While undertaking a Person-Centred Care in Practice (PCCiP) masters module, I began to reflect on relationships within maternity care. I wondered if midwifery remained as the ultimate relational, women or person-centred model. Due to the way midwifery has been shaped through obstetric authoritative knowledge, streamlining and centralising, I questioned just how person-centred relationships can be within midwifery and specifically the supervisor–supervisee relationship. I have chosen to use Kolb's (1984) model for this reflection (Figure 1).
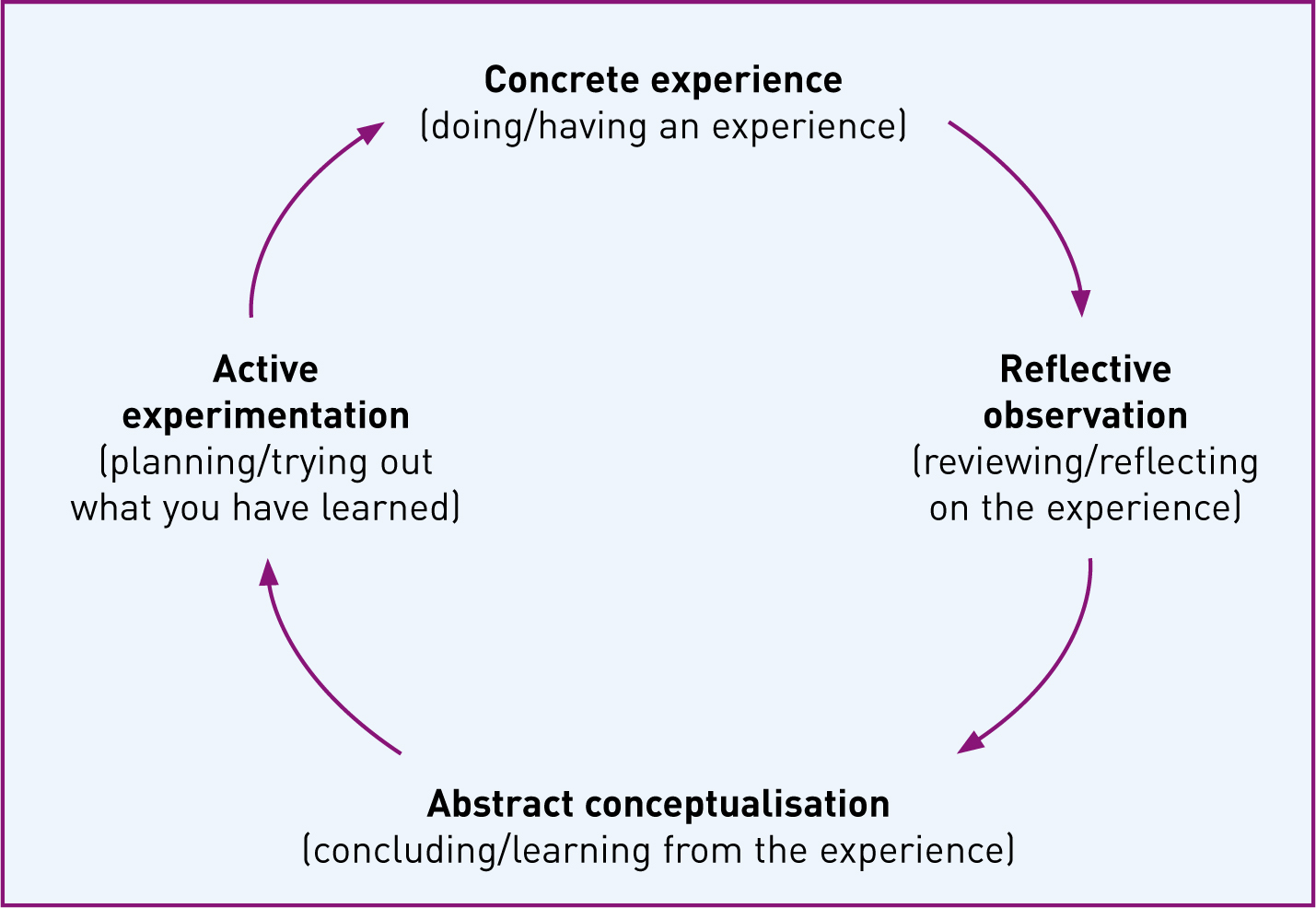
Kolb (1984) suggests that more than just an experience is needed to achieve learning: reflection, forming general opinions, and actively experimenting with concepts and processes are also required. Learning may begin at any of the four points in Kolb's cycle where it encourages the reflector to take on roles of activist, reflector, theorist and pragmatist. The aim of this paper is to critically explore supervision of midwifery through a ‘person-centred care in practice’ lens using the senses framework and concepts such as co-production and emotional labour (Table 1).
