Although a healthy urinary system is an essential aspect of every woman's life, health professionals often neglect bladder management during pregnancy, labour, and puerperium (Carr and Cook, 2009). The relationship between childbirth and bladder dysfunction is well documented in the medical literature (Chaliha, 2006); however, experiences in maternity bladder care have not been published, and no research has been developed to address this topic to date. Stress urinary incontinence is estimated to be present in over 150 million women worldwide (Irwin et al, 2011), although childbirth is not the only risk factor (Stothers and Friedman, 2011). Modern western lifestyle activities—such as obesity, constipation, smoking, caffeine and alcohol consumption, and certain forms of exercise—contribute to the development of stress urinary incontinence in young nulliparous women of childbearing age (O'Connell et al, 2001). According to 2014/2015 statistics, in England, approximately 58% of women were obese or overweight, 28% ate the recommended five portions of fruit and vegetables a day, 31% played sport at least once per week (NHS Digital, 2016a), and 44% had drank alcohol once a week or more (NHS Digital, 2016b).
The global female population is facing a public health crisis, which is responsible for physical and psychological chronic morbidities that directly affect women's quality of life and socioeconomic outcomes (Minassian et al, 2012; Seshan and Muliira, 2014). This situation is further aggravated by the normalisation of urinary dysfunction (Peake et al, 1999; Avery et al, 2015), embarrassment, stigma, and the subjective nature of the topic, which means that prevalence is likely to be underestimated (Israfil-Bayli et al, 2015). Furthermore, the existence of research gender bias, which is reflected in the under-representation of female participants, prioritises male issues to the detriment of female health issues (Ovseiko et al, 2016), such as urinary incontinence.
It is therefore perhaps not surprising that there has been little focus on women's experiences of bladder care during childbirth. This situation represents a squandered opportunity to inform, explore, and diagnose postnatal urinary incontinence (Butterfield et al, 2007), as well as chronic failure to promote healthy urinary systems and increase the degree of awareness and control of bladder health among women. This feeling of control (Bryanton et al, 2008), coupled with the level of childbirth preparation and expectation (Goodman et al, 2004), affects women's satisfaction with maternity experiences. In order to highlight this, the present study provides insight into women's knowledge, perceptions, and opinions of their maternity bladder care.
Methods
Study aim
The aim of this study was to explore experiences of bladder care during pregnancy, labour, and after birth.
Study design
A qualitative, exploratory, and descriptive approach was used for this study.
Sampling and setting
A purposive sample of nine participants was sought from women who had received maternity care and given birth at one hospital in south England and/or its two associated birth centres.
Participants
Participants were eligible to join the study if they met the inclusion and exclusion criteria (Table 1).
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
|
To avoid biasing the participant-researcher interaction, participants were also excluded if they had received clinical midwifery care from the principal investigator (Moch, 1999). Initially, postnatal midwives screened for potential participants before discharge; however, this strategy was unsuccessful. Therefore, additional ethics committee approval was obtained to recruit via the Facebook pages of local maternity groups, which proved to be very effective. A heterogeneous representation of different modes of birth was sought (Table 2).
| Participant | Parity | Mode of birth | Baby's age at interview | Catheter required | Leaking episodes |
|---|---|---|---|---|---|
| Cally | 2 | Water birth with perineal tear (repaired) | 6 months | No | After birth |
| Shannon | 1 | Water birth with grazes (no repair needed) | 4 months | Unable to urinate after birth | After birth |
| Sarah | 2 | Water birth with perineal tear (repaired) | 8 weeks | No | After birth |
| Halina | 1 | Forceps, epidural and episiotomy | 6 weeks | With epidural | After birth |
| Alice | 1 | Ventouse with episiotomy | 6 months | No | After birth |
| Abi | 1 | Forceps, episiotomy and epidural | 7 weeks | With epidural | In pregnancy |
| Karla | 2 | Spontaneous vaginal birth with perineal tear (repaired) | Less than 6 weeks | No | None |
| Lisa | 2 | Spontaneous vaginal birth (no perineal repair) | 19 weeks | Management of retained placenta | None |
| Anna | 1 | Elective caesarean section | 7.5 weeks | At caesarean section | In pregnancy |
Data collection
The principal investigator, a female practising midwife and Master's degree student in Clinical and Health Research, undertook in-depth, semi-structured interviews at a time and place at participants' convenience (a participant's home or the university). An interview guide (Box 1) was used to minimise interviewer bias, and to perform universal enquiry across all participants (McNamara, 2009). This interview guide was previously piloted, and the data collected were included for analysis. A total of nine women participated in the study. Interviews lasted from 15–54 minutes, were digitally recorded, and transcribed verbatim. Data were collected between February and March 2017. Participants selected their own pseudonyms.
