There is a national ambition to provide women with the power and autonomy of choice; however, the development of the concept of New Professional Management is problematic for this ideal. Understanding how a midwife's professional status contributes to women's care is important for high-quality care provision. Considering contemporary practice and reviewing midwifery professional history sufficiently enough to ask ‘why have patterns persisted?’ enables understanding of wider professional structures and reduces the focus on individual milieu (Wright Mills, 2000). Sociological imagination and knowing oneself in the context of history and politics enables the individual to recognise what is happening and to contribute to society (Wright Mills, 2000). Through exploration of the organisational, national, and professional factors that affect midwifery, in addition to what women and their family's needs are, the question ‘can a midwife achieve professional autonomy in the contemporary UK maternity system?’ is answered. This attempts to prepare midwives for future practice with a conceptual framework to support new professional midwifery and professional imagination (Wright Mills, 2000; Power, 2008).
Autonomy, choice and managerialisation
The ability to walk the tightrope between the managerial process and the needs of the individual gives value to the role of the professional and, ultimately, there is reward for the reduction of risks. Managerialism presents a major challenge to the midwifery profession as standards and outcomes are measured by policy and audit (Carvalho, 2014).
A hybridised professionalism has been identified through qualitative interviews, demonstrating the legitimisation of managerialism within traditional professional values (Carvalho, 2014) and it has been shown that an ability to control the bureaucracy furthers individual status (Faulconbridge and Muzio, 2008). This ‘organisational professionalism’ supports the notion of hybridisation. The support of organisational systems contributes to the success of individual professions. The advancement of personal midwifery success by aligning to the medical imperialised profession could be attributed to this hybridisation (Mander and Murphy-Lawless, 2013). In addition, a literature review on professionalism identified that management in the medical profession has eroded professional control (Numerato et al, 2012). The rationalisation and standardisation of healthcare can affect clinical practice, dictating the need for negation, hybridisation and strategies to support care provision. A response to this is reverse managerialisation, where managerial discourse is provided but organisational process and utilisation of guidelines are avoided in practice (Numerato et al, 2012). The hybridisation of new professional management could be argued to align with the evolution of a semi-professional role and lean toward a technocratic model where intervention in birth is seen as normative (O'Connell and Downe, 2009). This does not fit within the aims of the National Maternity Review (2016) and the direction of UK maternity care.
The pressures of working in public services with scrutiny from service users, organisations and quality assurance methods are well known and it is commonly thought that the paid professional cannot be free to utilise their autonomous powers because of the capitalist employment system (Power, 2008). The rise of a trust conflict, in part because of public demand for accountability of professionals, has been exacerbated by health scandals (Shore, 2008) and the inception of general management in healthcare originating from the Thatcher administration (Kirkpatrick et al, 2005). This demonstrates that the emphasis is on economics rather than professionalism (Sardar, 2000). The Morecombe Bay report (Kirkup, 2014) and Investigations of the Midwifery Supervision Extraordinary Review (Porch et al, 2014) provided the midwifery profession with significant challenges to its reputation and integrity. The recommendations for increased governance further contributes to ‘audit culture’ and disempowers professionals to fulfil the ideals of autonomy (Power, 2008) while increasing the ‘coercive accountability’ of both the individual and the organisation (Shore, 2008). Additionally, the Care Quality Commission (2017) compounds the proliferation of audit and risk through healthcare inspection. The Care Quality Commission's governance procedure scrutinises safety and examines ethical principles of care provision.
Facilitating evidence-based practice is central to the creation of guideline culture. Whilst guidelines provide care recommendations, their use is not essential. Guidelines align themselves with the utilitarian foundations of the best outcome for the most people (Symon, 2006) and the expectation of use is assumed (Berg et al, 2000). The intention of such guidance is to provide equal and objective care to all, which ensures transparency and parity. However, evidence-based practice illuminates the importance of individual choice as opposed to guideline adherence (Sackett et al, 1996). As a result, Berg et al (2000) describe guidelines as a double-edged sword. Compliance with guidelines support and legitimise a clinician's actions and aid the decision-making process. However, this can reduce the influence of individual circumstance. Keeping a focus on the care recipient and ensuring a shared sense of responsibility is acknowledged as good practice and correct utilisation of the guidelines. This enables the retention of clinical autonomy (Berg et al, 2000), juxtaposed with a de-professionalisation view of guidelines (Numerato et al, 2012).
