Maternal obesity (a body mass index (BMI) of 30kg/m2 or higher at the first antenatal consultation) is a key modifiable risk factor in pregnancy. The health problems linked to maternal BMI for both mother and baby are substantial and well-known to midwives (Catalano and Ehrenberg, 2006), but the UK prevalence of antenatal obesity in 2006 was 18.5% and this figure only seems to be increasing year-on-year (Heslehurst et al, 2010). Inevitably, this puts more pressure on squeezed health services, with health-care costs estimated to be 37% higher among obese women compared to those with a normal weight (Morgan et al, 2014).
In addition, finding the ‘right recipe’ of support and lifestyle advice can be somewhat challenging. In terms of reducing risk factors through healthy eating and physical activity, in one Australian nutrition study, only 7% and 13% of mothers reported consuming the recommended portions of vegetables and fruit, respectively, per day and, in total, 12% consumed more than two takeaways per week (Wen et al, 2010). In an analysis of population survey data, 60% of pregnant women reported engaging in no leisure time physical activity (Hesketh and Evenson, 2016).
Although there are no UK recommendations for gestational weight gain, the National Institute for Clinical Excellence (NICE) (2010) advises that professionals weigh women, discuss the risks of high BMI in general, give advice about diet and physical activity and refer women to a dietician or other appropriately trained individual. American Congress of Obstetricians and Gynecologists (ACOG) guidelines recommend that women with an uncomplicated pregnancy exercise for 20-30 minutes most days of the week (ACOG, 2015). However, midwives report lacking the time, skills and confidence to raise the often sensitive issue of weight with women during antenatal appointments and to provide ongoing support for diet and physical activity (Foster and Hirst, 2014; Furness et al, 2015).
In observations of antenatal appointments where diet and physical activity were discussed with women, researchers concluded that there were large variations in midwife behaviour change skill levels, with many setting behaviour change goals for women which lacked specificity and relevance (Brown et al, 2013).
Encouragingly, pregnancy may be a time when women are particularly motivated to make changes to their healthy eating and physical activity behaviours (Phelan, 2010; Smith et al, 2014) and evidence is accumulating surrounding what support may be most helpful. One systematic review of 44 randomised controlled trials of healthy lifestyle programmes for pregnant women suggested such programmes could have positive effects, reducing maternal weight gain, risk of preeclampsia and shoulder dystocia (Thangaratinam et al, 2012).
Dietary interventions that included a balanced diet and maintenance of a food diary were found to be most effective in reducing weight gain and associated clinical complications. However, the authors note several reasons for the finding, such as better participant adherence to diet than to physical activity recommendations, suggesting that well-designed physical activity and other lifestyle interventions should not be ruled out. Another systematic review, focusing on 14 physical activity interventions, found that using certain behaviour change techniques could reduce the common decline in physical activity during pregnancy (Currie et al, 2013).
Core elements of interventions to support obese antenatal women have included social support (Smith et al, 2014) and behaviour change techniques including self-monitoring, setting behavioural goals and receiving feedback (Gardner et al, 2011). However, researchers point out that the majority of interventions have not been informed by theory, a factor which has ben shown to be less effective (Albaracci et al, 2005).
This is because they enable interventions to be targeted at the constructs (e.g. attitudes or self-efficacy) which cause behaviour (Michie and Prestwich, 2010). Furthermore, the lack of detailed reporting of intervention content has prevented an accurate assessment of their most effective ingredients (Gardner et al, 2011). Specifying the theory-informed intervention content according to an available taxonomy of behaviour change such as Michie et al's (2013) Behaviour Change Technique Taxonomy (version 1) would enable replication and assist in identifying the mechanisms by which behaviour is changed.
As part of taking forward Scotland's Improving Maternal Infant and Nutrition: Framework for Action (Scottish Government, 2011) several health boards in Scotland have introduced dedicated lifestyle programmes to support antenatal women who are obese. This article reports the efforts of a team of midwives, health psychologists, dieticians and physiotherapists in one such health board to develop and pilot such an evidence-based programme called Bump Start.
