All pregnant women in England, Wales and Scotland are offered screening for Down syndrome at their first antenatal (booking) appointment with their midwife (UK National Screening Committee [UK NSC], 2007). Information provided by midwives aim to enable women to make an informed choice to accept or reject screening (de Jong et al, 2014).
With the introduction of non-invasive prenatal testing (NIPT) into the NHS, ensuring women are making informed decisions is vital due to the test's increased accuracy (UK NSC, 2016). If midwives can effectively communicate current Down syndrome screening infor mation and support infor med decision-making, then it will be easier to incorporate NIPT into practice.
National Institute for Health and Care Excellence ([NICE], 2019) guidelines for antenatal care outline that ‘good communication between healthcare professionals and women is essential’; language is key to this. However, oral and written health information is often too complex for the average individual to understand (DeWalt et al, 2004). In attempting to describe aspects of language which could enhance understanding, Adams et al (2009) suggest using plain language, limited ‘medical jargon’, diagrams and checking clients' understanding.
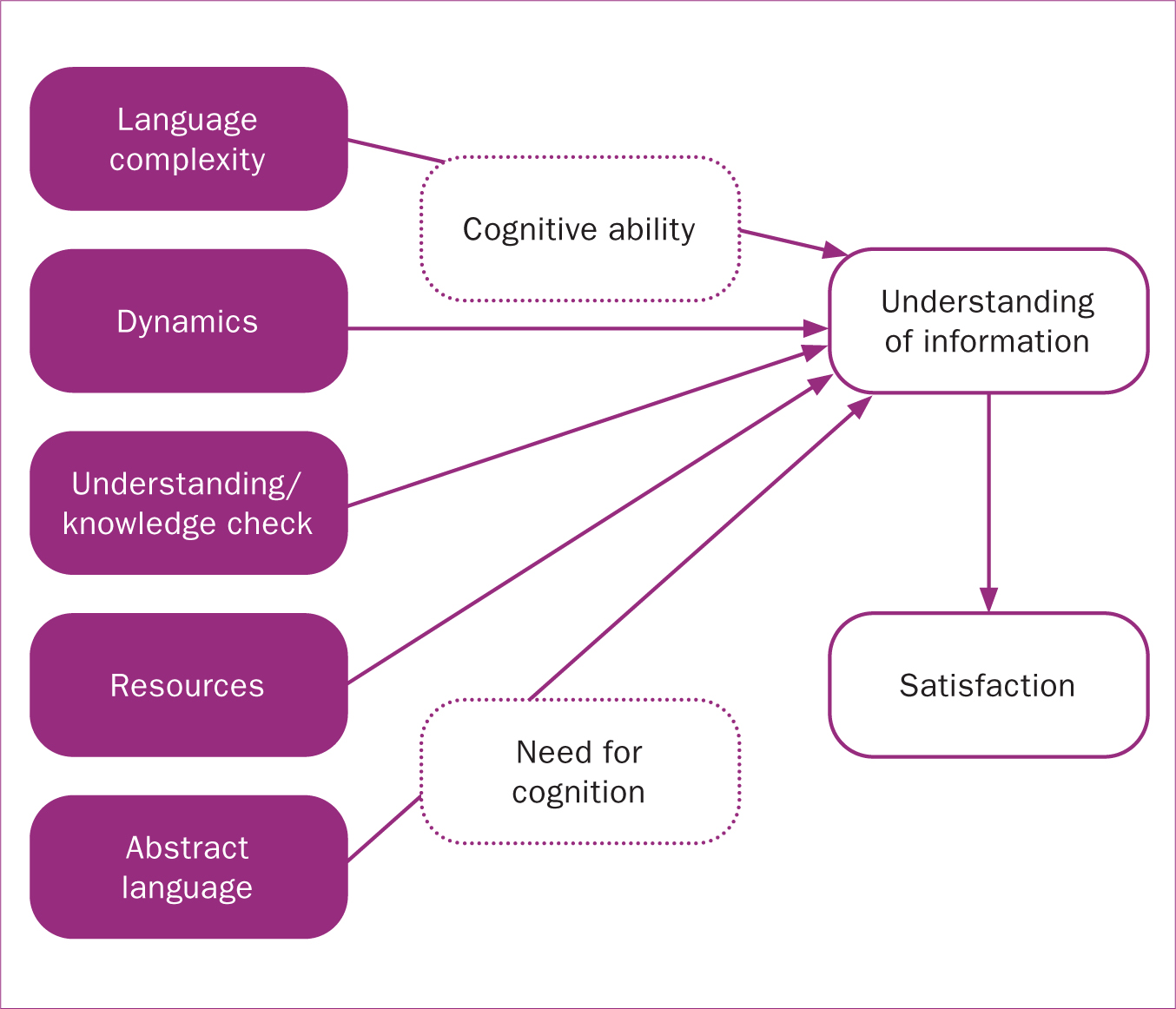
This is the second in a series of papers which aim to identify factors that could influence women's understanding of Down syndrome screening information presented by midwives. The first paper described an assessment tool – measuring understanding of screening information and communication (MUSIC) – that is used to measure women's understanding of Down syndrome screening information, their cognitive status, and the midwives' communicative style.