Evans (2010) proposed that street-level bureaucrats can have autonomy over how they adhere to policy, but are they are criticised for this as being non-compliant with guidance. Conversely, this is proposed as being a ‘professional’ and having agency over ones decision making by Evans (2010). Arguably, street-level bureaucracy is necessitated by a shortage of time and resources, leading to those on the ‘front line’ (midwives) not being able to provide autonomy to the women they serve. However, Finlay and Sandall (2009) oppose this view by presenting the argument that a continuity of care model may provide the street-level bureaucrats that are ‘stuck in the middle’ a way to reassert and align the autonomous underpinnings of midwifery to serve both the individual women and the organisation.
The ‘dominant social values of individualism and consumerism’ (Symon, 2006) in the postmodern period have provided the benefits of technology in addition to hazards. ‘Risk society’ (Shore, 2008) reduces confidence in the natural processes of pregnancy and childbirth, and reduces midwives' autonomy and the ability to provide women with real choice (Edwards and Murphy-Lawless, 2006). Women are expected to choose the least ‘risky’ course possible and adhere to medical recommendations (Symon, 2006). Society expects conformity to the reduction of risk as the norm; therefore, in maternity the individual woman is expected to conform to this expectation (Beck, 2009). The desire to avoid being labelled immoral by not acquiescing to scientific recommendations can change a woman's mind from what she wishes to the standard care option (Edwards and Murphy-Lawless, 2006). Furthermore, social and cultural values of convenience and control increase doubt in women's belief in their own ability to birth. Thompson's (2013) qualitative study of 10 midwives' views of caring for women who have requests that sit outside of clinical guidelines and recommendations found that midwives can be uncomfortable in caring for these women. In this study, midwives expressed fear of litigation, an addition of time and resources needed to care for these women, and threats to their own autonomy and professionalism. The midwives did highlight the importance of support from coordinating midwives and medics, whilst being anxious of the response they may get initially if this was medicalised and unsupportive of women's choice (Thompson, 2013).
The role of the professional is to help the individual through their choice (Leicht, 2016) and uphold the belief of individualised informed choices, not confront individuals. However, incremental changes to the environment and professional expectations as well as institutional pressure can lead to ethical drift (Kleinman, 2006). This drift is a gradual deterioration of ethical principles that were once upheld and is detrimental to the profession, the professionals and the organisation.
The liberal professional and the bureaucratic professional are bound by ethical principles, as in the case of midwifery (Leicht, 2016). However, a professional's corporate employer is not bound by ethical codes (Leicht, 2016). The publication and visibility of the NHS Constitution (NHS, 2015) allows staff, consumers and the general public to understand the values and social purpose of the NHS. However, whether these values are upheld is difficult to police, particularly in the case of privatised organisations contracted to the NHS (Frith, 2013). The Care Quality Commision (2017) is tasked with this responsibility. Through healthcare inspection, incorporating ethical principles, the Care Quality Commission does periodically hold employers to account.
Midwifery roles and professional issues
A midwife's place of work can impact on autonomous practice because of the persisting domination of the medical model. As demonstrated in the Nilsson et al (2019) ethnographic study, midwives had doubts about their own knowledge and reduced freedom to work autonomously when on delivery suites. The midwives in the study were expected to be busy, rather than focus on the woman's needs alone. Whilst this study was completed in Sweden, some similarities with the UK system can be seen; the access to free maternity care, the dominance of the medical model, a women-centred care ethos and a long history of midwifery. However, there are restrictions on the home birth provision in comparison to the UK (Lundgren et al, 2020) which may affect the results.
The art of seeming to do nothing is a much-valued professional attribute of the midwife (Powell, 2000). This art can be described as having the ability to be vigilant and unrushed but timely, demonstrating a belief in the natural process of pregnancy, birth, and the postpartum period, without being casual, whilst providing learned judgement. Additionally, it is important to ensure necessary referral to obstetric expertise, but only when needed. This art is part of being an exemplary midwife and is important to the professionalism of midwives (Powell, 2000). In the delivery suite, the ability to provide this advocated art is challenged by the productivity insisted upon by healthcare organisations (Powell, 2000). Workplace culture challenges this further, as midwives are expected to appear busy, which reduces midwives' time with the women.