The aim is to support antenatal women with a BMI of over 30kg/m2 to make healthy changes to diet and physical activity during pregnancy, to ultimately reduce gestational weight gain and risk of obesity-related complications. Given this is a small ongoing pilot, results presented are preliminary, and the study aims to highlight factors that went well and challenges experienced, to share learning with other teams.
Bump Start programme methods
This section includes the development of the Bump Start intervention through a thorough scoping exercise, and Bump Start's design, participants, intervention content and procedures, measurement and analysis of initial pilot data.
Scoping exercise
To inform our programme development, a health psychologist led a comprehensive scoping exercise. It included conducting 27 questionnaires with postnatal women, designed to assess what type of support women would have liked to receive during their pregnancy. A focus group was also conducted with around 15 pregnant women at an NHS antenatal class. The psychologist held informal conversations with antenatal and postnatal women at Homestart mother and baby groups to gain a wide variety of views from women across the sociodemographic spectrum. Additionally, published and grey literature was reviewed to explore the content and effectiveness of interventions to support overweight and obese pregnant women, including guidelines for development of programmes and appraisal of existing programmes piloted in the local health board area. Finally, meetings were held to consult with a range of colleagues (including health psychologists, hospital and community midwives, dieticians, health improvement coordinators, health visitors, infant nutrition coordinator, health walk leader, and a practice education facilitator) to gather expert views on the intervention's development.
Two health psychologists analysed questionnaires, meeting, literature review and observation notes, and focus group audio recordings using framework analysis (Creswell, 2009) to apply a psychological model of behaviour change to understand psychological drivers of healthy behaviour change. The ‘capability, opportunity, motivation and behaviour’ model (COM-B) is itself part of a wider framework for intervention design called the behaviour change wheel (Michie et al, 2011), and is an intervention development approach increasingly being used to design effective health behaviour change interventions (Handley et al, 2015). The COM-B model suggests that to perform any behaviour, an individual must have:
The scoping exercise suggested that all three psychological determinants of healthy living may be important targets of Bump Start, and so techniques to build motivation, capability and opportunities to make healthy changes would all be relevant.

Furthermore, consensus was gathered from guidelines, evidence and the women that the focus of the intervention should be on diet and physical activity but should be holistic, involve relaxation, ‘feeling good’ during the exciting time of pregnancy and ‘giving baby the best start’, rather than an excessive drive on weight loss which was seen as off-putting and pressurised. The scoping exercise determined that a group programme would foster support and encourage women to self-manage over the longer-term. Finally, a multi-disciplinary team (MDT) approach, a community setting and evening delivery of the programme, and use of wearable technology were seen as important and attractive features. Women stressed that self-reported measures would need to be short and quick to complete. This scoping exercise was invaluable in informing the design and content of the antenatal programme. Results were presented to the local public health maternity steering group who agreed to provide a small amount of funding to pilot the programme.
Design
‘Bump Start’ was designed as six weekly sessions followed by four monthly follow-up sessions for consolidation, of 1.5 hours each. Sessions were held on a weekday evening in a local community room located within a supermarket, in a medium-sized town in north east Scotland, and focused on three areas of lifestyle behaviour change: healthy eating, physical activity and stress reduction.
Participants
Between February and March 2016, 18 women who would be between 16 and 25 weeks pregnant in May (the start of the programme) were approached by their midwife during a routine antenatal appointment. They were told about the programme and asked for permission for the lead programme midwife to telephone them. The lead midwife called each consenting woman to explain the programme's aims, design and content as well as provide information about the practical details of each session. Of the 11 women invited, 10 participated in the first Bump Start group. Exclusion criteria included a BMI below 30kg/m2; a severe and chronic mental health problem; being considered at high risk of miscarriage by their midwife; or having a health problem managed by restriction of physical activity.
