In recent years, birth trauma has become the focus of much perinatal research. Childbirth can be a triggering event for mothers and lead to symptoms of postnatal post-traumatic stress disorder (PTSD), including intrusive flashbacks of the birth, avoidance of hospitals or future pregnancy, or feelings of irritability, fear, guilt and shame (American Psychiatric Association [APA], 2013). A systematic review estimated postnatal PTSD prevalence to be between 4-6% (Dekel et al, 2017). However, the experience of birth trauma affects many more women who do not meet the clinical cut-off for PTSD but display symptoms of traumatic stress after birth (Ayers, 2004).
Mothers who experience obstetric complications or high levels of medical intervention during birth are more likely to present with postnatal PTSD (Adewuya et al, 2006; Andersen et al, 2012; Milosavljevic et al, 2016). However, this is not a clear and linear relationship consistently found in the literature and it is important to note that obstetric complications are not a prerequisite for a traumatic childbirth experience (Czarnocka and Slade, 2000). A birth without complications may be appraised as traumatic if the mother experiences poor quality interactions with healthcare providers, leading to a negative perception of her childbirth experience (Elmir et al, 2010; Simpson and Catling, 2016). Recent reviews of birth-related PTSD present subjective birth experiences to be a more powerful contributing factor of trauma compared to obstetric factors (Ayers et al, 2016; Dekel et al, 2017). A subjectively traumatising birth can include high levels of distress, fear for the self and/or baby, lacking control over the birth or feeling unsupported (Garthus-Niegel et al, 2013).
It is suggested that a high level of medical intervention during childbirth can be a greater risk factor for trauma symptom development when also combined with poor perception of care (Creedy et al, 2000). This suggests that the subjective experience of feeling unsupported during childbirth can be an ‘additive’ factor for birth-related PTSD in births requiring high levels of intervention. This is supported by qualitative research revealing interpersonal difficulties, such as feeling abandoned, being ignored, and lacking support, being commonly identified as women's worst ‘hotspots’ during their traumatic childbirth experience (Harris and Ayers, 2012). Conversely, a supportive birth environment can provide a protective barrier against the potentially negative impact of birth with high levels of medical intervention, particularly for women with experience of prior trauma (Ford and Ayers, 2011). Experimental research suggests that support from healthcare practitioners has greater influence over women's perception of trauma and sense of control than stressful events during the birth (Ford and Ayers, 2009). Therefore, level of support during birth is a key factor in birth-related trauma, but it is unclear whether this relationship reflects a buffering function or an additive risk factor for postnatal PTSD.
This study explored this relationship between subjective experience of birth and level of obstetric intervention, and their effect on postnatal trauma symptoms. A questionnaire was designed to assess whether feeling supported during childbirth could mediate the potentially negative impact of a birth requiring medical intervention. Free-text responses of traumatic birth experiences were included to improve the researchers' understanding of the relative weight of obstetric and subjective factors on the trauma-linked appraisals mothers make about their births.
Methods
Overview
Women who had given birth in the 12 months preceding October 2018 were invited to complete an online survey, which measured their subjective birth experience, level of obstetric intervention experienced during their most recent birth and postnatal symptoms of trauma, anxiety and depression. The survey also contained free-text response questions for women to expand on their birth experience in more detail.
Recruitment
Participants were recruited via local mother and baby groups in South West England (UK) and social media pages. A link to the survey was posted on various forums on Twitter and group pages on Facebook, including ‘Happity’. Approval from group moderators was gained prior to the study being advertised on group pages. Data were collected over a 3-month period from October–December 2018. Inclusion criteria stipulated that participants must have had their baby within the last 12 months and be more than 18 years old. A total of 222 eligible participants completed the online survey.
Data collection
The study advertisement linked directly to the online questionnaire, which was hosted on an online survey software, ‘Survey Monkey’. Upon clicking the link, participants were provided with a study brief and an online informed consent page. The survey was completed anonymously and no personal identifiable information was collected from participants. In addition to general demographic information, the survey included the following measures.