| Sense of security | To have secure conditions of employment |
| Emotional demands of work recognised | |
| To work within a supportive but challenging culture | |
| Sense of continuity | Exposure to good role models and environments of care |
| Expectations and standards of care communicated clearly and consistently | |
| Sense of belonging | To feel part of a team with a recognised and valued contribution |
| Belong to a peer group | |
| Sense of purpose | A clear set of goals to which to aspire |
| Beneficial direction | |
| Sense of significance | Practice is valued and important |
| Your work and efforts matter |
Concrete experience
Statutory supervision is a regulatory framework that was introduced in the 1902 Midwives Act. It has a long history of ensuring midwives are suitably educated and competent to remain on the Nursing and Midwifery Council (NMC) register. The current varied remit of a supervisor of midwives (SoM) includes supporting allocated midwife supervisees via annual review, monitoring standards of midwifery practice and investigating clinical incidents. Over the decades, the role and responsibilities of SoMs have evolved due to organisational, social and legislative changes to health care. Yet the fundamental function of a SoM remains—protecting mothers and babies—by underpinning and promoting good midwifery practice and offering every midwife practising in the UK a framework for guidance and support. In relation to an assets-based approach, SoMs are a community, and supervision could be seen as a resource that has protective and promoting factors, which should have the ability to enhance midwives at an individual level and the midwifery community at an organisational level (Morgan and Ziglio, 2007).
An extension of the SoM role includes offering support to, and working in partnership with, women (NMC, 2014). This is another example of supervision's potential as a health asset, promoting the individual maternity service user and the maternity service user community to be co-productive.
Historically, the majority of SoMs were also in managerial roles. The two roles were difficult to separate and define clearly with the combination being reportedly punitive and authoritative. This led the supervision framework to be seen in a negative light (Perkins, 2013). However, the NMC had a drive to raise the profile of supervision and emphasise the supportive aspect of SoMs to midwives and women and produced guidance and leaflets to promote supervision to midwives and women (NMC, 2009; 2010).
Some midwifery leaders have argued that midwives are the most suitable way of raising the profile of supervision (Barker, 2012). Midwives and SoMs must experience supervision in a positive, proactive light to be prepared to actively promote supervision.
Coinciding with this effort has been an increase in the levels of administration in supervision processes, most likely due to the high profile cases where the framework of statutory supervision has been reviewed and questioned (Francis, 2013; Parliamentary and Health Service Ombudsman (PHSO), 2013). The lack of recognition of the burden that this bureaucracy is placing on SoMs, midwives and maternity services is worrying.
Therefore, a situation where midwives and SoMs will see, and feel, supervision as reactive rather than proactive will prevail, with both groups in no place to promote the role to women and service users.
As a newly qualified SoM, I was keen to undertake the role after exploring the support aspect of supervision, not only for midwives but also for women. However, I quickly became somewhat discouraged and uncertain about the role. As a result of the recent concerns and my own observations, I began to query if the current framework was fit for purpose. In 2002, the newly-formed NMC recognised supervision as an effective model for regulation (NMC, 2002). Now in 2015, as a result of the PHSO recommendations and a review by the King's Fund, the NMC has accepted the separation of midwifery supervision and regulation (PHSO, 2013; King's Fund, 2015). This paper aims to critically evaluate the current premise of SoM through a person-centred care lens.
Observations and reflections
As part of my reflections during the ‘person-centred care in practice’ module, I have been considering the various frameworks and concepts we have explored in relation to supervision and the new domains laid out by the NMC (2014).