Intervention
The sessions were designed by the health improvement midwife and health psychologist in conjunction with dieticians, physiotherapists and a midwife specialising in stress reduction and relaxation during pregnancy. A launch session engaged participants in the programme through introductory activities, introduced participants to a Fitbit pedometer and included incentives, donated by local organisations and businesses (e.g. fruit and vegetables and beauty products) as well as collecting baseline behavioural data. The six main sessions and four follow-up sessions covered different aspects of making changes in the three lifestyle behaviours and included several key behaviour change techniques, such as setting and reviewing SMART goals (specific, measurable, achievable, relevant, timed), and monitoring activity levels through the pedometer.
As indicated from the scoping exercise, main session content was embedded within the COM-B model (Michie et al, 2011). Using the behaviour change wheel approach (Michie et al, 2014), the team chose from a range of desirable behaviour change techniques (BCTs) indicated by the scoping exercise, which would map onto each factor (Table 1), including those targeting capability, opportunity and motivation to change diet and physical activity behaviours.
| Session | Topic | Delivered by | Session activities | COM-B aspect targeted and main behaviour change techniques (BCTs) and labels (Michie et al, 2013) |
|---|---|---|---|---|
| Session 1 | Launch session | Health improvement midwife and health psychologist | Introductions; summary and aims of programme; provide Fitbit pedometer and incentives |
Opportunity; Motivation
|
| Session 2 | Physical activity | Health improvement midwife and physiotherapist | Group discussion; practice pregnancy friendly exercises; goal setting |
Capability; Opportunity; Motivation
|
| Session 3 | Healthy eating | Health improvement midwife and dietician | Review goals; group discussion; myth busting exercise; caffeine guessing game; portion size and food labels exercise; goal setting |
Capability; Opportunity; Motivation
|
| Session 4 | Relaxation | Health improvement midwife & specialist midwife | Review goals; group discussion; practice relaxation; goal setting |
Capability; Opportunity; Motivation
|
| Session 5 | Physical activity | Health improvement midwife and physiotherapist | Review goals; group discussion; practice pregnancy friendly activities; goal setting |
Capability; Opportunity; Motivation
|
| Session 6 | Healthy eating | Health improvement midwife and dietician | Review goals; meal planning exercise; hunger scale and snacking; fats and sugar game; goal setting |
Capability; Opportunity; Motivation
|
| Session 7 | Review | Health improvement midwife and health psychologist | Review goals; summary; problem solving game; quiz; prizes; goal setting | Capability; Opportunity; Motivation 9,1 Credible source; 1.5 Review behaviour goals; 1.4 Action planning; 1.2 Problem solving; 3.1 Social support (unspecified); 10.2 Material reward (behaviour) |
The sessions were designed to be as interactive as possible, with group tasks to enable women to get to know and gain support from each other while learning knowledge and skills to enable them to make lifestyle behaviour changes. Table 1 provides more information on the key session content; the type of health professional delivering the session; and the BCTs utilised, from the BCT Taxonomy v1 (Michie et al, 2013), a comprehensive taxonomy of techniques. These were also tailored to individuals' goals and progress, and their relationship to the COM-B behaviour change framework (Michie et al, 2011). Participants were provided with a workbook, outlining the key session content with space to write down reflections and weekly goals (available on request).
Measures
Participants were asked to complete measures at baseline (launch night), at end of the main programme (6 weeks) and follow-up (4 months post-intervention) for the subset of women who attended the final follow-up session. Further follow-up data collection is planned for May 2017, 12 months following baseline.
Physical activity was measured in two ways: using steps recorded through a Fitbit (a three-axis accelerometer increasingly used in mHealth studies) and by self-report, using the Global Physical Activity Questionnaire (Armstrong and Bull, 2006). This self-report measure of physical activity has been widely validated (Bull et al, 2009; Cleland et al, 2014) and applied to pregnant women (Hesketh and Evenson, 2016). Participants recorded weekly steps using their Fitbit at baseline, 6 weeks and 4 months follow-up. In the measure, vigorous intensity activity is explained as ‘activity that causes large increases in breathing or heart rate’ and moderate intensity as ‘activity that causes small increases in breathing or heart rate’.