This paper describes research that uses this tool with the aim to establish how Down syndrome screening information is currently communicated by midwives and the influence of this on women's understanding. As a first step, we explored the literature on factors in midwife communication likely to influence understanding (Table 1).
| Component | Language complexity |
|---|---|
| What it is | Oral communication within antenatal appointments could be made more understandable by using shorter words, phrases and sentences |
| Relevance | Midwives communicate screening and genetic terminology every day, however, the public may be less familiar with it. Within the UK, literacy deficits are widespread and individuals with low literacy in particular are likely to find medical or genetic dialogue difficult to understand |
| References | Erby et al, 2007; Roter et al, 2007; Roter et al, 2009 |
| Component | Dynamics |
| What it is | The dynamics of language can be assessed in a number of ways, such as the pace of conversation, whether the conversation is dominated by one speaker, if it is interactive, or the length of time each speaker talks |
| Relevance | If screening information is provided in a dense ‘lesson type’ format, women may have insufficient time to process the information. Interactive speech facilitates conversation between midwife and woman. Individuals with diverse literacy skills differ in the dynamics they require for optimum learning, emphasising the importance of tailoring information to the individual |
| References | Hunter, 2006; Roter et al, 2009; Deery and Fisher, 2010 |
| Component | Knowledge/understanding check |
| What it is | Women's current knowledge should be established at the start of the appointment and midwives should check understanding throughout the appointment |
| Relevance | To facilitate informed decision-making. However, midwives have noted that they may not ask open questions or encourage interactive conversation due to time pressures |
| References | Dormandy et al, 2005; Porter et al, 2007; Nursing and Midwifery Council, 2018 |
| Component | Resources |
| What it is | Pictures or diagrams can assist verbal explanation |
| Relevance | Additional resources allow visualisation of risk statistics and the screening process. This may be particularly beneficial to individuals with lower literacy skills. Research has found a significant increase in participants' (n=987) ability to interpret numerical risk data correctly when visual aids were used |
| References | Garcia-Retamero and Galesic, 2010; Centre for Health Care Strategies, 2013 |
| Component | Abstract language |
| What it is | Words such as ‘chair’ or ‘needle’, which are easy to visualise or describe events exactly, are referred to as concrete. Abstract words, such as ‘care’ or ‘risk’, are harder to visualise and are open to interpretation |
| Relevance | Information provided within genetic counselling sessions is often abstract which can complicate communication (and impacts comprehension and recall). Using concrete words may thus be preferable but found that individuals with higher literacy learnt better in genetic counselling sessions when more abstract information was presented. This highlights the individual nature of effective interpersonal communication |
| References | Sadoski et al, 1997; Kim, 2009; Roter et al, 2009; Beukeboom et al, 2013 |
| Component | Satisfaction |
| What it is | Good communication should result in improved understanding and greater satisfaction with services provided |
| Relevance | Dissatisfaction with healthcare is often a consequence of a lack of communication. Poorer comprehension could lead to dissatisfaction with services and generate feelings of anxiety, which could cause disadvantageous long-lasting effects |
| References | Paradice, 2002; Roter et al, 2007; Deane-Gray, 2008; Glover, 2014 |
Methods
A new framework, MUSIC, was developed as a tool to assess midwives' communication, women's cognitive status and their understanding of Down syndrome screening information (Figure 1) (John, 2019). This paper focuses on five aspects of midwife communication that may facilitate women's understanding (Table 3).