The Traumatic Event Scale (TES-B; Wijma et al, 1997). This 23-item scale measures trauma symptoms following childbirth specifically in line with the Diagnostic and Statistical Manual of Mental Disorders criteria of PTSD (APA, 2013). The scale includes items such as ‘unpleasant thoughts and images of the delivery experience force themselves on me’. Participants rate how often they experience these items, from ‘not at all’ to ‘often’. The TES-B was selected because of its specific application to childbirth-related trauma, as opposed to other trauma symptom scales that measure PTSD symptoms more generally, such as the Impact of Event Scale (Horowitz et al, 1979).
The Perception of Labour and Delivery Scale (PLDS; Bailham et al, 2004) comprises three subscales, which measure the participant's subjective experience of birth. The first consists of seven questions that relate to perceived levels of staff support, and includes items such as ‘how much did you feel that your wishes and views were listened to by staff during your labour and delivery?’. The second subscale comprises four items that relate to the perceived level of pain during labour, and the third comprises four items regarding the perceived level of fear for self and baby during birth. Participants responded on a scale of 1–10 (‘not at all’ to ‘extremely’) and analysis was conducted on total scores for each subscale. The PLDS was incorporated to determine which of the three subjective factors of the birth experience are more strongly associated with trauma symptoms.
The Intrapartum Intervention Score (IIS; Clement et al, 1999) measures the level of medical intervention experienced during birth. Women select the obstetric procedures they experienced on a 19-item list that includes forceps/ventouse delivery, episiotomy and internal monitoring. The total level of intervention was generated from the weighted sum of precalculated scores for each item. The IIS has been used in previous research to investigate the interaction between support and obstetric intervention (Ford and Ayers, 2011).
Postnatal depression was assessed using the Edinburgh Postnatal Depression Scale (EPDS; Cox et al, 1987) and anxiety was measured with the Generalised Anxiety Disorder assessment (GAD-7; Spitzer et al, 2006). In addition, women were asked to provide free-text responses to questions about their most recent pregnancy and birth.
Data analysis
The data from the quantitative measures were analysed using correlational analyses to assess the relationship between all variables, and regression analysis to measure the relationship between subjective and obstetric experiences of birth with postnatal trauma symptoms. Mediation analysis was conducted to explore the relationship between the level of intrapartum intervention and trauma symptoms, as mediated by perception of support. Confidence intervals of 95% were used and P<0.05 was considered statistically significant. The free-text response data were organised into meaningful groups and important aspects were identified.
Results
The demographic information of the participants is presented in Table 1. The majority (64%) of mothers were between 25–34 years old. This reflects the national statistics of ages of mothers giving birth in the UK in 2018–2019, 58.5% of whom fell within this age bracket (NHS Digital, 2019). The prevalence rates for caesarean sections in this sample also reflect national figures for emergency (16%) and elective caesareans (13%) (NHS Digital, 2019).
| Characteristics | Frequency, n=222 (%) |
|---|---|
| Age (years) | |
| 18–24 | 41 (18.5) |
| 25–34 | 142 (64) |
| 35–44 | 39 (17.6) |
| Marital status | |
| Single or separated | 24 (10.9) |
| Living with partner | 62 (27.9) |
| Married | 134 (60.4) |
| Parity | |
| Primiparous | 140 (63.1) |
| Multiparous | 82 (36.9) |
| Type of birth | |
| Emergency caesarean | 31 (14) |
| Elective caesarean | 21 (9.5) |
Based on the TES-B scores, 17 women (7.7%) met full DSM-IV criteria for PTSD. A further 16 women (7.2%) met partial criteria, defined as meeting at least one of the DSM-IV PTSD symptoms from each symptom group: re-experiencing, avoidance and increased arousal, with symptom duration for at least 1 month (Stein et al, 1997). As within-group numbers were small, analysis was based on total trauma symptom scores from the full sample (n=222).