We operationalised the ACOG guidelines of 20-30 minutes of activity most days of the week to mean that participants met the guidelines if they reported ≥100 minutes of moderate or vigorous leisure time activity or active transport per week (e.g. 20 minutes on 5 days), following Hesketh and Evenson (2016).
Diet was measured using the 5-a-day Community Evaluation Tool (Richardson et al, 2011), which is a practical and valid measure with strong correlations with other measures, such as food diaries, with reduced participant burden. Fruit and vegetable intake (portions in the past 24 hours) was the main dietary outcome since it is a key indicator of overall healthy diet (Guenther et al, 2007; Moore, 2015). Additionally, a 30-minute focus group with seven Bump Start participants was conducted following the final session, facilitated by one of the team whom the participants had not previously met (EB), to explore participants' views of the programme and its effective and ineffective components. Key themes were analysed using thematic analysis (Braun and Clarke, 2006).
Analysis
Data were analysed mainly through descriptive statistics. Given the small sample size and the initial nature of the findings, inferential statistical testing was only applied to help to explore the 6 week data without inferring too much information from these findings. Paired samples tests were conducted using SPSS software (version 16) to explore statistically significant pre-post differences for participants with complete data. The 4 month follow-up data had such a small sample size that only descriptive data were included.
Results of Bump Start
Participants
Ten participants started on week 1 of the programme; two participants dropped out of the programme due to illness. Attendance was strong (at least 70%) until the last two follow-up sessions, when several women were due or delivering. Figure 1 shows attendance patterns.
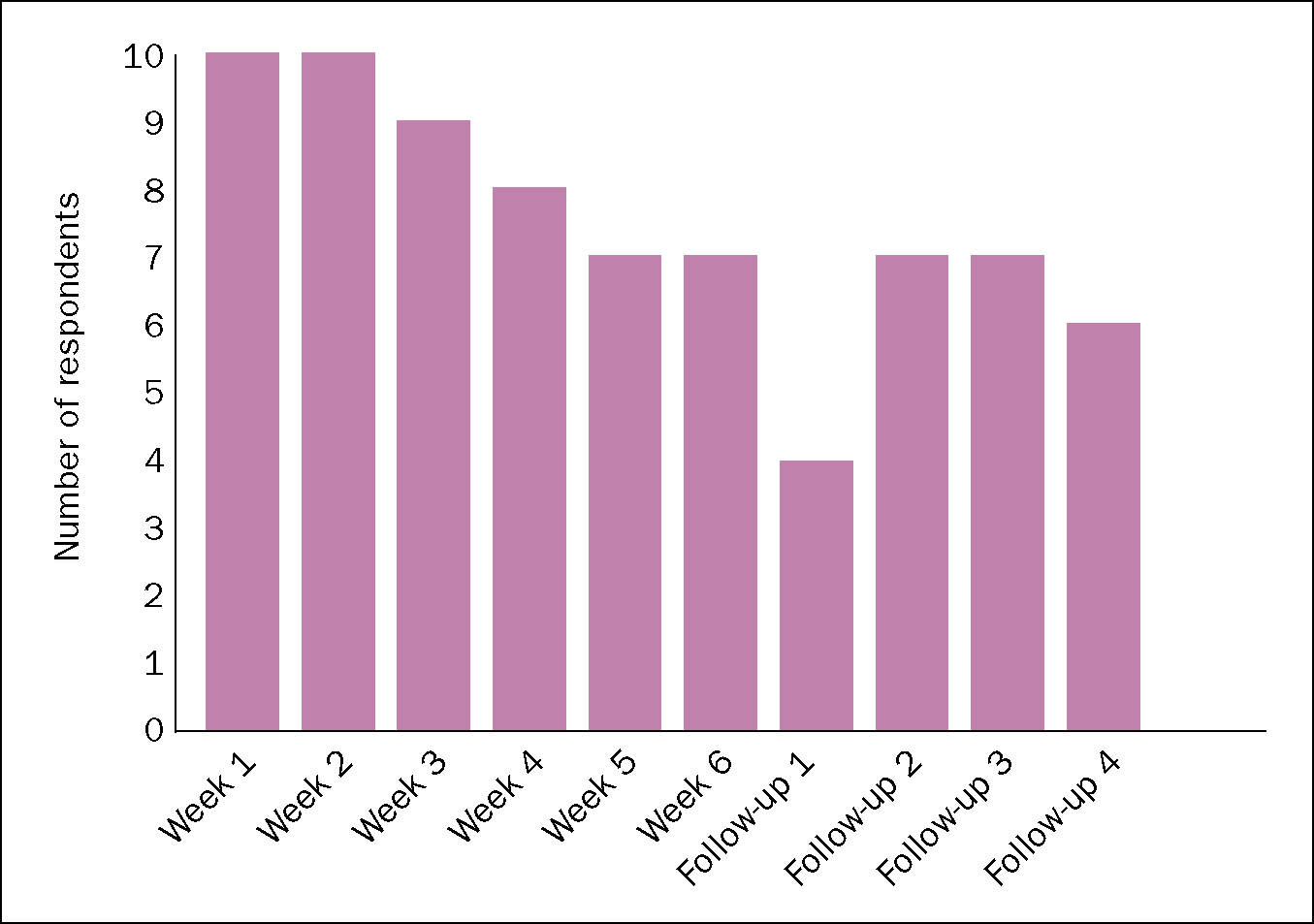
