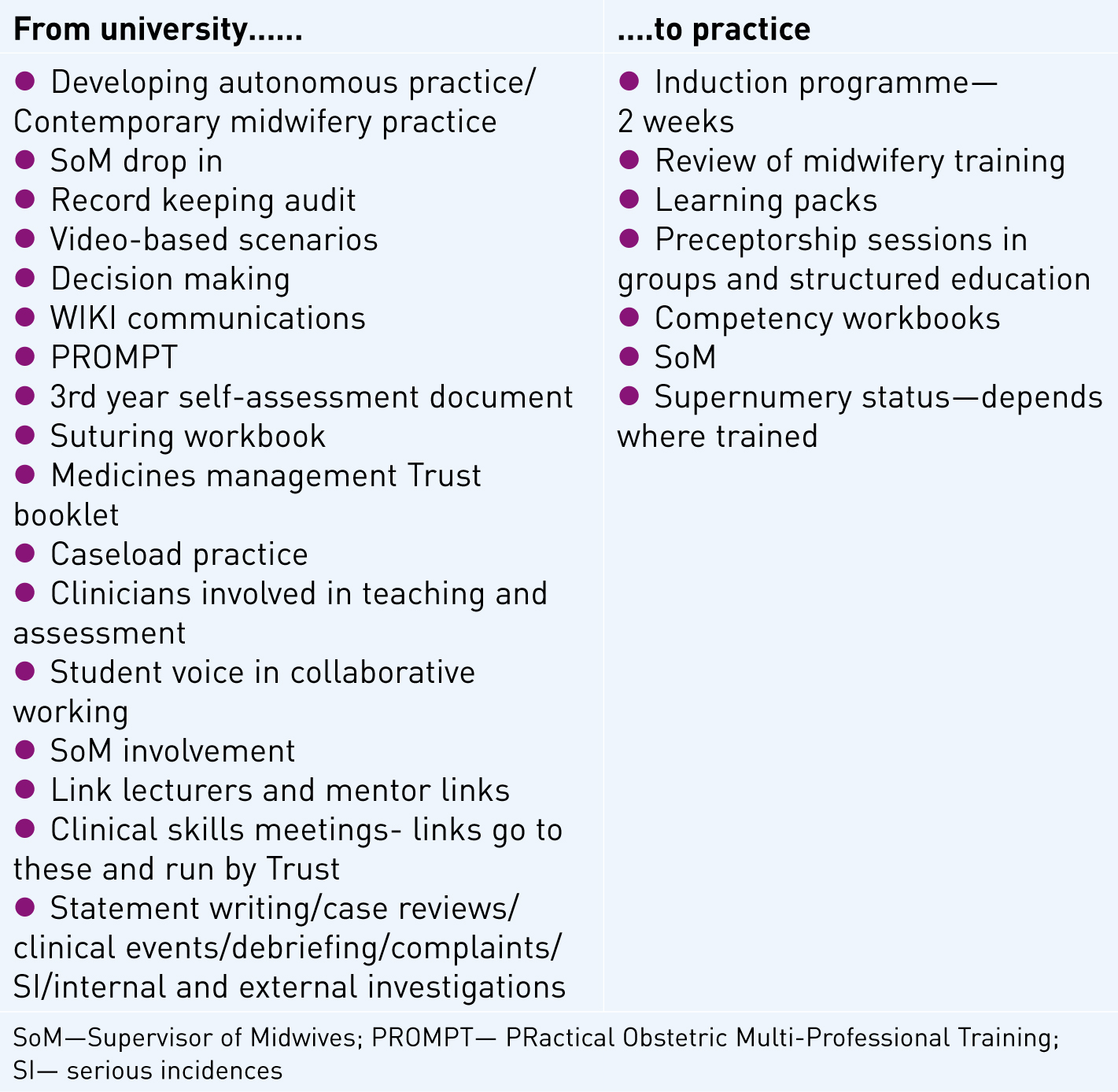
The ‘transition project’ commenced in 2005 with students developing knowledge and practical suturing skills in their third year and working towards completion of the related local Trust competency workbook for midwives. Students also work towards completion of the medicines management competency workbook in readiness for the Trust induction week; Trust conflict resolution; Trust aseptic non-touch technique (ANTT) training; case-loading experiences linked to the newly implemented University programme requirements and access to a drop-in Supervision of Midwives clinic, which introduced students to support mechanisms that midwives are afforded (Kitson-Reynolds, 2005). Over a 10-year period the activities have expanded (Figure 1) to include attendance at PRactical Obstetric Multi-Professional Training (PROMPT) training (Winter et al, 2012); a management experience and insight to roles where students have the opportunity to shadow various senior clinicians and managers throughout the Trust regardless of specialty (for example, infection prevention teams, risk management, consultants and pharmacists); care of a woman with remefentanyl; a spiral training programme linked to care of women with an epidural in situ; 1–1 record keeping supervision audits (Kitson-Reynolds and Rogers, 2011). Students are also involved in statement writing, investigations, complaints (if involved) and are supported through these processes as if qualified midwives (Kitson-Reynolds and Ferns, 2013) with named Supervisors of Midwives (SoMs). The latest inclusion surrounds data collecting for NHS Litigation Authority audits to consolidate what the students were learning in theory and to show how important service improvements linked to benchmarking and quality initiatives are for safe health outcomes. By becoming involved in such activities during the student midwife's training, the anticipation is for a seamless transition to their new role, changing responsibilities and active involvement once qualified.