Correlational analyses were used to examine the relationship between subjective experience of birth, intrapartum intervention score and postnatal experience of trauma, depression and anxiety. Table 2 presents Pearson correlations between all variables included in the analyses.
| EPDS | GAD-7 | IIS | PLDS pain | PLDS fear | PLDS support | |
|---|---|---|---|---|---|---|
| TES-B | 0.69 | 0.65 | 0.21 | 0.30 | 0.50 | –0.49 |
| EPDS | 0.77 | 0.05 | 0.21 | 0.36 | –0.32 | |
| GAD-7 | 0.01 | 0.20 | 0.39 | –0.29 | ||
| IIS | 0.29 | 0.25 | –0.29 | |||
| PLDS pain | 0.35 | –0.51 | ||||
| PLDS fear | –0.37 |
TES-B=Traumatic Event Scale, EPDS=Edinburgh Postnatal Depression Scale, GAD-7=Generalised Anxiety Disorder Assessment, IIS=Intrapartum Intervention Score, PLDS=Perception of Labour and Delivery Scale (subscales: pain, fear, support)
The scores on TES-B were significantly associated with those for postnatal depression (r=0.69, P<0.001) and anxiety (r=0.65, P<0.001). Total trauma symptom score was also associated with all three subscales from the PLDS: lower perceived support (r=–0.49, P<0.001) and greater self-reported fear (r=0.50, P<0.001) and pain (r=0.30, P<0.001). Trauma symptoms shared a positive correlation with level of obstetric intervention (IIS), although IIS was not significantly associated with either depression or anxiety.
Regression analysis was conducted to test the extent to which level of obstetric intervention and subjective experience of birth explained postnatal trauma symptoms. The results are shown in Table 3. At stage 1 of the analysis, IIS explained 4% of variance in trauma symptoms. At stage 2, the three subjective experience measures (fear, pain and support) were added. The second model accounted for 35% variance overall, a significant improvement on model 1 (adjusted R2=0.35; ΔR2=0.32; F (3, 217)=36.10, P<0.001). The results suggest that lower perceptions of support and greater fear shared independent variance with levels of trauma symptoms, over and above the perception of pain and obstetric intervention. In this second model, intervention was no longer a significant independent predictor of trauma.