Data analysis
The data obtained were analysed using the framework from Pope et al (2000), following an inductive perspective and assisted by a memo technique (Birks et al, 2008). To ensure trustworthiness and to establish confirmability in the analytical process, an audit trail (Lincoln and Guba, 1985) was used (Table 3).
| Themes | Key areas | Final themes | Overarching theme |
|---|---|---|---|
| Bladder care discussion, issues, experience with leaking (pregnancy and post-birth) | Experience | Muddling through to earn a ‘badge of honour’ | Lack of care |
| Experience of second-time mothers (false reassurance) | |||
| Women's assumptions: getting on with things; mismatch between expectations and reality | Expectations | ||
| Baby seen as a priority | Priorities | Caring for a baby, but who cares for me? | |
| Physical issues less important than mental health problems | |||
| Bladder care: antenatal appointments and urine samples | Care | ||
| Ante- and postnatal bladder care: lack of direct enquiry | |||
| Lack of information about a healthy bladder | Information | Do you speak ‘bladder language’? | |
| Internet to validate expectations, experience and feelings | |||
| Knowledge related to experience | Knowledge | ||
| Relationship between pelvic floor and bladder care | |||
| Self-realisation after talking about it | Thoughts | ||
| Worries about continence in pregnancy |
Findings
This study was expecting to collect women's experiences of bladder care during pregnancy, labour and after birth. However, women interviewed reported to have had limited maternity bladder care. Instead, they focused their attention on disclosing their experiences of bladder issues, particularly urinary incontinence. Consequently, the main finding was that there was a scarcity of maternity bladder care received by the women interviewed.
Overall, of the nine women interviewed, five had experienced some degree of incontinence following birth and two during pregnancy. Initially, seven themes emerged by applying the framework analysis. An amalgamation of common themes was carried out following consensus with the principal investigator's supervisor, resulting in four final themes (Table 3).
Muddling through to earn ‘a badge of honour’
Areas identified were: environment, mismatch of expectations and reality, false reassurance, lack of preparation, normalisation, and ‘getting on with it’ (Figure 1).
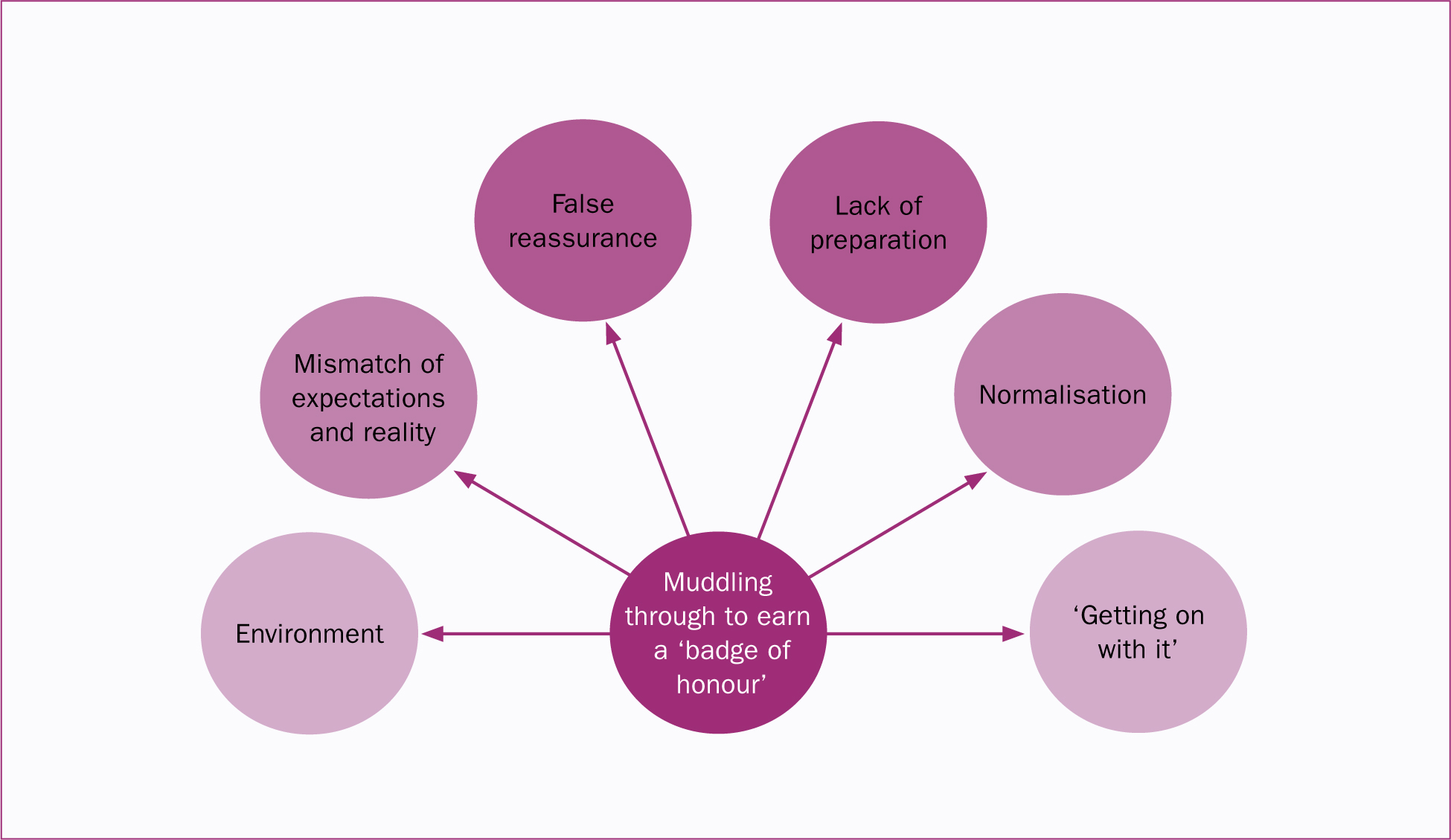