| Language complexity | Number: word count and sentences | ||
| Average: sentences per paragraph, words per sentences | |||
| Readability: passive sentences, Flesch Reading Ease and Flesch-Kincaid Grade Level. Passive sentence measures how informative text is; the higher the score the more complex and formal the text. The higher the score on the Flesch Reading Ease, the easier the text is to understand: | |||
| Score | Difficulty | ||
| 0–40 | Very difficult to difficult | ||
| 40-80 | Average | ||
| 80+ | Easy to very easy | ||
| Flesch-Kincaid Grade Level should aim for a score of 4.0–5.0 | |||
| Technical terminology score: if any of the following eight words were used in the appointment, it was noted whether the midwife provides an explanation of these words or not: diagnostic, amniocentesis, amniotic, screening, chromosome, abnormalities, millilitres, obstetrician | |||
| Dynamics | Interactivity: number of speaking turns in a session per minute | ||
| Pace: average number of syllables per word × total transcript word count/session length (in seconds) | |||
| Duration: average duration in seconds spanning a block of uninterrupted speech | |||
| Check knowledge/understanding | Knowledge check: do midwives check women's current knowledge levels when they commence the appointment? | ||
| Understanding check: do midwives check that women understand the information throughout the appointment? How do midwives check understanding; do they explicitly ask or use paraphrasing? | |||
| Resources | Are additional resources used to aid explanations, eg pictograms? | ||
| Abstract language | The linguistic category model (LCM) (Semin and Fiedler, 1988): the higher the score, the more abstract the text. Four-word categories are distinguished to produce an ‘abstract score’, computed as follows: | ||
| Word type | Score | ||
| Descriptive action verbs (eg yell, hit, walk) | 1 | ||
| Interpretative action verbs and state action verbs (eg help) | 2 | ||
| State verbs (eg think, admire, hate, appreciate) | 3 | ||
| Adjectives (eg social, aggressive, honest, reliable) | 4 | ||
| Length | Shortest | Longest | Mean |
|---|---|---|---|
| Booking appointment | 00:22:03 | 01:12:07 | 00:44:57 |
| Down syndrome discussion | 00:00:15 | 00:09:08 | 00:02:59 |
Design
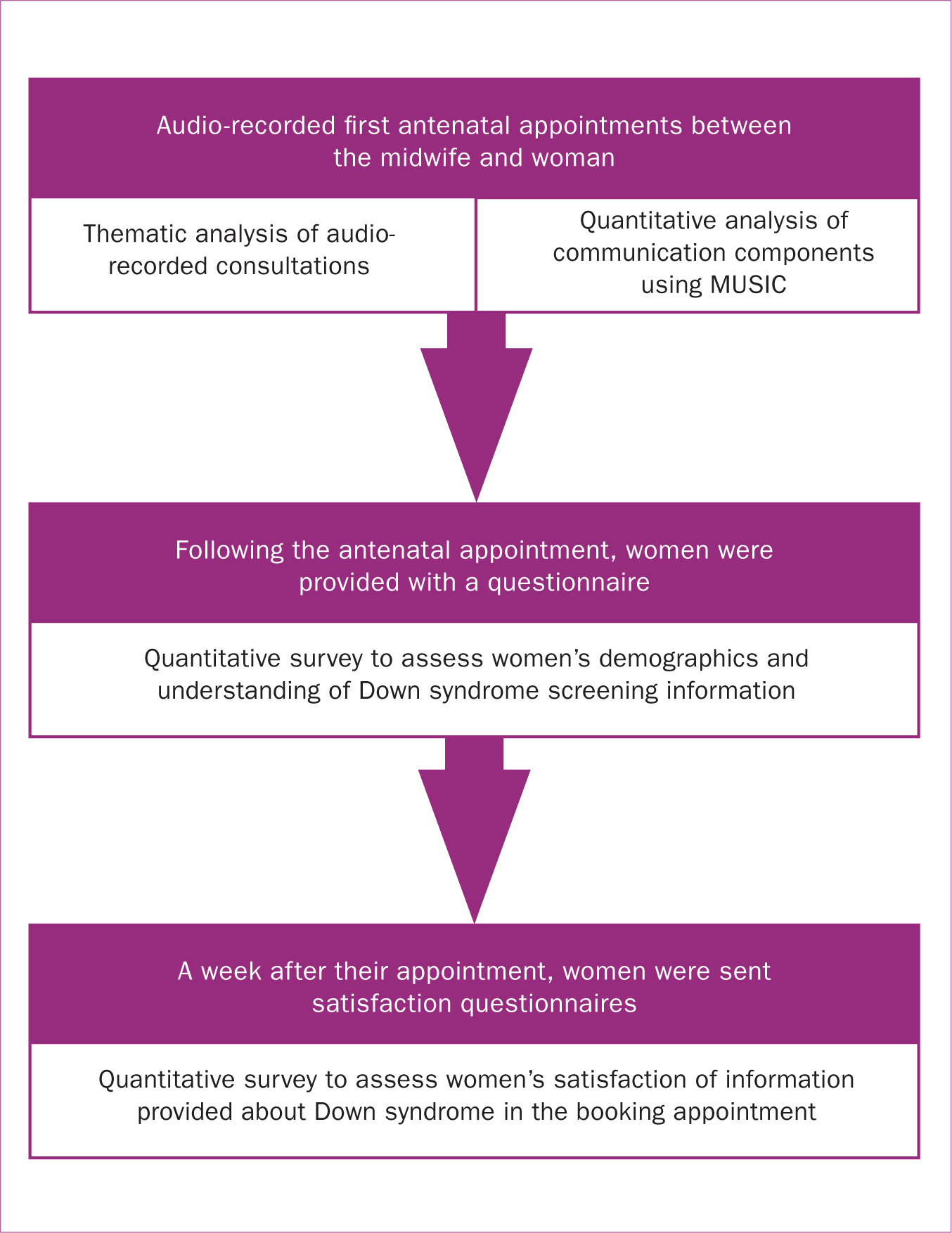
A mixed-methods design was employed using audio-recorded consultations and quantitative surveys (Figure 2).
