Diabetes is one of the most common complications of pregnancy and encompasses gestational diabetes mellitus, which is diagnosed during pregnancy; and pre-existing diabetes, which includes type 1 diabetes mellitus, type 2 diabetes mellitus and other rare specific types of diabetes (American Diabetes Association, 2011). The prevalence of type 1 and type 2 diabetes is increasing. In particular, type 2 diabetes is increasing in specific minority ethnic groups including people of African, black Caribbean, south Asian and Middle Eastern family origin (Confidential Enquiry into Maternal and Child Health (CEMACH), 2005). Approximately 87.5% of pregnancies complicated by diabetes are estimated to be due to gestational diabetes mellitus, with 7.5% being due to type 1 diabetes and the remaining 5% to type 2 diabetes (National Institute for Health and Care Excellence (NICE), 2015). In addition, there is little published evidence on the effect of diabetes in pregnancy on mental health. Although many articles have researched diabetes and pregnancy, or pregnancy and mental health, few have researched all three together.
What is diabetes?
Diabetes is a group of metabolic diseases characterised by chronic hyperglycaemia resulting from defects in insulin secretion, insulin action, or both. Metabolic abnormalities in carbohydrates, lipids, and proteins result from the importance of insulin as an anabolic hormone. These metabolic abnormalities are a consequence of low levels of insulin, which is required to achieve adequate response and/or insulin resistance of target tissues—mainly skeletal, muscles, adipose tissue, and to a lesser extent, liver—at the level of insulin receptors, signal transduction system, effector enzymes or genes (Galtier, 2010). The severity of symptoms is due to the type and duration of diabetes. Some diabetes patients, especially those with the early stages of type 2 diabetes, are asymptomatic. Others who experience marked hyperglycaemia—and especially children with absolute insulin deficiency—may suffer from polyuria, polydipsia, polyphagia, weight loss and blurred vision. Uncontrolled diabetes may lead to stupor, coma and, if not treated, death as a result of ketoacidosis or nonketotic hyperosmolar syndrome (Craig et al, 2009).
MBRRACE-UK (Knight et al, 2014) highlighted the need for improvement in care of women with pre-existing medical conditions. Nearly three-quarters of women who died between 2009–2012 had a co-existing medical condition, 3.4% of whom were women with diabetes. During this time period, three (2.8%) women died as a direct result of their diabetes. Detailed review of these deaths indicated that all women had poor glycaemic control before conception and during their pregnancy.
Women with pre-existing diabetes (type 1 or type 2) have an increased risk of adverse pregnancy outcomes, including miscarriage, fetal congenital anomalies and perinatal death. Box 1 lists contributory factors that are associated with adverse pregnancy outcomes.
As the prevalence of both type 1 and 2 diabetes in the general population is increasing, the number of women affected by diabetes in pregnancy is also increasing. In the US, gestational diabetes mellitus has increased by 56% (Ross et al, 2016).
Gestational diabetes
Gestational diabetes mellitus is usually a transient glucose intolerance that occurs during pregnancy. It can affect up to 3.5% of all pregnancies in England, but the incidence has increased in the past 20 years due to the continuous rise in overweight and obesity in women (NICE, 2015). Between 50-70% of these women will go on to develop type 2 diabetes in the first 5 years after developing gestational diabetes (NICE, 2015).
The Hyperglycemia and Adverse Pregnancy Outcomes (HAPO) study (HAPO Study Cooperative Research Group et al, 2008) examined a global population of around 25 0000 non-diabetic women and demonstrated a continuous relationship between glycaemia and adverse pregnancy outcome. The adverse pregnancy outcomes reported included primary caesarean section and birthweight. A greater association was found between maternal glucose levels at 24-32 weeks' gestation and frequency of adverse perinatal outcomes. More recently, the International Association of the Diabetes and Pregnancy Study Groups (IADPSG), has further analysed the HAPO study data and recommended revised diagnostic criteria for gestational diabetes. This is reflected in NICE (2015) guidance on management of diabetes in pregnancy. If a diagnosis of gestational diabetes is confirmed, NICE (2015) recommends a review with the joint diabetes and antenatal clinic within 1 week.
Despite improvements in treatment management in women with pre-gestational diabetes, adverse pregnancy outcomes, including large-for-gestational-age babies and preterm birth, are still frequent. The daily challenges of diabetes place significant demands on pregnant women. Even without diabetes, pregnancy can be a stressful time, with nausea, fatigue and psychosocial stress, and depression in healthy pregnant women is common (Woods, 2010). Outside pregnancy, the prevalence of depression is higher among people with diabetes than in the general population. Treating depression may improve glycaemic control for these people.