Although women recognised that their bodies had changed after they had given birth, those experiencing urinary leaking episodes did not regard them as a symptom of ill health, but rather a formality of the childbearing experience. Moreover, this incontinence after birth seemed to be translated into a ‘badge of honour’. One participant in particular realised that she was experiencing urinary incontinence only after discussing her experience. Consequently, only three women had disclosed their symptoms to a health professional. By contrast, other women felt ‘lucky’, regardless of whether they had experienced incontinence or not:
‘That joke about how once you have a baby, things won't be the same and all that, which nobody tells you before you have a baby—obviously. I suppose it's almost like a badge of honour, isn't it? Things definitely change […] I guess it's just one of those things, isn't it? There's nothing you can do about it really […] and actually, until you came here today, I wouldn't have said I had problems, which is quite interesting. I just agreed to do the study to help.’
The findings also revealed an evident mismatch between expectations and reality. This mismatch could be explained by a lack of expectations that the women possessed regarding maternity bladder care. One participant in particular did not expect young women to experience urinary incontinence, largely due to the association of incontinence with older age, its normalisation through the media, and the advertisement of incontinence pads on TV:
‘Before I was pregnant it was … it was something definitely to happen to older people or disabled people.’
Women's expectations varied according to the number of babies they had, highlighting how these mothers learnt from experience. Based on this, second-time mothers who participated in the study were expected to have acquired knowledge from previous pregnancies, which made them assume that they had to ‘get on with it’:
‘For second-time mums they just expect you to know, you know, kind of get on with it […] I was fine cos it's your second one, you kind of just get on with it, you don't worry about them things.’
The pressure that health professionals exerted on second-time mothers could provide a false sense of security, as women built their expectations from exposure. Therefore, if their expectations did not match their reality with their first baby, this would be perpetuated in subsequent pregnancies. Another false reassurance was noted as a result of the ability to urinate ‘normally’ after birth, in contrast with the appearance of urinary incontinence months later:
‘I think perhaps it gave me like a false sense of security, like, after I had him that … because I was able to like pee, like, a bucket.’