Study participants
Midwives (n=16) who communicated antenatal screening options to women were recruited from NHS Wales. Women attending their first antenatal booking appointment were recruited by participating midwives. Women were required to be over 16 years of age, have the capacity to consent, and have adequate fluency in written and spoken English. Recruiting only English-speaking women allowed the exploration of midwife communication only as an influence on understanding.
Data collection
The study protocol and data collection is summarised in Figure 2.
Data analysis
Only the communication from the audio recordings relating to Down syndrome screening was transcribed verbatim. The recordings were analysed using both quantitative (Table 2) and qualitative measures.
Thematic analysis was employed to identify the following themes based on findings from the literature review:
Reliability
The research team coded 5% of transcripts to check coding consistency and inter-rater reliability. Any differences were discussed and an agreement was reached. In order to ensure test-retest reliability, 5% of transcripts were randomly selected and rated by the same coder on more than one occasion.
Findings and discussion
Overall, 16 midwives participated and they recruited 100 women aged 17–42 (average 27.6 years). The majority of participants identified as white British (98%). There was great variation in appointment and Down syndrome discussion length (Table 3). Home visits were associated with women having a better understanding compared to women who attended hospital/clinic appointments, although this difference was not significant (Table 4). This may be because midwives dedicated significantly more time to home appointments and Down syndrome screening discussions.
| Setting | N | Mean | Std. deviation | Std. error mean | |
|---|---|---|---|---|---|
| Down syndrome | Clinic | 74 | 6.54 | 2.252 | 0.262 |
| understanding score | Community | 26 | 7.35 | 2.077 | 0.407 |
MUSIC: communication measures
Language complexity
Microsoft Word analysis of transcripts provided a mean Flesch Reading Ease (Flesch, 1948) score classified as ‘plain English’ (Table 5). The mean Flesch-Kincaid Grade Level score was 10.36 which is higher than recommended (Flesch and Kincaid, 1965). Only 5% of dialogue was passive. Sentences should contain 20 words or fewer (Stockmeyer, 2009), however, sentence length averaged over 28 words with one appointment having 59 words per sentence.
| Measure | Range | Mean |
|---|---|---|
| Sentences per paragraph | 1–14 | 3.35 |
| Words per sentence | 4.4–59 | 28.06 |
| Passive sentences | 0–26 | 5.06 |
| Flesch reading ease | 39.5–100 | 69.43 |
| Flesch-Kincaid Grade Level | 0–27.4 | 10.36 |
| Unexplained technical terms | 0–6 | 1.28 |
Dynamics
While on average there were five speaker turns per minute (Table 6), midwives dominated discussions and, on average, spoke for over 2 minutes and 30 seconds. In contrast, women spoke for an average of 15 seconds. One midwife spoke for 2 minutes and 9 seconds in one speech block before the woman spoke, implying that active listening was not always employed. Health professionals should attempt to limit the duration of speech to enhance interactive communication (Roter et al, 2008). Generally, midwives spoke at quite a high pace (Table 6).
| Dynamics | Range | Mean |
|---|---|---|
| Interactivity (speaker turns per min) | 0.47–20.00 | 5.00 |
| Duration (seconds) | 2.60–129.00 | 26.62 |
| Pace (syllables per second) | 3.17–33.25 | 5.00 |
Knowledge/understanding check
Women's knowledge was checked in 44% of appointments, with the majority of midwives asking one question to assess knowledge. The questions asked can be grouped into four categories (Table 7).
| Category | Example |
|---|---|
| Knowledge of Down syndrome | ‘Do you know what I mean by Down syndrome?’ [033] |
| Knowledge of screening and testing | ‘Amniocentesis, have you heard of that?’[008] |
| Knowledge obtained from previous pregnancies | ‘Do you remember the Down syndrome? Did you have Down syndrome screening screening last time?’ [005] |
| Knowledge obtained from information in booklets | ‘Now the main one that we do is the Down syndrome screening, did you read about that with the measurements on the back of the neck?’ [092] |
Questions about whether women had received and read the leaflet were not counted as knowledge checks since reading it does not necessarily equate to understanding.
‘Yeah I read stuff but there was stuff on there that I was like, I don't understand what it—’
Checking women's knowledge at the beginning of the Down syndrome discussion allows the midwife to tailor the appointment. Only one open question was asked by a midwife to explore understanding.
‘Now so what, what, what's your interpretation of the Down syndrome screening?’
‘Oh, I didn't know what it entailed—I just wanted it.’
While this woman has already made a decision, it is uninformed since she does not have knowledge of what screening is. Checking understanding allows the midwife to establish whether women are making informed decisions. Women's understanding was only checked in 28 appointments. Some midwives may not feel they need to check women's understanding. Ahmed and colleagues (2013) found that midwives believed that being an ‘information provider’ was sufficient to facilitate informed choice.