Rationale
Typical demographics indicate that about 90–95% of student midwives who undertake pre-registration education and clinical practice training locally stay local on qualifying. New midwives commence employment in groups at set start dates throughout the year and access induction periods covering up to 2 weeks. This is followed by a supernumery phase prior to taking on case-loads, dependent on place and style of service provision, as soon as practicable. With this in mind, it may be more cost- and resource-effective for the service to review current practices investing in the final year students through their transitional period regardless of destination post-registration. By moving some of the induction education to the final weeks of the student midwife's clinical training programme, it is anticipated that senior students will begin to consider a gradual change of mind-set that will aid their transition to their first post. This proposal aims to shorten the induction period and release staff to commence practice earlier thus meeting the demands of the service. The cost and resource implications of releasing large numbers of staff during a short period of time, while maintaining a safe service are a challenge for most service providers. As with any change, there will always be pros and cons to such innovations.
Feedback from snap shot survey
A ‘Survey Monkey’ (SurveyMonkey, 2015) was set up for 17 newly qualified midwives who had trained and taken a first post in the local NHS Trust. Eight completed the survey answering seven questions (Table 1) that had been devised between the project lead and practice educator team within the NHS Trust. The purpose was to attain a very cursory overview of the effectiveness of the final year of midwifery preparation in terms of leading into the induction programme for newly qualified midwives employed locally and up to 1-year post-induction period. The qualitative responses have been used to modernise the induction programme along with the themes from case reviews, clinical events, debriefing etc. that are not related primarily to the newly qualified midwives performances, but from practice generically.
| Question posed | Themes from qualitative responses |
|---|---|
| Do you feel that your midwifery training supported your transition to becoming a qualified midwife? | 100% (n=8) replied yes |
| Do you feel that the developing autonomous practice module supported your transition to becoming a qualified midwife? | 75% (n=6) replied yes |
| What was the biggest difficulty you faced as a newly qualified midwife? |
|
| What was the best aspect from your training that supported your transition to becoming a qualified midwife? |
|
| If you could include anything else in your training to support your transition what would it be? |
|
| What would be your advice to the next group of students to qualify regarding transition? |
|
| Has preceptorship been a useful tool to support your new role? | Yes (n=8) |
The project development group
A task and development group was convened post-survey comprising the Midwifery Programme Lead, Supervisors of Midwives, Practice Educator for students, Labour Ward Coordinator, the Education Quality and Learning Environment Lead and latterly a Consultant Midwife. The Local NHS Foundation Trust's induction and preceptorship programme for all newly appointed midwives was reviewed to challenge preconceived ideas, assumptions, custom and practice, robustness and contemporaneousness in order to ensure the processes remained fit-for-purpose. By doing so it sought to further enhance the transition from student to newly qualified midwife. The task and development group's primary question asked if there was any aspect of the induction process that could, and/or whether it should, be brought forward and introduced to senior student midwives during their final clinical placement or earlier. The group considered the rules, regulation, Trust policy and ethics as to the need to wait for first post commencement. This would be different to the achievement of the essential skills clusters and knowledge set out and required by the NMC (2009) standards for pre-registration education and EU Directives (Directive 2013/55/EU) and not to the detriment of achieving a successful course outcome.