Expectations about a healthy bladder came from the environment, and women (particularly those experiencing ‘leaking’ issues during the postpartum period) either normalised or worried about them, depending on the experiences of their inner circle:
‘People laugh about [how] even if you sneeze you wet yourself, and, you know, sort of don't jump up and down and that sort of thing. So I guess it's just normal anyway.’
Although they expected certain degrees of adjustment in the postpartum period, women felt that the lack of preparation regarding bladder changes significantly affected their ability to process the experience. Anticipation and forewarning would have been preferred, as opposed to dealing with unforeseen issues during a vulnerable time:
‘I expected [there] to be some difference, but it did really sort of surprise me quite a lot, and they said because of the forceps can cause some trauma to the bladder […] I think there may be a bit more emphasis put on it to say, you know, “At this extreme, this could happen, and it is quite normal” […] because I only had that conversation really after it happened. But at that point, you sat there and cried about it and then you've got the advice and you are emotional anyway cos you've just given birth—and so it's not the best time for them to be told […] other people go through it, so to have been told before hand.’
Moreover, women did not seem to feel the need to practise pelvic floor exercises (PFE) despite the existence of leaking issues. One participant, Cally, was able to urinate as she had done before the birth, and therefore did not see a need for exercises, despite episodes of urinary incontinence:
‘It's not something that you need to do, like if you are hungry you need to eat and it's easy, you can fix your problem, but you don't need to do your PFE […] if it's working you don't sort of think about it.’
Caring for a baby, but who cares for me?
This theme covered mothers' and professionals' priorities, and showed how barriers to disclosing bladder problems were exacerbated by a lack of direct enquiry (Figure 2).
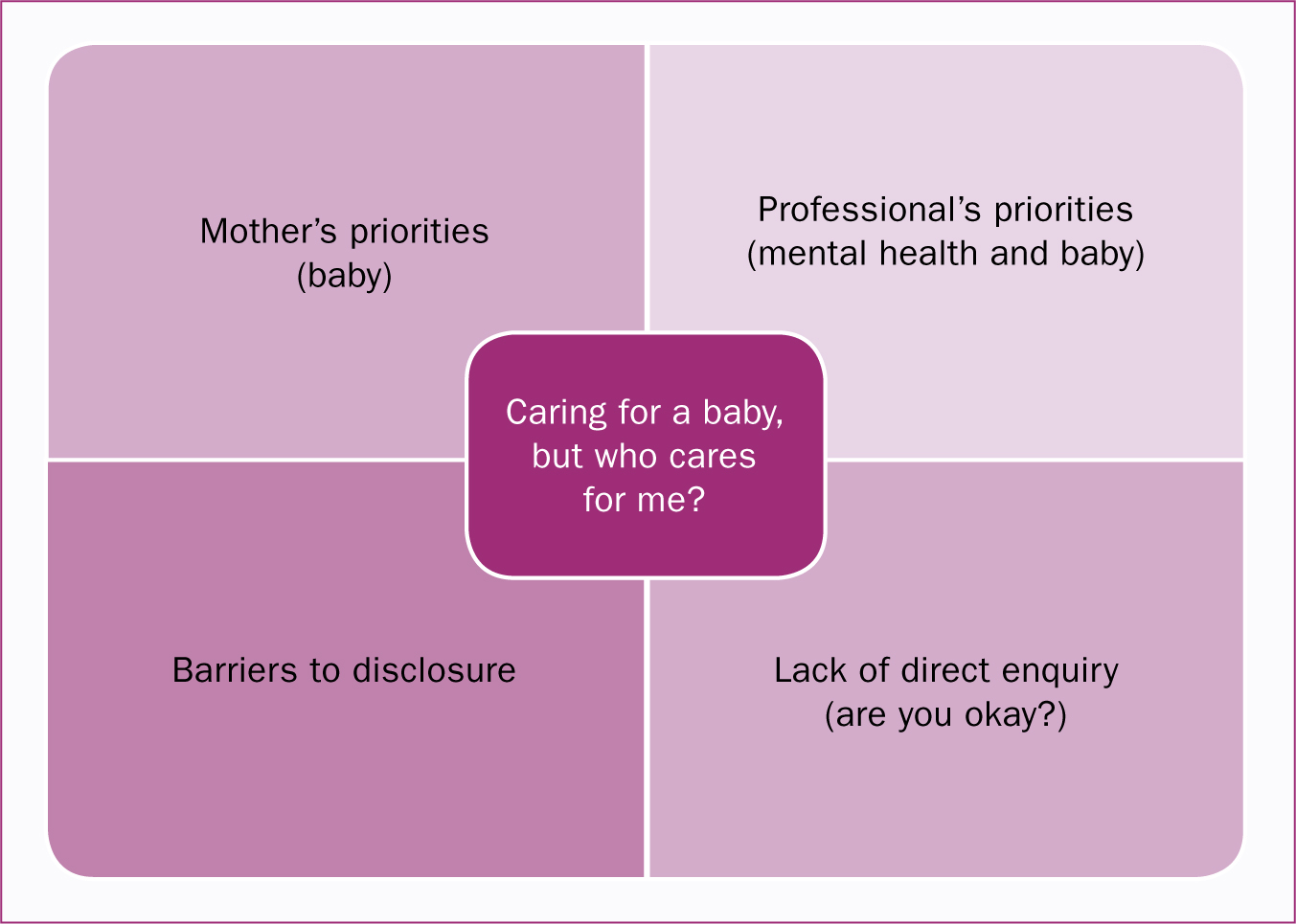
Women reported that all of their efforts shifted towards their babies, their families, and their houses to the detriment of themselves during the postnatal period.
‘I do think that sort of is more about them than it is about you […] like your care for yourself tends to go out the window.’
‘All you are thinking about is feeding and the baby. You don't really worry about yourself.’