While the Nursing and Midwifery Council (2018) states that health professionals should ‘check people's understanding’, there are no guidelines outlining how to do so. The majority of women were asked direct questions, where admission of non-comprehension could be embarrassing for them. One midwife encouraged agreement which might make it difficult for the woman to disagree.
‘You understand that, don't you?’
One midwife checked whether the woman had enough information to make her decision. Another encouraged questions:
‘If I just have confused you, please [Woman 074: No, no I understand completely] let me know and ask further.’
This supports participation in the individual's own healthcare and can improve understanding (Kountz, 2009). One sensitive approach to assess under-standing was when midwives took responsibility for potential misunderstandings.
‘Is that okay? It's quite complicated the way I've explained it, probably.’
Although, stating that information is confusing may unconsciously support the idea that it is complicated and women may feel they will not learn more by asking further questions. There was no relationship between the number of times midwives checked women's knowledge/understanding and women's understanding of Down syndrome screening information, although this could be due to the low number of questions midwives asked.
Resources
Resources were used in only 3% of appointments. Only one midwife successfully made use of leaflets to show the different screening pathways. Resources may have aided women's understanding however, so few midwives used them and analysis was not viable.
Abstract language
All midwives used similar levels of abstract language, therefore we were unable to establish whether concrete language aids understanding for all, or whether tailoring language, as abstract or concrete, enhances understanding.
Satisfaction
Forty-seven women returned the satisfaction questionnaire, the majority of these (47.8%) found information ‘very easy’ to understand. There was no significant correlation between how easy/difficult women thought the Down syndrome screening information provided was and their understanding.
Previous research has found that women's satisfaction does not necessarily relate to how informed they are (Etchegary et al, 2016), reflecting ‘unconscious incompetence’, in being unaware what they do not know (Howell, 1982). Another explanation is that generally participants do not want to criticise their healthcare provider and consequently, provide high satisfaction ratings (Andersson et al, 2013; Dowswell et al, 2015).
The majority (n=22) felt they learnt most about Down syndrome from their midwife supporting findings that pregnant women generally prefer information face-to-face (Dormandy et al, 2005; Lewis et al, 2014). The next most helpful option (n=17) was the leaflet which supports research outlining that pregnant women value written information (Dahl et al, 2006; Silcock et al, 2015). The internet is increasingly being used as a source of health information (Lagan et al, 2011; Mercer et al, 2014) and our findings support this. When women were asked about improvements to enhance understanding of Down syndrome information, most identified more time and information (Table 8).
| Improvement | n |
|---|---|
| Simpler words | 2 |
| Slower pace | 1 |
| More time | 6 |
| More information | 8 |
| Other [comment: ‘realistic information not just negative’] | 1 |
Most women (n=18) identified that the information the midwife provided helped their understanding ‘a lot’, although this was not reflected in understanding scores. Women were asked to score how much the midwife's description made them think about their screening decision (1=not at all, 5=a lot). Most (n=12) scored 3; there was no significant correlation between this and their understanding score.