Further development of the project is expected to include:
In view that student midwives follow women through their care trajectory rather than being allocated to a particular clinical area, it is not until their first posts that they experience the need to understand resource management requirements. A management week will be planned into every final year student midwife's clinical placement to include the overview of daily routines and responsibilities (Figure 2) and to begin to take ‘ownership’ for that clinical environment.
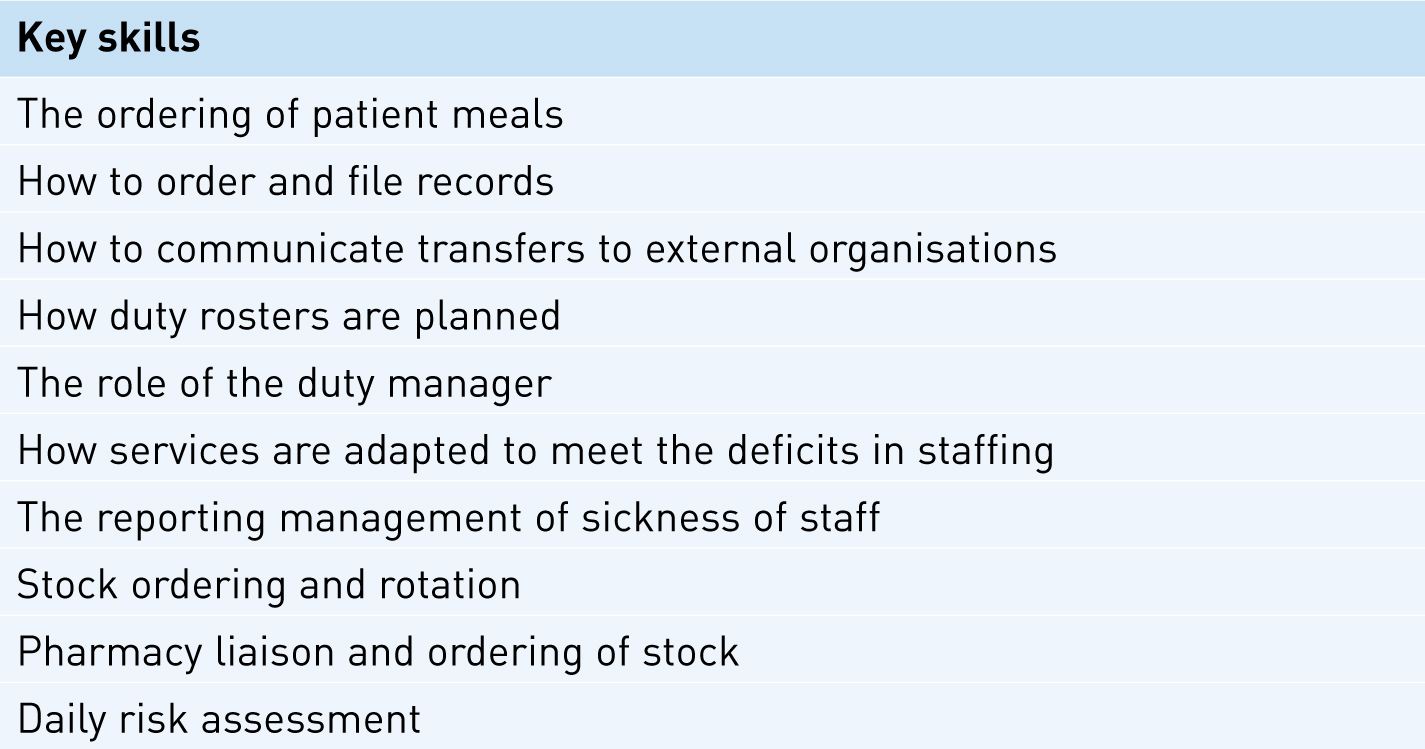
Transition passport
The task and development group set out a number of objectives, one of which was to develop a ‘passport for transition,’ which originally was planned to start on day 1 of the first year of the midwifery student training programme, but later reconsidered to commence on the first day of the third year to continue until the end of the preceptorship period. The ‘passport's’ purpose is to evidence skills and knowledge that the individual newly qualified midwife is working towards that could be mapped and transferred between NHS organisations as appropriate. The plan is for all third year student midwives to be given the passport at the start of their third year clinical placements and for the progress to be reviewed once qualified and during the induction week (to include skills from Figures 1and2). A further review will take place 3 months into their first post to monitor which competencies/skills had been achieved. At this point, the cohort of newly qualified midwives will be separated into groups of similar needs so that a tailored education programme can be instigated for individual attainment. Careful consideration has been applied so not to label groups in any way that suggests a hierarchy or competition, such as red, amber, green or 1, 2, 3 or gold, silver, bronze teams. The concept is not to create competition; however, there may be inevitable consequences to this approach and will need to be carefully reviewed so not to create a negative atmosphere.