Table 2 lists key participant characteristics for nine participants who provided this data. Participants had a mean age of 31, gestation of 19.7 weeks, BMI of 36.1kg/m2 and the majority were white non/ex-smokers with a pre-tax household income of >£21,000 per year.
| Age (years) | Gestation (weeks) | BMI (kg/m2) | Annual Household Income (£) | Ethnicity | Smoking status |
|---|---|---|---|---|---|
| 34 | 18 | 38.2 | >21 000 | White | Ex-smoker |
| 41 | 17 | 35.5 | >21 000 | White | Ex-smoker |
| 25 | 16 | 34 | 15 501–21 000 | White | Non-smoker |
| 29 | 20 | 40.7 | >21 000 | White | Smoker |
| 27 | 19 | 45.5 | >21 000 | White | Non-smoker |
| 31 | 23 | 31 | Not specified | Non White | Ex-smoker |
| 26 | 24 | 32 | >21 000 | White | Non-smoker |
| 32 | 18 | 38 | Not specified | White | Non-smoker |
| 34 | 22 | 30 | >21 000 | Not specified | Not specified |
| Participant number | Minutes of moderate activity/week | Fruit and vegetable portions per day |
|---|---|---|
| 1 | 0 | 1 |
| 2 | 510 | 2 |
| 3 | 300 | 4 |
| 4 | 195 | 4 |
Six week follow-up data
For eight participants with completed data at 6 weeks, mean self-reported minutes of moderate physical activity, measured through the GPAQ, more than doubled from 478.75 minutes per week at baseline to 1128.75 minutes at follow-up. This difference was not statistically significant [t(7)=-1.80, P=0.115], likely due to the small sample size. Three participants met ACOG guidelines (defined as 100 minutes of moderate or vigorous leisure time activity or active transport per week) at baseline; four met the guidelines at follow-up. Accelerometer-measured steps per week increased from a mean of 5590 at baseline to 6598 at 6 week follow-up, although again the difference did not reach statistical significance [t(7)= -0.894, P=0.401]. Mean self-reported portions of fruit and vegetables consumed per day increased from 3.12 to 7.00 portions per day, a statistically significant difference [t(7)=-3.49, P=0.01]. At baseline, two participants reported meeting the ‘5-a-day’ recommended intake; at follow-up seven of the eight participants were eating ≥5 portions of fruit and vegetables a day. Figure 2 illustrates baseline and follow-up results.