Qualitative results
Thematic analysis allowed the identification of subthemes within five overarching themes (Figure 3). A deductive approach using the literature identified the first four themes. An inductive approach was used to recognise the last theme and sub-themes. There was some overlap between sub-themes when analysing transcripts.
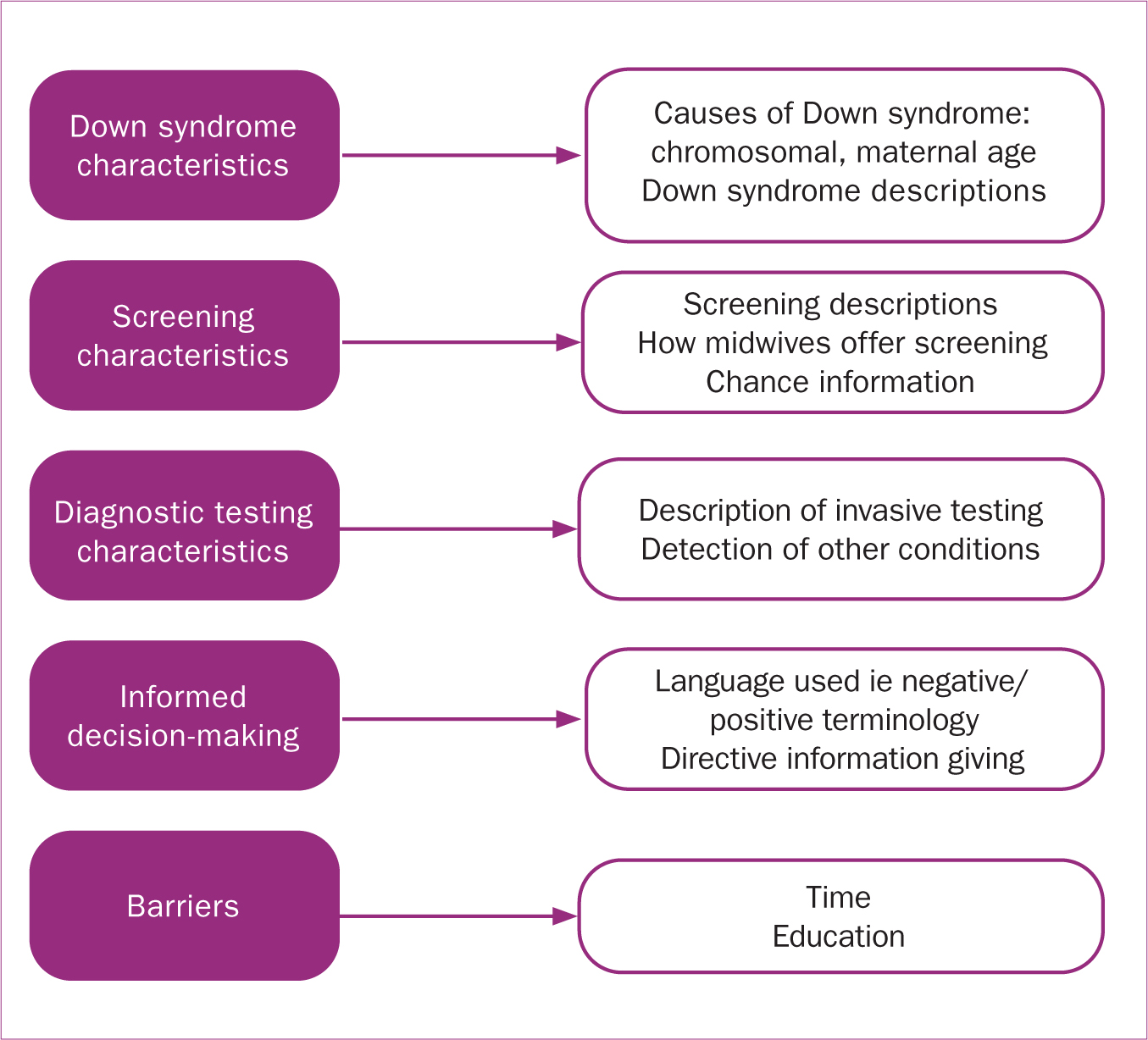
Theme 1: Down syndrome characteristics
Causes of Down syndrome: the causes of Down syndrome were discussed by only five midwives to 27 women. Two midwives sometimes provided inaccurate information: ‘It's a problem with the X and Y chromosome’ [008], ‘It's chromosomal, it's not genetic’ [035]. Five midwives in 18 appointments mentioned that the chances of having a child with Down syndrome increases with maternal age.
Down syndrome descriptions: women want more information regarding the condition (Skirton and Barr, 2010) and expectations of life with a family member with Down syndrome (van Schendel et al, 2016). However, only three midwives described Down syndrome in five appointments, and there were no discussions regarding what life with a child with Down syndrome would be like (Table 9).
| Transcript | Quote |
|---|---|
| 035 | ‘Problem you've got is you can't tell how bad the Downs is [Woman 035: Yeah] because you can have a baby with Down syndrome that goes to mainstream school, does really well [Woman 035: Yeah] and then you can have a baby with Down syndrome that‘s got a lot of health problems and, you know, that can really impact on your lives.’ |
| 088 | ‘There are varying degrees of Down syndrome as well. You can have a child that is quite badly affected with it because obviously we do have other things that happen with Downs, like cardiac problems and things like [Woman 088: Yeah] that and again, you know, any difficulties depend on the severities. You see, there's lots of children on the tele now [Woman 088: Yeah] with Down syndrome that are acting, that are doing brilliantly, [Woman 088: Yeah] leading really good lives, isn't it.’ |
| 095 |
Midwife: ‘But you know what Down syndrome is [Woman 095: Yeah] so they've got sort of classical features [Woman 095: Yeah] with the Down syndrome, but they can have learning difficulties and sometimes they can have cardiac problems so there's varying degrees, you could have a, a child that's very—’ |
Theme 2: screening characteristics
Screening descr iptions: in 15 appointments, combined screening was not described as both a measure of nuchal translucency (NT) and a blood test. In one appointment, neither the blood test nor the NT measurement were described. The quadruple test was discussed in 64 appointments but the procedure was not explained in 9. The quadruple test was not named in the majority of appointments and instead was introduced as ‘the old test’ [100] ‘the 16-week scan’ [052] or as ‘traditional blood tests’ [092].
How midwives offer screening: in the majority of appointments, screening was described and then women were asked to make a decision. In 11 appointments, seven midwives discussed and sought consent for all the screening tests together.
In 19 appointments, six midwives asked whether women wanted screening before it was described, introducing a potential risk of the women making uninformed decisions, for example, seven women thought screening involved invasive testing.
One woman declined screening at the outset and the midwife offered no further information. Another consented to screening, although she had not been provided with any information about Down syndrome or screening. Only one midwife in the sample facilitated informed refusal.