This reflection has offered the opportunity to explore, critique, compare and discuss each concept in depth. I have found myself considering if the current framework of supervision enables SoMs to provide support to midwives that reflects the principles of person-centred care. Could a person-centred model improve supervision for midwives, SoMs and, ultimately, women and their families? Patient care and employee care should be reflected equally in the philosophies and ethics of a health-care organisation and any authority within that which makes a contribution to services (Thompson, 2005).
Abstract conceptualisation
The framework of supervision is based in a statutory structure. The Local Supervising Authorities (LSAs) sit within an NHS authority. The LSA appoint a practising midwife as a Local Supervising Authority Midwifery Officer (LSAMO). The core functions of the LSA and LSAMO involve public protection, quality assurance and clinical effectiveness. Under the umbrella of clinical governance, the standards for the preparation and practice of SoMs are monitored by the LSAMO. Recently updated, these standards are underpinned by four domains defined by the NMC (2014). It is yet to be decided if the NMC will continue to set the standards for supervision of midwifery education although it is evident that education will need to be adapted. The four domains weave together the scope and range of midwifery practice. I have considered domain 2 (Table 2)—communication and interpersonal skills—and domain 4 (Table 3)— leadership and teamworking—in the light of the senses framework (Nolan, 2004; 2006; NMC, 2014).
| Supervisors of midwives must: |
|---|
| 1 Support and work collaboratively with midwives working with complex ethical, legal and professional issues |
| 2 Work in partnership with women and create opportunities for women to engage actively with and influence maternity service provision |
| 3 Support and work collaboratively with supervisor of midwives colleagues and members of multidisciplinary and governance teams to improve standards of care and ensure a safe service to women and their families |
| 4 Demonstrate the ability to engage with a wide variety of individuals, groups, agencies and organisations at local and national levels |
| 5 Recognise when people are anxious or in distress and respond appropriately so as to promote their wellbeing, personal safety and resolve conflict |
| 6 Use effective communication strategies and influencing skills to achieve desired outcomes, respecting the dignity and human rights of all concerned and know when to consult a third party and make referrals for advocacy, mediation or arbitration |
| Supervisors of midwives must: |
|---|
| 1 Act as a role model, apply best practice in motivation and provide visible leadership in the workplace |
| 2 Develop multidisciplinary team working which encourages mutual respect and values the contribution of all parties |
| 3 Be self aware, recognising own values, principles and assumptions |
| 4 Undertake continuing professional development in the supervision of midwives |
| 5 Appraise and modify performance as a supervisor of midwives by learning from experience, through feedback, reflection and evaluation |
| 6 Develop an understanding of the strategic and political factors which may influence the provision of maternity services |
| 7 Actively listen and provide support to women who raise concerns in relation to the care they have received and, work in partnership with members of the multidisciplinary and governance teams to investigate and respond appropriately and in a timely manner to address these concerns |
At present, supervision, through its regulatory role and its transactional leadership style, offers a reactive task-orientated transactional model of care for midwife supervisees (Maben et al, 2010). The care and support is responsive not proactive, it remains within the status quo and is compliance-focused, it does not allow true partnerships to form between midwives and SoMs. The domains are broad and could be used in a more positive light allowing elements of transformational leadership to flourish. The supervision framework does show elements of transformational leadership which is a goal it aspires to, but this is not translated into reality.
Supervision needs to encourage and develop a more prominent transformational model of leadership and care. This could evolve into a relational model of care for supervisees and women. A relational model of care understands and encompasses the person at the centre, therefore enabling learning, decision-making and self-development (Noseworthy, 2013).
On reviewing and comparing the frameworks, they are not as polarised as first expected but communicate a very different focus from what is experienced at the coalface.
By exploring models of patient-centred care I have formed a view of the style of leadership and care that I value as an individual and a health professional. This is not the dominant style in SoM. On reflection it has become clear that although supervision may attempt to adopt a relational, transformational model, it is bound by regulation and I agree that the two elements should be separated. This should allow room for a different style of supervision. Possibly a style of supervision that reflects the senses framework, that recognises and values individuals, the interrelationships and bonds that affects the lives of midwives, supervisees, SoMs and service users (Nolan, 2004).
In a climate where openness, informed decisions and, indeed, human rights of the individual are evolving to form health-care that is compassionate, person-centred and meaningful it is right that the current system of supervision is reviewed and re-modelled. Restructuring supervision based on a model that establishes relationships may be meaningful and therefore have much more success in protecting the public, improving safety and women's experiences (Hunter, 2008). Without change, the ‘perform or peril’ undercurrent of supervision may actually be burdening the midwifery profession and workforce. Any establishment of a relationship-based model may benefit from actively exploring the concept of an assets-based approach such as co-production.