Davis and Homer (2016) conducted a study to explore how the birthplace impacts midwives in Australia and the UK. Being ‘with woman’ was found to increase a woman's calmness and the contraction hormone oxytocin, which in turn promotes successful normal birth. Whilst the principles of care were provided equally in all birth settings, the way in which this care was achieved varied. The delivery suite was felt not to be the woman's space, but the organisation's, whereas home birth was the woman's space. The feeling of being watched and conforming to the busy work of the delivery suite drew concentration away from the women. Moreover, practice that is deemed acceptable at home was considered ‘unprofessional’ in the delivery suite, for example ‘enjoying a cup of tea with the family’. Furthermore, in the delivery suite, the scrutiny of care provision and time constraints provided midwives with a sense of being rushed and a need to conform to guidelines, instead of to listen to and be guided by the woman. This was described as less safe by the research participants. These findings have been acknowledged previously by other researchers (Curtis et al, 2006). Moreover, skills in time efficiency and technological equipment use are greatly valued in the delivery suite (O'Connell and Downe, 2009), further demonstrating the value of the medical model. This contrasts with community midwives, who have reported feeling more autonomous (Sargent, 2002). Midwives within the Davis and Homer (2016) study identified that their behaviour and care approach adapted depending on the birth environment.
Midwifery leadership, senior midwifery expectations and women's expectations can lead to an acquiescence to managerialisation and medicalised care (O'Connell and Downe, 2009). Porter et al (2007) supports this bureaucratic acceptance. Interestingly, midwives place blame for this acceptance on other midwives, doctors and even women, but refrain from taking individual responsibility (O'Connell and Downe, 2009), which opposes ethical professional expectations of accountability (Nursing and Midwifery Council, 2018). Some international maternity systems facilitate autonomy of both women and midwifery. For example, 80% of women in New Zealand opt for Midwifery Lead Carers in pregnancy and childbirth, who work in collaboration with obstetricians (Skinner and Maude, 2015) and are not constrained by institutional demands, with the ability to assess risk in a social and cultural context related to the individual. Although the system can be manipulated (Skinner and Maude, 2015), it has been concluded that uncertainty should be embraced and more work into how this might be dealt with is needed.
A crisis?
The midwifery profession is at a possible point of crisis, with 67% of midwives reporting moderate work-related burnout, exacerbated by reduced NHS staffing, a lack of autonomy and organisational pressures (Hunter et al, 2019). Women's choices are affected by pre-existing values, experiences and beliefs (Coxon et al, 2017). Choices within the guidance are given by use of persuasive or permissive language (Nolan, 2010) and risk society has permeated and increased medical influence (Symon, 2006). Beck (2009) warns of an ‘apocalypse-blindness’ and society's inability to identify societal change, highlighting the possibility of self-destruction without this recognition. Yet, the audit and risk culture perpetuate because of what Beck (2009) describes as a blindness of sociology to learn and use sociological imagination and, within that, history. This is the result of the ever increasing data and a wish to perfect science. Modernisation has rendered midwives incapable of transforming within a social-historical context.
What are the alternatives? Productivity could be measured by outcomes in optimal health and the experience, empowerment and respect of the woman and her family (Powell, 2000). Professionals can influence the risk management agenda to maintain values and ideologies, ensuring cultural fragmentation does not occur (Leicht, 2016). Midwives engaging in risk discourse, attending meetings, ensuring the underpinning professional values and pillars of the Code (Nursing and Midwifery Council, 2018) underpin guidance, engaging Professional Midwifery Advocates in advocating the midwifery agenda, strengthening the maternity workforce, supporting fellow midwives in their own advocacy of women and their family's needs, and leading by demonstration and commitment of values (NHS England, 2017). Research evidence and current maternity policy provide society with an opportunity to regain individualisation and autonomy (Brocklehurst et al, 2011; National Maternity Review, 2016). Yet, Beck (2009) argues that society is incapable of fixing the problems it has created in an age of advanced modernity and rationalisation. The view that the service user's need should be prioritised over economic need is important (Freidson, 2001). A solution may be found through reflective practice and sociological imagination.
Reflective practice
Reflection is used widely in healthcare to enable practitioners to make sense of what they do, to change practice and to promote professional development (Taylor, 2010). Whilst Schon (1983) may appear a dated source, the fundamental principles presented are still applicable today. He identified the theory-practice gap and advocated for a transition from technical-rationality to professional practice based on reflection-in-action. Rather than using specialist knowledge to confer power over individuals and retain professional autonomy, the professional uses knowledge to empower the individual to acquire that same knowledge through communication and conversation. The demystification of knowledge allows individual and tailored reflective conversations and contracts to occur. Reflecting on limits and understanding that actions are interpreted differently by different people enables the professional to engage individuals and offer greater accountability (Schön, 1983).