‘You're not going to [Woman 088: No] have the test, yeah? And that's absolutely fine so long as you understand, so if I just explain it quickly so you understand what the test is and what you're not going to have…’
Chance information: midwives did not present chance information consistently. In 61 appointments, the risk statistic (1/150) was presented, however, three midwives did not mention the 1/150 cut-off, with one explaining that ‘it is a risk factor, one in something, ok?’ [018]. The cut-off was incorrectly quoted as 1/250 to two women by two midwives. However, in other appointments, both midwives correctly stated the cut-off was 1/150.
False positive, ‘higher chance that's not a guarantee baby's affected’ [004] and false negative, ‘the women who got a low chance, it's not a guarantee the baby hasn't got Down syndrome but we say, right, low chance—we won't do any further testing’ [003] results were not always communicated by midwives. One midwife falsely reassured multiparous women that they would receive low chance results because they received a low-chance result in previous pregnancies: ‘but you've been fine in the past isn't it, I'm sure it'll all be fine’ [076].
Theme 3: diagnostic testing characteristics
Descriptions of invasive testing: the majority of women (83) opted for Down syndrome screening. Of these, 64 were told about further invasive diagnostic testing and the descriptions provided were not always adequate. In nine appointments, diagnostic testing was mentioned but not described. Only 33 appointments included descriptions regarding both the procedure and the risk of miscarriage. In five appointments, miscarriage risk was only mentioned after women raised it;
‘If you want to proceed in the next stage which is the amniocentesis, which is the needle through the belly button.’
‘Yeah. Yeah which carries a risk of miscarriage as well, doesn't it, yeah?’
In one appointment, the midwife provided incorrect and inconsistent information regarding miscarriage risk:
‘…it's 0.1 so I think that's 1, you know really 1% out of every 100, so it's very low risk.’
One midwife would not describe amniocentesis to a woman ‘unless you come back a high risk’ [055]. Three midwives encouraged women to think about what they would do if they received a high chance screening result. Four midwives attempted to discuss termination, although they only raised it in some of their appointments. However, when termination was discussed, midwives tended to use non-directive language.
‘If the baby was Down syndrome [Woman 016: Yeah] and you were still pregnant, then you are left with the dilemma: do you go ahead with the pregnancy or do you go for termination, and if you've thought about it and you decide: no, that's absolutely fine.’
Detection of other conditions: Down syndrome is often focused on during appointments because it is the most common chromosomal condition (Benn et al, 2015). Only three midwives mentioned the possibility of finding other conditions, with one explaining that ‘they can pick up other chromosomal abnormalities as well but the main thing they're looking for is Down because it is one of the more common chromosomal abnormalities’ [036]. This has ethical implications where women consent to Down syndrome screening without realising that they are also consenting to potentially finding other chromosomal conditions.
Theme 4: informed decision-making
Language used by midwives: three midwives used negative ter minology to descr ibe how women would feel if they received a high chance result:
‘I've seen women who've been really upset because you know they worry then the rest of pregnancy, worrying sick.’
One midwife used repetition – saying, ‘No, no, no’ – to stress that a high chance result is ‘bad news’. Sometimes negative terms were used, such as ‘malformations’ where more neutral terms would have been appropriate, such as ‘alterations’. Furthermore, it should not be assumed that women hold negative views about having a child with Down syndrome: ‘…they're, they're just so adorable and loveable’ [Woman 088]. Screening may thus have been discouraged based on the language employed.
Directive information-giving: directive information fell into two sub-themes; encouragement to have screening; encouragement not to have screening.
Encouragement to have screening: combined screening was promoted as superior to quadruple screening by half of midwives.
‘It's a very, very good test … this test used to be done, actually it's a private thing people, if they wanted it, they'd like to go privately to have it done but now we've got it on the NHS, so it's really good.’
One midwife advocated that others opt for screening, stating for example that ‘most mums and dads now are going for this’ [029] and ‘I'm finding a lot of ladies seem to have the test.’ [035]
Screening was presented as safe by two midwives, which could trivialise screening and make accepting screening seem a simple decision (Table 10). Screening was not always presented as a choice (n=46). Three midwives asked women if they were ‘happy’ to have screening without providing the alternate option. However, in the majority of appointments (n=54), the option of not having screening was presented.
| Transcript | Quote |
|---|---|
| 054 | ‘It's not invasive, [Woman 054: No] it's not, you know, it is just, it is literally just them measuring this area of the back of the [Woman 054: Yeah] neck.’ |
| 056 | ‘Nothing invasive [Woman 056: Oh right, yeah that's fine], it's just a scan.’ |
| 068 | ‘Yeah, yeah and it, that is, it's non-invasive.’ |
| 074 | ‘Just a measurement, it's nothing awful, all they do is measure the fold.’ |
Midwives sometimes assumed women would have screening.
‘I'm going to give you all the information today and I'm actually consenting you so I'm saying today that you're happy to have all the tests.’
This was particularly prevalent when woman had opted for screening on a previous pregnancy.