Mental illness and diabetes
Diabetes is an increasingly common health problem. Garrett and Doherty (2014) state that around one-third of people with diabetes have social and or/psychological problems that interfere with self-management. Identifying symptoms of mental health problems and meeting additional needs could help to improve overall health. Addressing the psychiatric and psychological barriers to good glucose control can help to reduce complications and improve pregnancy outcomes.
NICE (2009) addresses the treatment of depression in chronic physical health conditions—although not specifically diabetes. These guidelines adapt the stepped care model for depression, including psychological and social interventions and antidepressants. A key underlying principle is that of collaborative care, as integrating the treatment of depression with diabetes management, ideally within the same clinical team, is likely to lead to improved outcomes for both conditions (Katon, 2010).
Diabetes, pregnancy and mental health
When a woman develops depression during her pregnancy or during the postnatal period, this also has an adverse affect her baby. Depression in pregnancy is associated with poorer maternal health, increased likelihood of obstetric complications, preterm birth, and neonatal complications (Byrn and Penckofer, 2013). Postnatal depression is associated with difficulties with maternal-child bonding, inadequate care of the child, and lower rates of breastfeeding (DelRosario, 2013).
Pregnancy is a potentially stressful event that could make women with pre-existing diabetes more vulnerable to depression. Similarly, when a women develops gestational diabetes, this could contribute to depressive symptoms (Gonzalez et al, 2008). It is important to remember that depression is associated with poor diabetes self-care, which may be more challenging during pregnancy and the postnatal period, when diabetes management and glycaemic control are especially complex (American Diabetes Association, 2016). NICE (2018) sets out clear guidance for health professionals to support women and their families.
It is also important to acknowledge the woman's role in caring for her baby and to support her to do this. Women should be involved in all decisions about their care and the care of their babies. It is important that health professionals are familiar with local and national guidelines on the rights of the baby (NICE, 2018) and continuity of care for any mental health problems if care is transferred from adolescent to adult services (North West Coast Strategic Clinical Networks, 2018) (Figure 1). It is also important to remember the role of the partner, family or carer in providing support.
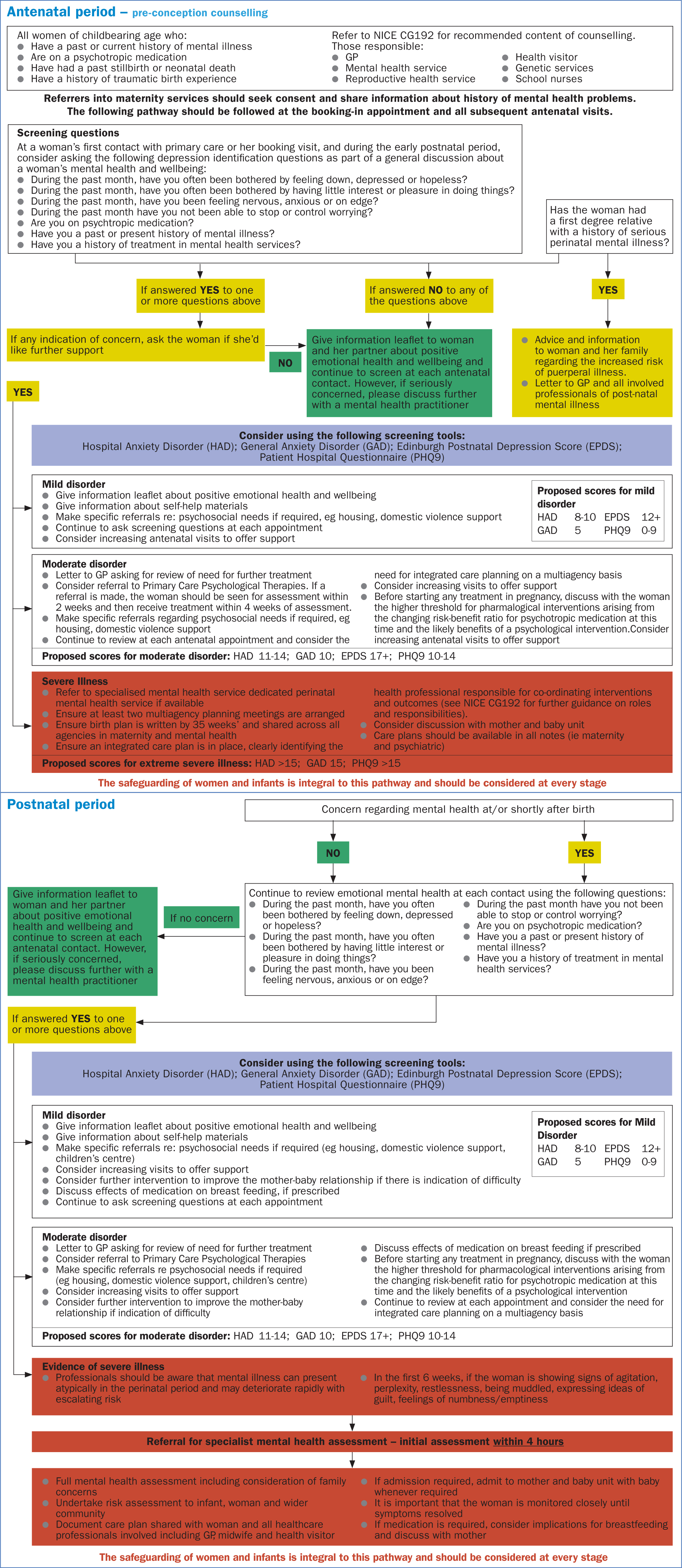
At a women's first contact with primary care or at a booking visit, consideration should be given to asking depression identification questions as part of the general discussion about a women's mental health and wellbeing.