Co-production is a concept of partnership, where a service provider and a service user unite and share expertise (Table 4). It recognises and values the contribution of both parties (Realpe and Wallace, 2010). By exploring the key dimensions of co-production against the SoM domains 2 and 4, the idea that midwives are best placed to promote supervision holds true (Barker, 2012; NMC, 2014). For the purpose of this analysis, midwife supervisees are the service user and supervisors of midwives are the service provider. In terms of co-production, the domains appear forward thinking. The domains recognise the relevance and importance of relationship, contribution and collaboration; however, this only achieves descriptive or intermediate level co-production (Realpe and Wallace, 2010).
| Recognising people as assets rather than as problems |
| Building on people's existing skills and resources |
| Promoting reciprocity, mutual respect and building trust |
| Building strong and supportive social networks |
| Valuing working differently, facilitating rather than delivering |
| Breaking down the divisions between service providers and service users |
Perkins (2013) suggests that the majority of midwives are unaware of the extent of the SoM role. Their perception is limited to exposure as a supervisee and therefore, they use supervision in a limited capacity. A transformational level of co-production can not be achieved with the current model of supervision as it is not being delivered effectively. Therefore, the benefits of co-production empowering frontline staff remain unexplored.
In recent years evidence has emerged of poor workforce morale and Hunter et al (2008) question if this is partly due to working within frameworks that are not relationship-focused. Hall (2013) considers evidence that shows in times of low morale, midwives withdraw further, limit exposure to meaningful relationships and focus on tasks instead. Therefore, I hypothesise that midwives are not well-placed to promote supervision.
Most of Midwives rules and standards, Supervision Standards and Domains, and The Code (NMC, 2012; 2014; 2015) actively encourage co-production at descriptive and intermediate level. Therefore, the NMC guidance could be used as a health asset, by service providers and service users. The dominant transactional model of leadership and increased bureaucracy has an inhibitive effect, among others, on the ability of supervision of midwives to build on the role of health asset and undertake co-production.
I would argue that the negative effect of a transactional leadership style, the direction of SoM strategy and the pressures executing the strategy is palpable within supervision. As a result there may be lack of cohesion, drive, creativity, community and communication. I am aware this may not be representative of all SoM teams. Although some SoMs may be suffering from the effects of the dichotomy explored in this paper, especially the service centric perspective of SoM.
The reason the current model of supervision may be self-limiting to teams, and therefore, individuals, deserves further analysis and is beyond the scope of this reflection. I would, however, like to explore emotional labour in relation to the complex and challenging role of SoM.
I interpret the concept of emotional labour within health care, a title coined by Hochchild in 1983, as the emotional impact, response or conflict experienced by a health professional during the act of caring. The contextual aspect of caring should also be recognised as this may enhance the emotional impact. Consequently, the ‘cost’ of emotional labour may be increased. Hochschild (1983) defined characteristics of a job that involves emotional learning. I suggest the third characteristic may reflect regulatory aspects of the NMC's standards and guidance for nurses and midwives. The core dimensions of the Knowledge and Skills Framework used by NHS employers create layers of control (Department of Health, 2004; NMC, 2012; 2014).
‘They allow the employer, through training and supervision, to exercise a degree of control over the emotional activities of the employee.’
Emotions are a human response to circumstances and social situations and ethical health care and leadership should recognise this (Huy, 2000; Thompson, 2005). Service providers and allied authorities, such as the LSA, should also recognise that emotions will manifest when conflict occurs between workplace, service provider, personal and professional ethics. Due to the varied tasks and responsibilities of the SoM, and the complex relationships with employers, LSA, NMC, the service and supervisees, emotional labour will be felt by SoM and may require a masking of emotions (Haycock-Stuart, 2010). The overall cost of this emotional labour and the necessary surface acting could in some way be responsible for any poor dynamics or achievements in supervision. This is not a criticism of SoMs and the self-motivated individuals who work hard. It is a critique on the impact that a combination of transactional leadership style, an outmoded model and increased regulation may have on individual or groups of SoMs.