| Model | Standardised beta | t | P | 95% CI | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| 1 | IIS | 0.21 | 3.12 | 0.002 | 0.04 | 0.19 |
| 2 | IIS | 0.02 | 0.25 | 0.80 | –0.06 | 0.07 |
| PLDS pain | –0.02 | –0.36 | 0.72 | –0.17 | 0.11 | |
| PLDS fear | 0.37 | 6.19 | <0.001 | 0.26 | 0.50 | |
| PLDS support | –0.36 | –5.57 | <0.001 | –0.40 | –0.19 | |
IIS=Intrapartum Intervention Score, PLDS=Perception of Labour and Delivery Scale (subscales: pain, fear and support), CI=confidence interval
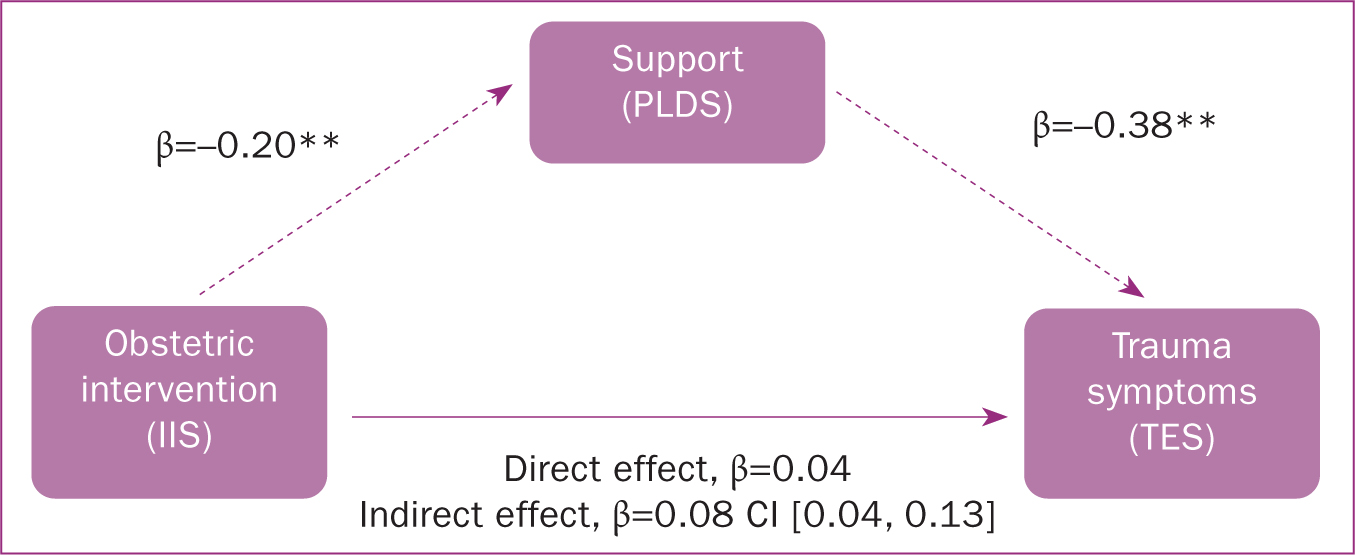
Mediation analysis using SPSS PROCESS macro version 3.3 (Hayes, 2017) tested whether feeling supported mediated the relationship between obstetric intervention and postnatal trauma. Figure 1 presents the mediation model with unstandardised beta coefficients for the pathways between intervention, support and trauma symptoms. A significant negative indirect effect of intervention on trauma symptoms via perceived support was observed, β=0.08; 95% CI (0.04, 0.13).
Free-text responses
As part of the survey, women were asked whether they experienced complications during the birth, as well as whether they considered their birth to have been traumatic. Responding ‘yes’ opened a text field inviting women to expand on their answers. Overall, 79 women (36%) reported to have experienced complications during their birth and almost half of these women also stated that they found their birth to have been traumatic (n=39). In total, 64 women (29%) reported their birth experience as traumatic, 39% of whom did not report experiencing obstetric complications. Organising the free-text response data revealed five meaningful aspects of women's experience of traumatic birth: obstetric factors, lack of control, concern for baby, psychological trauma, and lack of support (Figure 2).
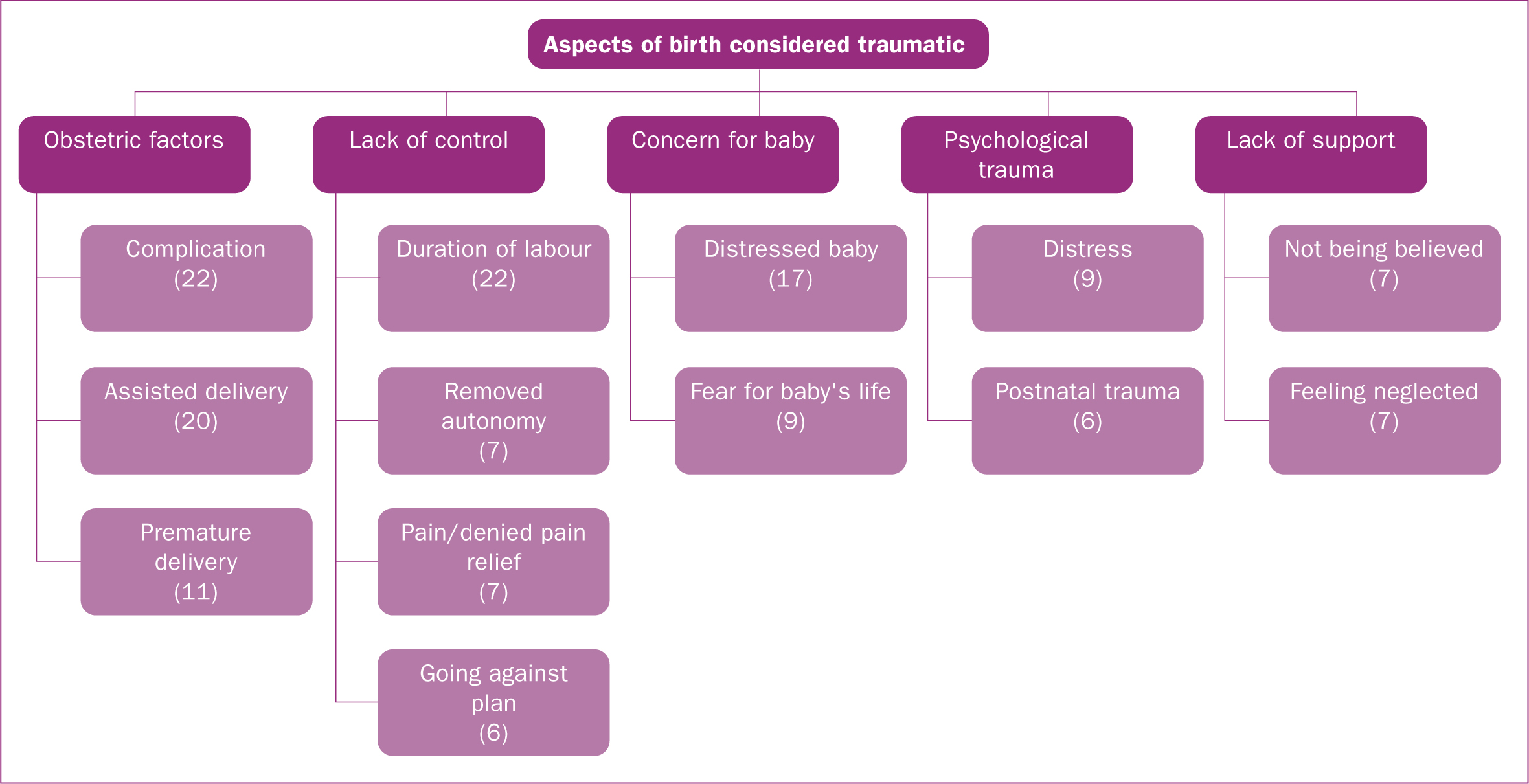
Obstetric factors
The first aspect comprised comments of women's obstetric experience. Obstetric complications, such as haemorrhage, tearing or infection, were commonly reported (n=22). A total of 20 women reported an assisted delivery in their accounts of the most traumatic aspects of their birth, and 11 women identified premature birth in their accounts.
‘Baby wouldn't come despite forceps so had an emergency section, which I wasn't expecting’