With ongoing reflective practice and the transformations in care provision (continuity of care), as advocated by the National Maternity Review (2016), it may be possible to engage in sociological imagination, learning from history and research, to make change happen. The National Maternity Review (2016) has provided contemporary maternity care and professionals within this care with an opportunity to utilise both science (the research at hand) and the art of midwifery to affect this change. As identified by Power (2015), ‘one single approach is too inflexible’. Combined, perhaps autonomy and authority over women in midwifery care would then be relinquished, allowing for exceptions such as in crisis and emergency situations (Schön, 1983). Professionals can promote institutional change by understanding, interpreting and planning action in the interest of and on behalf of the clients they serve (Leicht, 2016).
Conceptual framework for New Professional Midwifery
To ensure that a profession survives, it should acknowledge and understand the needs of society (Freidson, 1988). The variability incurred by a professional working with others outside of their profession (midwives working with women) presents difficulties because of the changeable needs of society. However, the profession and the professional have the power to control its own functioning (Freidson, 1988). Power (2008) identifies different perspectives of professionalism. The ‘distressed professional’, identified in midwifery through the lack of decision making and bullying to conform to the medical model, and the ‘oppressed professional’, resulting from managerialisation. These perceptions, in addition to the wide availability of information, create consumers rather than care recipients. Power (2008) critiques both these perceptions as not acknowledging the wider perspectives influencing professionals. Wright Mills' (2000) ‘sociological imagination’ is supported by Power (2008). Asking relational (what is the structure of the profession and the differences in comparison to other professions?), temporal (what are the social historical position of the profession, included and excluded parties, how is it changing?) and dispositional (who is in the profession? How are they selected? What type of people are they? What affects them?) questions can afford the ability to consider both personal and societal views to enable change (Power, 2008). These ideas can be seen in the conceptual model in Figure 1.
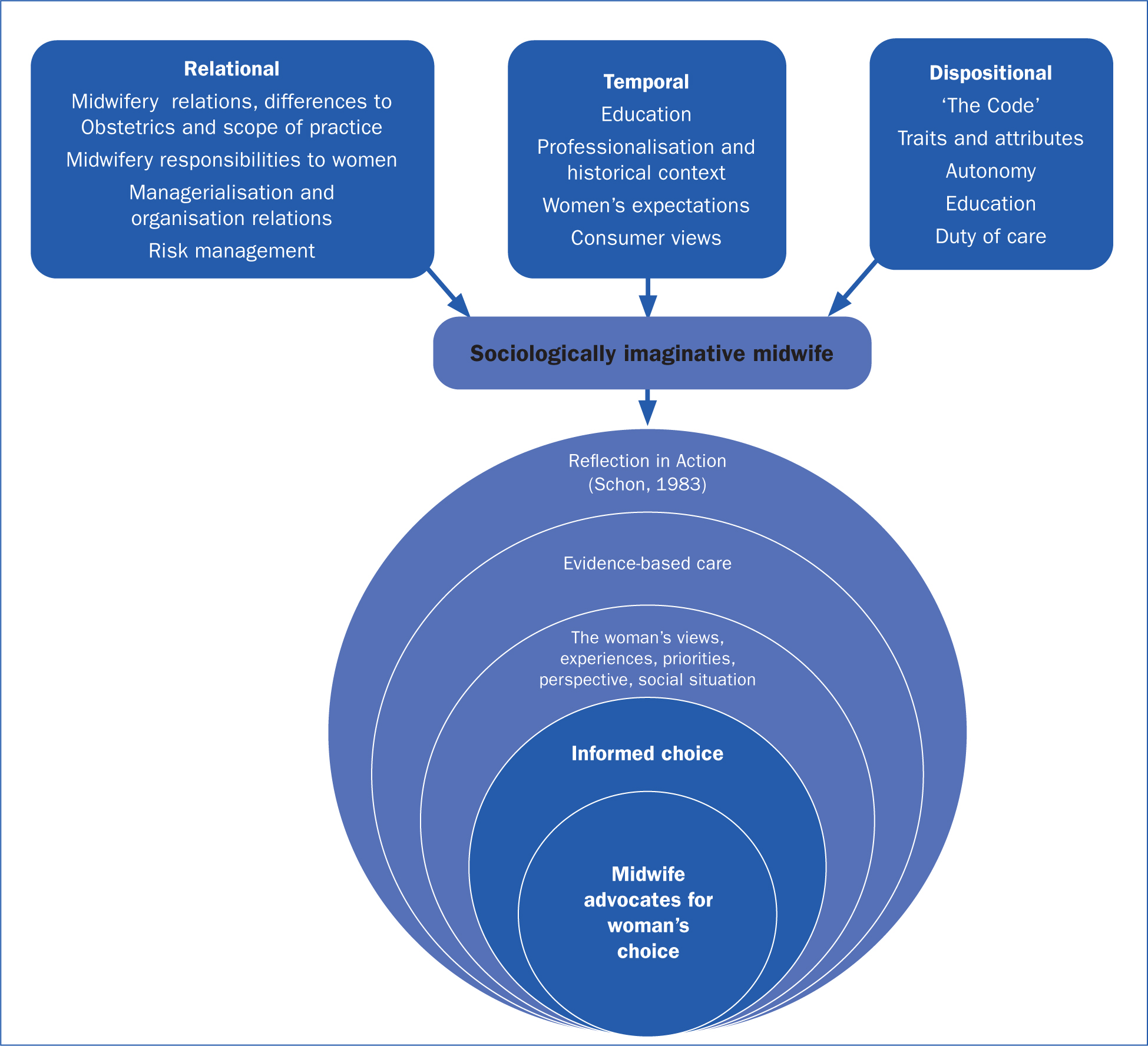 Figure 1. New Professional Midwifery: a conceptual model
Figure 1. New Professional Midwifery: a conceptual model
In addition to professional sociological imagination, the component of ‘woman’ has been considered to highlight the central aim of the midwife, to be ‘with woman’ facilitating and advocating choice and autonomy. The midwife's autonomy is therefore a conduit to woman's autonomy. ‘The Code’ (Nursing and Midwifery Council, 2018) is upheld and individualised choice and care is provided and advocated through evidence-based practice, in the context of the woman's own life, ensuring the principles of ‘Reflection in action’ are utilised (Schön 1983).