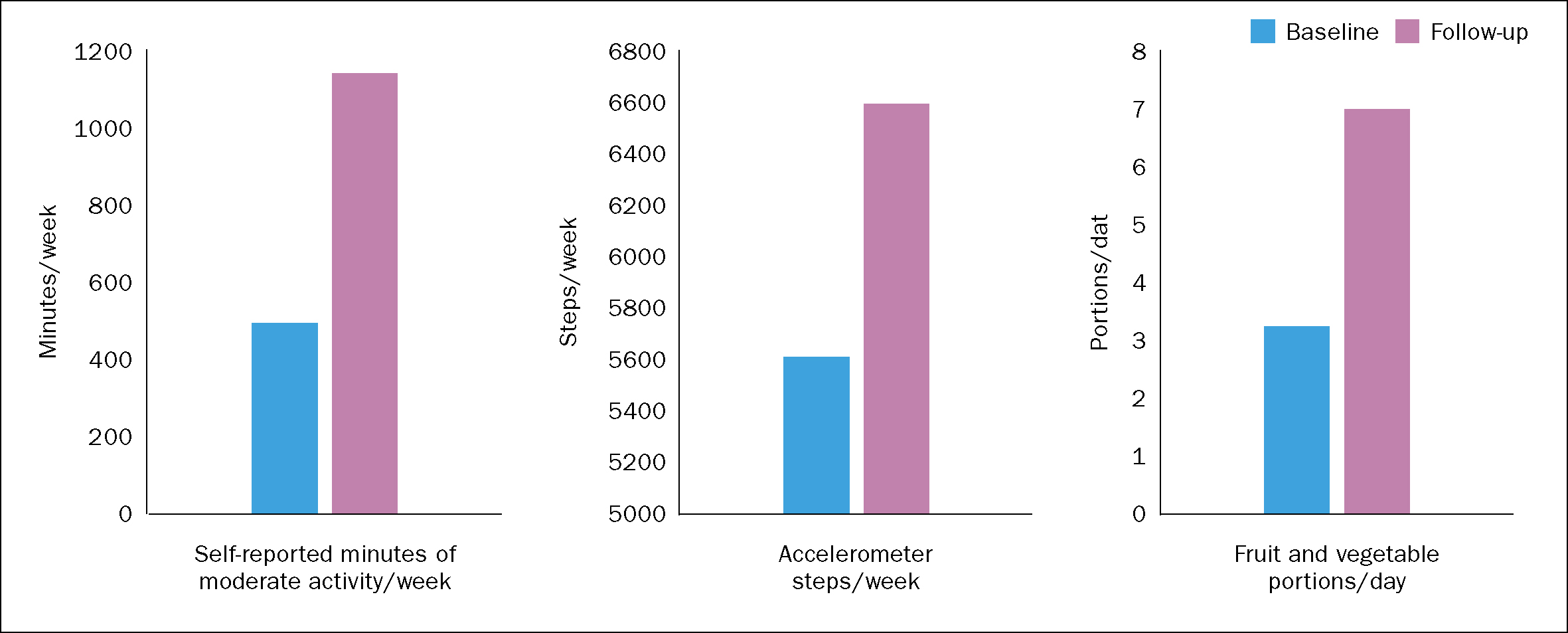
Four month follow-up data
Four women attended the final follow-up session to provide data. Nearly all were full-term or had recently delivered. Understandably, physical activity had decreased, with a mean of 251.25 minutes of moderate activity per week. However, three of the four women were still meeting the ACOG guidelines for physical activity. Self-reported fruit and vegetable intake had also decreased to a mean of 2.75 portions per day.