Lack of control
The most common aspect relating to the perception of the birth experience that was unrelated to obstetric factors surrounded the mother's perceived lack of control. Overall, 22 of the survey responses contained accounts of the duration of labour. This was in the context of either feeling it was too quick (n=11) or too long (n=11). Women's accounts that identified experiencing a lack of control resulting from not having a choice about the events surrounding their birth were categorised as ‘removed autonomy’. This was in the context of too many doctors in the birthing room, not having the freedom to give birth in the desired position or not being asked consent for internal examinations. Six women specifically reported that their birth experience did not adhere to their expectations or birth plan and these were categorised as ‘going against plan’.
‘People flooded the room while I was pushing and I didn't know why. Found out afterwards it was because baby's heart rate dropped’
Finally, within this aspect were women's accounts relating to pain, which was either in the context of experiencing overbearing pain (n=3) or being denied pain relief (n=4).
Concern for Baby
A total of 17 mothers related their traumatic birth experience to factors surrounding the perceived health of their baby, based predominantly on signs of physical distress or fears for their baby's life.
‘I didn't know how my baby would deliver or if she would be alive’
Psychological trauma
Overall, nine mothers explicitly reported feelings of distress associated with high stress or panic. Additionally, six women described persistent trauma symptoms resulting from their birth experience, one of which referred to her partner experiencing postnatal trauma from the birth.
‘Yes I still find it traumatic and am very concerned about having another baby due to this’
Lack of support
Women's perceptions of lack of support corresponded to either not being believed about the progress of their labour (n=7) or feeling neglected and disregarded by healthcare professionals (n=7). Within this, five women reported a lack of information about what was happening to them and two women discussed feeling abandoned during birth.