‘So you had it done last time, so you'd have that done again, would you?’
Encouragement not to have screening: if women did not want further diagnostic testing, or did not think they would terminate the pregnancy, they were sometimes discouraged from screening;
‘It would probably be better then, if you didn't have the blood test because I've seen women having the blood tests, being high chance, they haven't wanted to go for an amnio. They've had this high-chance result with them all the way through the pregnancy and the baby hasn't got Down syndrome. It spoils their pregnancy, so if you wouldn't have an amnio, then am I right in thinking, then, it would probably be better that you don't have the blood test done or, or some people will say, “Well, I still want to have the blood test done”.’
Receiving a high-chance result was framed as a negative outcome: ‘God forbid that you are in the high risk’ [094], ‘you'd think no, no, no, bad news’ [041].
Theme 5: barriers to informed decision-making
Time: often, there was insufficient time for women to make a decision, however, they were still expected to make a choice. Due to time limitations, midwives did not always pursue any uncertainty women had and tended to accept their first decision. For one woman, screening had already been arranged for the following day, potentially pressurising her to decide quickly:
‘Yeah well what you, you got to really think about it so that you know tomorrow now… We need to know before you go for the scan…’
Even when women did not receive leaflets prior to their appointment, they were still expected to make a decision.
‘I know you haven't had much time to think about this [Woman 066: No] now, have you?’
In only one appointment was the woman provided time to consider her decision after the clinic. Six midwives suggested women opt for screening and then opt out at the screening appointment if they changed their mind.
‘Do you want me to say yes today and then if you read it and you think about it, you can decline? [Woman: Yeah] Yeah as long as you let us know before we take your bloods on the next one [Woman: Yeah] … But I'll do all the blood forms ready.’
While these six midwives assured women they could change their mind, the concern with presenting screening in this way is that it could be routinised. McCourt (2006) found that Down syndrome screening information was ‘run through in a rather conveyer-belt fashion’. The current research supports these findings where the majority of appointments followed the pattern set out in midwives' antenatal booklet. Due to time constraints and the amount of information covered within booking appointments, conversations were not very interactive and midwives tended to steer women towards the next question, dominating these conversations and interrupting women to potentially ‘keep them on track’ (Table 11). Down syndrome screening is also one of the last conditions discussed and it could be that by this point, women are already overloaded with information.
| Transcript | Quote |
|---|---|
| 002 |
Midwife: ‘So you said you going to go for it this time?’ |
| 028 | (Woman already received scan date, IVF pregnancy) |
| 041 |
Woman: ‘My friend was 1 in 24, and she panicked all the way through and she wasn't—’ |
| 077 |
Woman: ‘No, I didn't read it. I just said yes to it all |
Education: the causes of Down syndrome were rarely discussed; the term ‘chromosome’, when used, was not explained and two midwives provided incorrect information. Midwives may be insufficiently educated in core genetics concepts and may lack confidence when incorporating genetics into practice (Kirk et al, 2007). With the introduction of NIPT, ongoing education in science literacy, genomics and probability is essential for midwives to deliver accurate information to women confidently (Kirk et al, 2007).
Midwife communication
When we consider these subthemes, it could be that where midwives have sufficient genetic knowledge, they may not communicate it effectively. Tsouroufli (2011) stated that midwives need to be ‘equipped with excellent communication skills, rather than simply have knowledge of antenatal chromosomal screening for Down syndrome’. In our study, midwives did not always adhere to guidelines outlining what topics should be communicated regarding Down syndrome screening.
The information midwives provided was often complex and not interactive, knowledge/understanding was insufficiently checked and there was little evidence of an informed consent process. Not all women were fully informed regarding Down syndrome screening, although they made a decision to accept or reject screening. These findings have significant implications for safe midwifery practice in relation to screening and informed decision-making. Despite this, women seemed satisfied with the services received. The strengths of this research relate to the rigorous development of MUSIC (John, 2019).
However, a study of this complexity is likely to have some limitations. Overall, both the age and ethnicity of women included in this research does not generalise to the wider pregnant population. Therefore, care must be taken with generalising findings and a larger study is required.
Conclusion
This research revealed how information is communicated within day-to-day booking appointments. Vital questions have been raised regarding the way Down syndrome screening is communicated and consequently understood. As NIPT is introduced (Department of Health, 2016), the amount of pre-screening information midwives will be required to communicate will increase and autonomous decision-making will become more challenging (Beulen et al, 2016).
Pre-test counselling for NIPT needs to be balanced, accurate and adequately support informed decision-making (van Schendel et al, 2016). When introducing NIPT, ‘if existing programmes are problematic to start with’ (Munthe, 2015), then new information may be difficult for midwives to learn and communicate. It is imperative that midwives' knowledge is up to date and that screening information is communicated effectively before new screening methods with greater implications are introduced. Ongoing training is required and midwives should be supported at practice, policy and leadership levels to undertake this.