Participant views of the programme
Participants were highly positive about Bump Start, saying how important the programme had been to them during pregnancy and even volunteering to make a promotional video for health professionals. Four themes emerged from the focus group data: 1) new knowledge, skills and confidence; 2) expert reassurance; 3) making healthy changes; and 4) social ties. Participants described attending for both the health of their baby and to make friends for one participant, ‘it's all reaching down that path of healthy baby’. They enjoyed learning new knowledge, goal setting skills and gaining confidence in healthy living, in the holistic, non-judgemental environment of the group. For example, one participant commented: ‘I looked forward to the meetings, different topics, doing things with the ladies outside the sessions and setting goals each week’. Participants found the multi-disciplinary approach useful and at times reassuring when they had specific pregnancy-related questions for specific professionals. Of many healthy changes they mentioned making, examples included more walking –‘I'm doing a lot more walking now. I get up and go!’ –and efforts towards smaller portion sizes –‘I've taken a smaller plate, I've taken what would be a side plate to have my dinner now’. Finally, the women described gaining much social support from the programme and, through a WhatsApp group, planned to continue meeting for coffee, healthy walks and sharing healthy tips in the longer term. Participants suggested the format of the programme had worked well for them, and thought in future it could include financial advice as part of its holistic focus.
Discussion
Summary of findings
Based on the results of a scoping exercise, a team of midwives, health psychologists, dieticians and physiotherapists developed and piloted a group healthy living programme for antenatal women with a high BMI. Although a small initial pilot, Bump Start had promising initial results, both in terms of engagement of women and health professionals within the programme and women making positive health behaviour changes during their pregnancy. At 6 weeks post-baseline, participants' mean fruit and vegetable consumption had more than doubled, indicating healthy changes to diet. Participants described consuming a mean of seven portions of fruit and vegetables at the 6 week follow-up point, substantially higher than the mean of 4.4 reported for pregnant women generally, within a previous study of Australian women (Wen et al, 2010). Self-reported physical activity and mean accelerometer-measured steps per week had also increased substantially. At 6 week follow-up, 50% of women reported levels of physical activity which met the RCOG guidelines, compared to only 13.1% in a large population sample of pregnant women (Hesketh and Evenson, 2016). Healthy changes mean that gestational weight gain may be minimised, hopefully ultimately reducing pregnancy complications for participants and their babies in this delivery or future deliveries. At 4 months, self-reported physical activity had decreased, although three of the four women who came were meeting RCOG physical activity guidelines. Hesketh and Evenson (2016) reported substantial decreases across the third trimester, even in the general population of pregnant women; perhaps there was less of a decline than could be anticipated for this group. Fruit and vegetable intake had also decreased: women attributed this to either feeling unwell towards the end of their pregnancy and therefore eating very little or having not yet established any kind of healthy routine, having recently delivered. Collection is planned to explore whether women have managed to re-establish their healthy habits.
Furthermore, there was relatively low drop-out until the four month follow-up point where many women were delivering their babies. In a well-attended focus group, participants expressed highly favourable views about Bump Start, its multi-disciplinary, holistic approach and focus on social support, and reported making important and sustainable healthy eating and physical activity changes.
Discussion of what worked well
Undoubtedly, many factors contributed to the results. For research and practice alike, it is important to reflect upon what may have worked well in a pilot intervention to help build on future work. Here four factors are considered: the use of a scoping exercise, emphasis on peer support, multi-disciplinary approach and using and reporting behaviour change theory and technqiues.
Scoping exercise
Bump Start's comprehensive scoping exercise meant that the programme was rooted in what participants wanted and what has been shown to work best. This likely contributed to its success in reaching maximum group numbers. Liaising with various health professional teams throughout the process also meant that staff were aware of the programme and felt included in decisions. This was invaluable in leading to generosity of time when resources were limited, facilitated recruitment and helped build a sense of enthusiasm about the programme. Although this takes time, scoping exercises are a valuable and often neglected part of intervention development, especially within the NHS (Wight et al, 2016).