The SoM role is voluntary and SoMs receive a token annual remuneration. I would suggest this could be interpreted as a lack of recognition and support for supervision as a framework. SoMs may perceive this to be a monetary statement that adversely reflects the value of their work and contribution, thus increasing inner conflict and enhancing emotional labour. It must also be recognised that the emotional labour expended in the role of SoM also has an impact on the substantive role undertaken by the midwife (Perkins, 2013).
Emotional labour experienced by the individual, and therefore, the team, must also be enhanced by the recent criticisms from the PHSO and the current considerable investigation processes (PHSO, 2013). Some experienced SoMs may not have had their supervisory education under the last decade's NMC standards (NMC, 2012; 2014). This could effect how they acquire knowledge and skills that allow for the demand of high-calibre, almost forensic, investigations of adverse events. Research exploring supervision found that many SoMs learn from each other through informal support and reciprocity (Richards, 2011).
The PHSO (2013) questioned how ethical the supervision process is and how objective SoMs can be when investigating their colleagues and peers.
Hunter's (2010) literature review discusses emotion work in collegial relationships. While some positive relationships exist where collegial support, teamwork and trust is salient, the article finds an overall negative view of relationships within the midwifery profession, at most levels. Although this literature review did not encompass the supervisee–supervisor relationship, these observations must be replicated in some supervisee–supervisor relationships and indeed in midwives’ relationship with, and view of, supervision as a whole.
Hunter et al (2008) equate relationship skills with the emotion management skills of midwives, suggesting both need support. They postulate that making changes to the context of care is a key solution to enhance relational, humanistic attitudes. A highly supportive workplace is required if positive relationships are to be formed (Hunter, 2010).
Research to explore the supervisee-supervisor relationship in terms of emotion work and how these can be nurtured and sustained could enhance the current or any new model of supervision.
‘When supervision works well it fosters safe, supportive and effective practice in which the ideals and identities of the midwife are respected.’
This captures the essence of holistic supervision, combining the framework's objectives with a humanistic, relational approach that values the individual midwife at the heart of it (Hall, 2013).
Active experimentation
I have briefly explored supervision by analysing and evaluating frameworks and leadership models, specifically the senses framework and two domains from the Standards of Preparation and Practice of Supervisors of Midwives (Nolan, 2006; NMC, 2014). I have examined SoM in the light of the key dimensions of co-production and considered the emotional labour of undertaking the SoM role.
A form of supervision based on the recently implemented model in Wales (Healthcare Inspectorate Wales, 2014) would allow diversification, co-production and proactive supervision. The Welsh model offers an 18-month rotation for SoMs, where they can be seconded from their substansive role and work solely as a SoM. This is being carried out to improve quality for all parties and ultimately safeguard the public.
As the PHSO's recommendations have come to fruition and regulation is to be severed from the supervision framework. I would suggest merging the NMC supervision standards and domains with the characteristics of co-production to create a new framework for SoMs. Utilising a change management model and working with organisations such as, the Scottish co-production network, could strengthen supervision in Scotland and the UK (Loeffler et al, 2013).
A possible outcome of separating regulation and supervision that should be considered could be the outright abolishment of supervision. Employers and health boards would no longer be bound by statute to support supervision. Given the choice, lack of understanding of the possible benefits of a new model of supervision and with a view to save money, NHS Health Boards may withdraw funding and agreements for time and resources to enable SoM.
Conclusion
This has been a thought provoking and somewhat revealing reflection of layers and nuances. It has enabled me to begin to understand the dilemma I have with supervision and its overall implementation. This reflection has highlighted, and confirmed that in my substantive role as a community midwife, I can be ‘me’. Due to various reasons, some discussed in this reflection, this could not be achieved in my role as a SoM.
I have concluded that the dominance of the transactional model of care offered within the supervision of midwifery framework does not lie comfortably with the transformational, relational model of care I believe in and can offer as an individual, a midwife and a health professional.
I now recognise the cost in terms of emotional labour due to the discord created by this plight, not just for me, but, for many SoMs. This reflection has allowed me to intellectualise my growing feelings of disharmony and this action has allowed me some relief. I will watch closely as midwifery supervision is discussed, reframed and hopefully sustained to become the health asset it could be.