Pregnant women who have gestational diabetes and depression are at greater risk of negative outcomes (Byrn and Penckofer, 2013). They are more likely to miss prenatal care visits, manage their diabetes poorly, ad to practise unhealthy behaviours such as smoking and alcohol use (Marcus et al, 2003). Diagnosing and treating the depression may therefore decrease the chance of comorbid complications (Byrn and Penckofer, 2013).
Treatment decisions
All women with pre-existing diabetes and those who develop gestational diabetes during pregnancy should be referred to a secondary care service. If a woman also has mental health issues, she should be referred to a specialist perinatal mental health service as soon as possible, and it is the responsibility of all health professionals who are involved in the care of a pregnant woman to signpost women to counselling or support services for mental health issues (NICE, 2018). Culturally relevant information on treatment and prevention options should be provide to the woman and her family on the pros and cons of psychological interventions and medication and the possible harms associated with treatment. It is important that the woman understands that mental health problems during pregnancy are not uncommon.
Health professionals should assess the level of contact and support needed by women with a mental health problem, and those also at risk of developing one. They should agree the level of contact and support with each woman and monitor them regularly for symptoms throughout the pregnancy and the postnatal period, particularly in the first few weeks after childbirth. Plans for monitoring symptoms should also be put in place.
Health professionals involved in the care of pregnant women should recognise that women who have mental health issues may not be willing to disclose or discuss their problem because of fears of a negative perception of them as a mother, or even that their baby may be taken from them. Other factors such as drugs and alcohol will have an impact on mental health and should also be considered. Health professionals should ensure that information is shared where appropriate, particularly when it concerns past or present mental health problems.
Women identified as high risk for mental disorders should be referred to appropriate services. This is outlined in detail in the regional pathway adapted from NICE guidelines (Figure 1) (NICE, 2018) and will be informed by Generalised Anxiety Disorder Assessment (GAD-7) and Patient Health Questionnaire (PHQ)-9 scores, and the woman's desire for onward referral. If a woman scores 9 or below on either scale she can be managed in primary care with the community midwife. If she requires consultant obstetric input for other reasons, she can be referred to any obstetrician. Self-help information should be provided and referrals should be made to address other psychosocial needs, such as housing or independent domestic abuse advisors. The woman should be screened at each contact until the end of the pregnancy.
‘Even without diabetes, pregnancy can be a stressful time, with nausea, fatigue and psychosocial stress, and depression in healthy pregnant women is common (Woods, 2010). Outside pregnancy, the prevalence of depression is higher among people with diabetes than in the general population’
Women with a score of between 10 and 14 on either scale should be referred to a consultant obstetrician with an interest in perinatal mental health. The woman's GP should be informed and a referral to a local psychological support service should be considered. Increasing the amount of antenatal contacts should also be discussed.
Women who score 15 or more on either scale should be referred to secondary care to a perinatal counselling clinic, with a simultaneous referral to the community perinatal mental health team. The community team should then screen and review the woman, and refer back into the hospital perinatal counselling clinic if the woman does not fit the criteria.
Postnatal care
The relationship between mother and baby can be difficult for some women with a mental health problem, and an assessment of the new relationship should be carried out at all postnatal contacts. Any concerns that a woman may have should be discussed and support and information provided, with further interventions to improve the new relationship considered if these are not resolved. Women who require inpatient care for a mental health issue within 12 months of childbirth should be admitted to a mother and baby unit, unless there are specific reasons not for doing so.
Conclusion
There are very few studies that have been carried out in women with diabetes and mental health issues, and this has identified the need for further research and discussion. However, the few studies that have been published have shown a significant increase in the risk of depression for pregnant women with diabetes compared to those without. Health professionals need to ensure that all women are regularly screened for depression when receiving prenatal care. Given the increasing prevalence of diabetes and depression, specific guidance for the management of women with diabetes and mental illness is warranted. Health professionals should identify, assess and offer support and treatment for women and families during this complex period.