Peer support
Research has shown antenatal social support to be a mediator of pregnancy outcome (Orr, 2004). For example, stressful situations such as childbirth are perceived as less stressful if the woman woman feels they have adequate and appropriate social support available (Taylor, 2011). Smith et al (2014) highlight the importance of the influence of social support in a community based antenatal lifestyle programme, and suggest that health professionals should provide opportunities for pregnant women to form social support networks. Within Bump Start, participating women and delivering health professionals alike felt peer support was fundamental to the programme's success, as presented in the focus group findings.
Multi-disciplinary team approach
MDTs are often considered the gold standard to developing and delivering safe and effective care (Lemieux-Charles and McGuire, 2006). Working as a team of health psychologists, midwives, dieticians and physiotherapists meant that specialist skills, knowledge and experience could be utilised, creating a relevant, up-to-date and evidence-based programme. Participants explained that while they liked the continuity of the same health psychologist and health improvement midwife attending every session, enabling them to establish trusting relationships, they enjoyed meeting and working with different health professionals each week as it was ‘something different.’ Health professionals commented that the experience of working with an MDT enhanced their own knowledge and skills, and felt they could offer reassuring answers, should participants ask a question that was outside the realm of their specialist knowledge.
Using and reporting BCT and techniques:
Goal-setting is a well recognised behaviour change technique and has been shown to reduce the decline of physical activity during pregnancy (Currie et al, 2013) and reduce gestational weight gain through dietary intervention (Soltani et al, 2016). At the end of each Bump Start session women were given time to set SMART goals, with assistance from the health professionals present. At the beginning of the following session, the women were encouraged to review their goals with the group. The women fed back that setting goals helped them focus on a realistic change and were therefore more likely to achieve it.
Research has shown that monitoring activity using a pedometer is a good way of motivating individuals to undertake physical activity, and has been associated with significant decreases in body mass index and blood pressure (Bravata et al, 2007). Furthermore, BCTs including ‘feedback and monitoring’ have been shown to be effective in reducing gestational weight gain after healthy living programmes have finished (Soltani et al, 2016). Bump Start participants agreed that their Fitbit accelerometer had been helpful, having a motivating effect and enabling them to set goals around increasing their step count. All planned to continue using them. The detailed reporting of session content in this article could hopefully help other interested teams adopt and and adapt our intervention for their local needs.
Limitations of this study
This small pilot study had many limitations in design, measurement and scope. Evidently, it is essential to continue to develop and test Bump Start, ideally progressing to a fully-powered randomised controlled trial, before its effectiveness can be determined. Fruit and vegetables consumed in the past 24 hours was the measure from the chosen ‘5-a-day’ Community Evaluation Tool. A daily food diary may have been a more comprehensive assessment but it was important to minimise participant burden. A single measure was selected to avoid any possible ‘cherrypicking’ of results. However, there are of course many other aspects of unhealthy eating behaviour which contribute to weight gain and obesity. We were also not able to include comprehensive measures of parity and social deprivation—which influence healthy living behaviours—or run intention-to-treat analyses.
Future considerations for practice
Even within this small pilot, the Bump Start team experienced the increasing pressure placed on health services (NHS England, 2013) when trying to source a team of already busy health professionals to assist with the design and delivery of an antenatal lifestyle programme—despite the help of a small Public Health grant. The team relied largely on the enthusiasm and goodwill of colleagues, which may cause issues with sustainability. Further investigation of whether women maintained behavioural changes postnatally will help explore the longer-term effects of the pilot. Nevertheless, investing time, effort and expertise in a programme such as Bump Start may be key to developing a programme which is engaging and likely to be effective; therefore six key recommendations may be helpful for colleagues in other health Trusts:
Conclusion
Overall, a small pilot to develop, deliver and evaluate a community-based group healthy living programme produced promising initial results. This paper has highlighted several aspects that worked well, and challenges faced along the way–which hopefully will be useful to other teams considering developing similar programmes. Innovative thinking, an understanding of behaviour change, proactive engagement with antenatal women in a community setting, and MDT working are all essential ingredients when tackling the issue of maternal obesity.