Conclusion
Can a midwife achieve professional autonomy in the contemporary UK maternity system? The answer is complex. Whilst autonomy is advocated and expected by the professional regulator (Nursing and Midwifery Council), it can be difficult to achieve. The evolving permeation of risk management and managerialisation throughout maternity services has removed, in part, the autonomous practice of many midwives, because of the fear of non-conformity and litigation. It could be argued that midwifery is in fact a ‘semi-profession’ because of this. It is a professional's duty to focus on how professional practice affects women in maternity care, as midwifery exists to serve the needs of society. If evidence-based practice, government policy, women's voices, maternity support groups and data demonstrate that midwifery practice serves society well then the professionals of the occupation have an ethical duty to ensure that the profession survives.
If women want choices, and research supports that they do, then midwives must retain autonomy to support and protect individual choice despite managerialisation. Having midwifery representation in the political and policy-making landscape, free from overly utilitarian, medicalised influence, will potentially influence risk society to ensure women's choice remains a central aspect of the quality improvement agenda. Whilst autonomy is a challenge to midwifery, working in partnership with women it can be achieved. However, risk is currently shouldered by the individual professional in their day-to-day practice. Through New Professional Midwifery and sociological imagination, relationships and partnerships with other professions and contemporary practice could shape the future for women's care and the midwifery profession.
Key points
- The Nursing and Midwifery Council code advocates the need for midwives to be autonomous
- Autonomous midwifery practice is difficult to achieve in the face of litigation, medicalisation of childbirth, managerialisation and consumerism
- Guidelines are founded on the best outcome for the most people
- Working in the public sector is pressurised
- Midwifery autonomy varies depending on clinical or home environment
- Reflection in action can help professionals instigate change
- Sociological imagination and combined with being ‘with woman’ can facilitate choice and autonomy. The midwife's autonomy is therefore a conduit to woman's autonomy.
CPD reflective questions
- How can you ensure women in your care are provided with choices?
- Do you know who is responsible for guideline management in your organisation?
- Do you feel that the ‘Conceptual framework for New Professional Midwifery’ is of use to your practice?