Prioritising their baby's needs was perceived to have a prejudicial effect on women's ability to maintain a healthy bladder. Despite prior or ongoing incontinence, a fully functioning urinary system did not seem to be a priority for some women.
‘Yes, I am [incontinent] at the moment, so hopefully I will do something about that respect. It's not … it's not really in my mind to be honest, with these two [children].’
‘Just when you have a baby … after the baby it's like … oh, everything is your baby and you just don't think to sit there and just do [PFE] for 2 minutes. You are thinking of doing something else, like, “Oh the baby's asleep, let's clean the house or make dinner, or like, do all the house, like, duties.”’
Additionally, women believed that clinicians seemed not to prioritise physiological and pathological physical changes that occurred during the postpartum period.
‘There's so much focus on the birth and what to do before … I think other than postnatal depression, which is, you know, heavily touched on, kind of what happens to your body and everything else is probably … there's less emphasis on that because I think it's almost, “There you go, you are fine, off you go”. And I think that's probably where there needs to be more focus, so just … you've been all prepared for it.’
‘When I saw the title of your paper I thought, ‘That's quite unusual’ because most postpartum care tends to focus on breastfeeding, periods, fertility, weight gain, depression, moods, and things. So that, to me, indicates that it's quite low down in people's list of priorities because it is all about how you and the baby are, if the baby is feeding, if the baby is growing, if you are healing, if you are depressed, how is your mood …’
During the antenatal period, women did not notice any difference in the prioritisation of care from health workers, and healthcare providers seemed to miss opportunities to enquire about, promote, and provide bladder care. Instead, any hint at bladder management ended at the collection of urine samples:
‘It's more about whether I had a urine infection rather than whether there was continence. That was more the question—whether I had cystitis, I suppose.’
‘I didn't really think about bladder care during pregnancy to be honest, maybe she [midwife] should have mentioned … I don't know, asking more about how I was passing urine, if it hurts, you know, anything like that. But they mainly just took your urine sample every time you went in and just check, like, the protein and stuff.’