Implications for practice
It is neither a university nor an NMC requirement to ensure midwives attain their Trust induction/preceptorship and post-registration competencies prior to qualification; this is an individual Trust issue. There is a cost to Trust induction training. This cost sits with each NHS Trust and not the HEI and consequently, one of the challenges to this project has been about who is paying for the in-house training. The counter argument has been that this is training that the Trust would be undertaking for the new employee, but it is being introduced at an earlier point in time. The risk is that all students will be offered the proposed training, but not all students will remain local for their first posts. This is an unwanted expense; however, the benefit to this is that by commencing the theoretical training while students are completing their midwifery training, any skills rehearsal with competency sign off can be commenced and achieved earlier once qualified. Alternatively, only those who have accepted first posts locally could be offered this opportunity ensuring so that financial investment remains to the benefit of the local environment, but this could be perceived as favouritism.
The second consideration is that not all new employees are from the student cohorts that have trained locally. These newly appointed midwives would then be required to have a separate induction programme, which may not be resource effective for smaller numbers. Altering the induction programme may be seen to segregate new employees rather than welcoming and integrate them into existing groups and cultures. To some extent this may already occur with those who have trained together staying together through the initial days of their preceptorship periods. It is unlikely, however, given the diverse ways of working and team allocation and the fact that newly qualified midwives proactively seek out allies throughout the service for support and reassurance (Kitson-Reynolds, 2010, unpublished). Positive cultures and values (McLean, 2012) have demonstrated inclusivity for all newly appointed practitioners especially as a change in professional roles and responsibilities appears to have a bonding effect.
There is a strong and reasonable argument for protecting the final year student midwife's time and experiences in order to consolidate their last placement requirements without them feeling pressurised into starting aspects of their newly qualified role. Students need, and deserve, to have space and time for their learning to avoid the risk of overload and work-related stress. To qualify and register, students are required to complete a portfolio of competencies as a minimum standard (NMC, 2009), which can be challenging for individuals. The introduction of the ‘passport’ and related activities aims to support induction and confidence for third year student midwives who want to commence the extra competencies/activities prior to registration and not to the detriment of their successful course completion. Anecdotally, students have requested to start extra training and skills packages to support them for their first posts and following successful clinical assessment placement sign-off. These students have primarily attained first posts locally and know which teams they are allocated to. They use the final weeks of their course in their future team, setting up their caseloads in preparation for employment with the aspiration of being fully conversant with the needs of providing holistic care for women at the point of registration. Recent students have, for example, challenged the ability to site IV cannulas, which has sparked discussions as to what is the expected role of the midwife compared to what may have traditionally be seen as an extended role. Students now receive training in their third year and are presented with the local NHS Trust training booklet to start completing through their final clinical placements and work towards being signed off as competent once qualified and Trust requirements have been achieved.
Conclusion
Potential benefits from the ‘transition project’ for the newly qualified midwife may include reducing anxiety due to role-change and a decreased workload in the induction period as skills and training are distributed out to allow for consolidation. Being an effective team member can lead to becoming accepted into the team earlier. Funding and the availability of training maybe an issue for the budget holder, but in terms of attrition, this type of innovation may save money in the long term. There is a recognised need to be able to cover the service demands safely and reduce the overload on the whole team, but this must be balanced by the support needed when newly qualified. Although this approach may be valued, one has to question if this is this about the service or consolidation of the individual, being mindful that some learn at a different pace to others.
This project is constantly evolving. New demands mean new challenges for both services and newly qualified midwives and ultimately to the benefit and safety of the women and their families that we serve.