‘Very rushed c section and not told about it till last minute’
‘Was supposed to be a home birth. Was at 10cm already by the time the midwives came because I didn't “sound in labour”. Midwife told me to stop making noise and focus on pushing (already was!). Blue lighted to hospital, baby was back to back with shoulder dystocia’
Discussion
This study provides further evidence that childbirth can be a traumatic experience for many women. Obstetric interventions during birth are an important factor for the development of postnatal trauma symptoms, but the correlational data suggest this may be less significant for postnatal depression or anxiety.
Principally, these findings support the theory that feeling supported during labour and birth evokes greater influence over postnatal trauma symptoms than the level of medical intervention experienced. This is in line with recent reviews of risk factors for birth-related trauma, which present subjective experience to be a stronger predictor of trauma than obstetric experience (Ayers et al, 2016, Dekel et al, 2017).
The novel finding from this research illustrates the relationship between these factors, presenting one of full mediation. The mediation model suggests that a positive and supportive birth experience can negate the potentially negative traumatic effects from the need for medical intervention during birth and therefore serves a protective function. The model ofers an alternative perspective that runs parallel to previously documented models, which suggest that poor perceived maternity care has an additive effect on the relationship between obstetric intervention and trauma symptoms (Creedy et al, 2000). The mediation model reflects previous longitudinal research that also presents a ‘buffering effect’ of a supportive birth environment (Ford and Ayers, 2011). The similarities in the pattern of findings between these two studies demonstrate the positive and protective impact a supportive environment can have on the mother, which continues to present after almost a decade of perinatal research. This supports the assumption that obstetric complications may contribute to the appraisal of childbirth as traumatic, but subjective factors play a mediating role in the development of birth-related PTSD (Olde et al, 2006).
The inclusion of free-text responses used in this study allows further exploration into mothers' accounts of factors surrounding the birth that contributed to a traumatic experience. Over half of the women who experienced birth complications did not appraise their birth as traumatic, suggesting an objectively difficult birth alone does not guarantee a traumatic experience for the mother. The aspects derived from women's appraisals of their traumatic birth experience supplement the quantitative questionnaire data presenting an interplay between mother's perception of her birth and the objective complications she experienced. A perceived lack of control was identified as a pertinent factor that often succeeded women's accounts of obstetric complications or reports of feeling unsupported. However, it is also important to note that a significant proportion of mothers' accounts did not contain a reference to an obstetric complication and instead focuseded on the perception of her birth experience/environment as being traumatic. The majority of these cases refer to incidents of fearing for the baby, feeling ignored by healthcare professionals or feeling rushed. These aspects reflect the interpersonal difficulties identified as ‘hotspots’ of traumatic birth experiences in previous qualitative research (Harris and Ayers, 2012) and emphasise the importance of a supportive environment that encourages a sense of autonomy during childbirth, to ameliorate fear and buffer against postnatal trauma symptoms.
Strengths and limitations
This survey was completed online by a large cohort of women who were up to one year postpartum. The use of online research allows access to a larger and broader sample of mothers, yet also succumbs to methodological flaws associated with internet studies. Mothers recruited online are more likely to report greater PTSD symptoms compared to community samples of women recruited from hospitals or antenatal clinics (Ayers et al, 2015). As this study was retrospective, the possibility of women presenting PTSD symptoms from previous trauma unrelated to the birth experience cannot be ruled out. Future research would benefit from a longitudinal design to assess PTSD symptoms antenatally and childbirth-specific PTSD symptoms during the postnatal period. The City Birth Trauma Scale (Ayers et al, 2018) offers a useful alternative to measure childbirth-specific PTSD symptoms, in alignment with the revised DSM-5 criteria for PTSD.
Conclusions
This study reinforces the value of supportive healthcare professionals and the power of a nurturing environment, which can buffer the potentially negative effects of an obstetrically complicated birth on postnatal trauma symptoms. The analysis of the free-text comments illustrates the diversity of experiences that can be perceived as being traumatic during birth, many of which do not rely on objective complications. These findings, alongside previous research in this field, continue to demonstrate the significance of a positive and supportive childbirth experience particularly where obstetric intervention is required.