Due to the apparent insignificance of bladder care, women were led to believing that any bladder symptom lacked value compared to other areas of maternity care, which could be regarded as a barrier for disclosure. The women interviewed had also expressed their concerns about discussing their bladder status with health professionals. One participant manifested her internal conflict between embarrassment and speaking up for the sake of her own health:
‘I'm just trying to just get by and not mention stuff […] But it's when the doctor came around when I was in hospital and explained just how important it was […] I was about to be discharged actually, when I thought, “I'm not sure if, you know, I've got issues with my bladder” […] but yeah, that was only from them speaking to me that I kind of then understood really how important it was to say something […] The embarrassment and everything, you have to kind of get over that. Particularly, if I hadn't said anything, I could have gone home and had problems […] but I could see how people may get embarrassed or worried about talking about it.’
Other barriers to disclosure identified were related to how professionals—particularly GPs at the routine 6-week postnatal check—presented themselves and dealt with care. Clinicians' characteristics were also mentioned. Women emphasised the lack of direct and specific enquiry regarding potential bladder problems, which was regarded as a preferable option to spontaneous disclosure:
‘I think he [GP] was a bit shy […] I didn't really get the impression like he was particularly confident talking about women's issues […] They could have been a bit more sort of specific […] covering the questions specifically—asking if there was a problem or not.’
‘It just didn't feel like a natural situation to bring it back, but I had a few questions I would have liked to ask, but he [GP] couldn't have been less interested really […] He didn't have a great bedside manner so … it would have made more sense to me, I suppose, if they give you […] someone who perhaps has a bit of, you know, caring nature about them.’
Do you speak ‘bladder language’?
This theme encompassed issues of information and advice provided to women, their lack of understanding, the language used, and use of the internet (Figure 3).
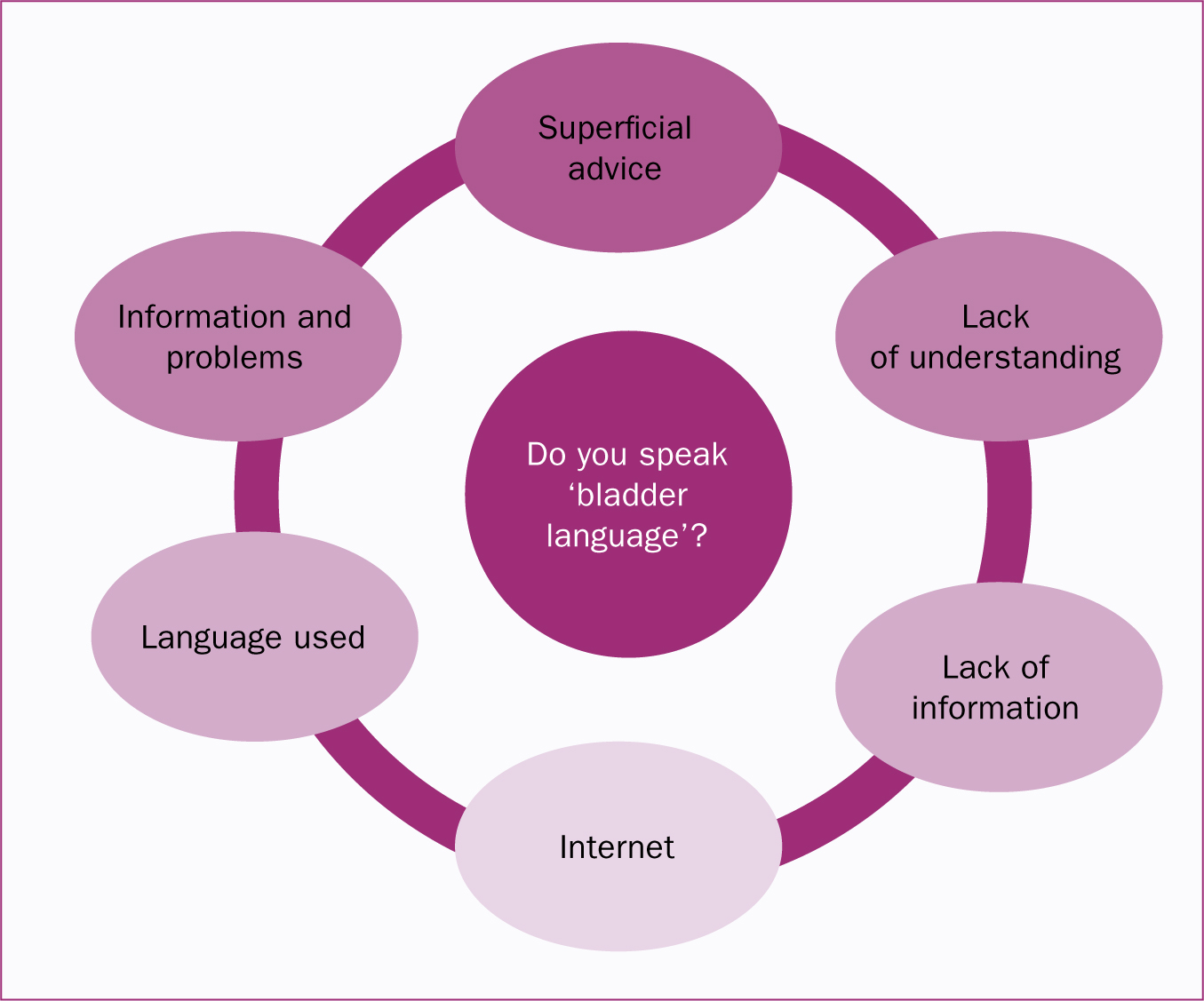
Women's lack of understanding of bladder terminology such as ‘bladder care’, ‘hesitancy’, ‘urine flow’, and the link between pelvic floor muscles and continence created a potential for misinterpretation and miscommunication between health care providers and women. The ambiguous approach and language used by clinicians to enquire about bladder functioning aggravated this lack of understanding, and meant that assessment was narrowed to a woman's ability to pass urine. For some women, this enquiry alone was not enough to trigger disclosure.
‘I was told to keep doing PFE after birth. I don't know if that was to do with my bladder and going to the toilet, or if that was to do with helping with the stitches to heal.’
‘I think she [midwife] asked if I have been passing urine, but … that's about it really.’
If women are not familiarised and actively informed about bladder care, inertia may lead them to normalise certain symptoms such as leaking urine after birth, and lack of sensation and control.
Some clinicians, likely intending provide reassurance, also diminished women's worries, possibly explaining why this common issue has been misinterpreted and normalised by participants:
‘I've been like, not able to make it to the toilet […] I know it's obviously a common thing that can happen […] My partner has said to go to the doctor but I'll just see because I know it's quite a common thing after … I've just sort of been using like, a pad.’
‘I was … actually told this is quite common as well, you know (from clinicians).’
‘I said, “I'm a bit concerned”, and she [health visitor/midwife] just went, “Oh, you are gonna get some of that after.” It was like, “But yeah, it's my second one and I kind of know what to expect.
I know it's gonna going to be weak, but I'm saying I am actually worried about this,” and yeah, one of them didn't really take it on board.’
Women expressed concern regarding the paucity of information related to bladder care, both during and after their pregnancy. In contrast, they felt overwhelmed about the amount of information at discharge, among which bladder care and pelvic floor promotion was not present:
‘I don't think it's addressed that much […] I think it would be good to incorporate that in sort of the midwife appointment or classes cos I think it's kind of not really touched on enough.’
‘I think it's one of those things, you just sort of—you know about this sort of thing. So it goes without saying, I guess.’
Information on and promotion of PFE was not a universal recommendation during pregnancy and after birth. Women often received recommendations from non-health care providers such as yoga or Pilates classes or pregnancy books, and some were concerned about the fact that PFE were generally not discussed in great detail:
‘It's kind of just, “Oh don't forget to do your PFE” and it's like, “Oh, how exactly should I be doing them?” But I don't know. You do them, but you don't know if you do them effectively or if you are just sort of not doing it right at all.’
‘They all sort of mentioned generally, “Make sure you do PFE”, but they don't really go into detail. Maybe they don't want to embarrass people. I don't know, or they just haven't got time.’
This lack information from clinicians could explain women's increasing use of internet resources, such as mothers' forums and Facebook groups, to validate women's experiences, expectations, and feelings, and to compensate for the absence of professional input:
‘You can cope with anything, I think, if you just think you are not alone […] So not looking for advice, just reassurance I guess, of other people having had the same problems I had.’
‘Looking for advice, like Googling “Is it normal for this?”’
Although women felt uninformed about their maternity bladder care, they were generally quite satisfied with their degree of awareness related to the provision of information on ill health:
‘There wasn't really that much information otherwise, but then I hadn't really had problems.’
In contrast, a participant who experienced incontinence and lack of control directly after birth believed in the importance of pre-emptively informing new mothers about the possibility of bladder problems. Nevertheless, she was torn between informing and/or scaring her pregnant friends:
‘I have tried not to scare them […] I have already spoken to them beforehand and just said, “Just be aware that this can happen.” […] I think if someone said to me, then I might not have been quite so scared when it happened […] they talk about pelvic floor, “You may lose a bit of feeling”, but that's quite far from, you know, “You might wet yourself”, I think. But also, you don't want to scare somebody who is about to have a child, so I think it's just in a sensitive way to mention that, you know, this can happen. And as I said, when I've heard after the event that other people have had the same issue, it's actually quite reassuring. I think just to hear you are not alone. And it does, you know, it does get better. It's not forever.’
Discussion
This study portrays the first in-depth views of experiences in maternity bladder care. Although this investigation did not specifically aim to target participants with urinary symptoms, it appeared that women experiencing some degree of bladder and pelvic floor issues might have felt attracted to take part in the study. Moreover, although the focus of the study was to explore experiences of care during pregnancy, labour, and after birth, the antenatal and postpartum periods were the focus for the majority of women interviewed. This could be explained by the importance that labouring women may place on other areas of care, and their perception of being less autonomous regarding their bladder care during birth.
The results of this study revealed that women experiencing bladder changes after birth, such as loss of control, lack of sensation, or leaking episodes, tended to normalise and accept them. They also used conservative measures or waited for a spontaneous resolution, rather than seeking professional help. This attitude could be explained by their constructed expectations of the childbirth experience, a trend also identified in a study focusing on women experiencing urinary symptoms after childbirth (Wagg et al, 2017). In Melville et al's (2008) interviews with non-pregnant women about their perception of the aetiology of urinary incontinence, the authors also concluded that bladder problems were understood to be beyond a person's control and part of being female. This attitude is reinforced by the lack of knowledge that women generally possess regarding maternity bladder physiology. As such, women face the dilemma of how to recognise when something is wrong if they remain unaware of what is right.
Unfortunately, the majority of women interviewed in the study felt disappointed by practitioners. Antenatally, clinicians seemed to focus on illness diagnosis through urinalysis, while postnatally they only seem to pay attention to babies and mental health issues. Therefore, it is evident that the postpartum period continues to be a neglected area of women's health, fuelled by a ‘conspiracy of silence’ (Strahle and Stainton, 2006). In order to break free of this vicious cycle, clinicians should actively discuss bladder care and look beyond a woman's ability to pass urine. Promoting a healthy bladder during pregnancy and after birth should not be limited to checking urine samples and recommending PFE. This neglect of bladder care could be originated by a professional's lack of knowledge (Williams et al, 2003) or even clinicians' embarrassment, which contrasts with women's willingness to be openly asked about their bladder status.
Another neglected area intrinsically related to bladder care is pelvic floor health promotion. Most women in the present study expressed concerns regarding the lack of information on PFE, including frequency, techniques, and—most importantly—duration. It is worrying that some women in the present study did not relate continence to their pelvic floor and were expected to undertake PFE for a limited period of time. It is vital that women embed PFE into their daily routine for the rest of their lives (International Urogynaecological Association, 2011), and more emphasis should be placed on this recommendation. Women would greatly benefit from a detailed explanation of PFE, rather than a simple reminder to do the exercises.
Participants also sought information regarding bladder/pelvic floor changes in both pregnancy and after birth in order to anticipate and prepare themselves, as opposed to dealing with an unexpected reality. In this context, multiparous women could also be at an increased risk for developing anxiety and frustration. The underestimation of multiparous women's needs (Cooke and Stacey, 2003), resulting from professionals' ‘you already know’ approach, could be regarded as a barrier to disclosing bladder problems, which further reinforces the normalisation of symptoms. Consequently, the use of internet resources to compensate for a lack of professional guidance should not be a surprise. Clinicians should consider acknowledging this gap and provide individualised care in order to avoid service users' anxiety caused by using the internet to seek health-related information for reassurance (Starcevic and Berle, 2013).
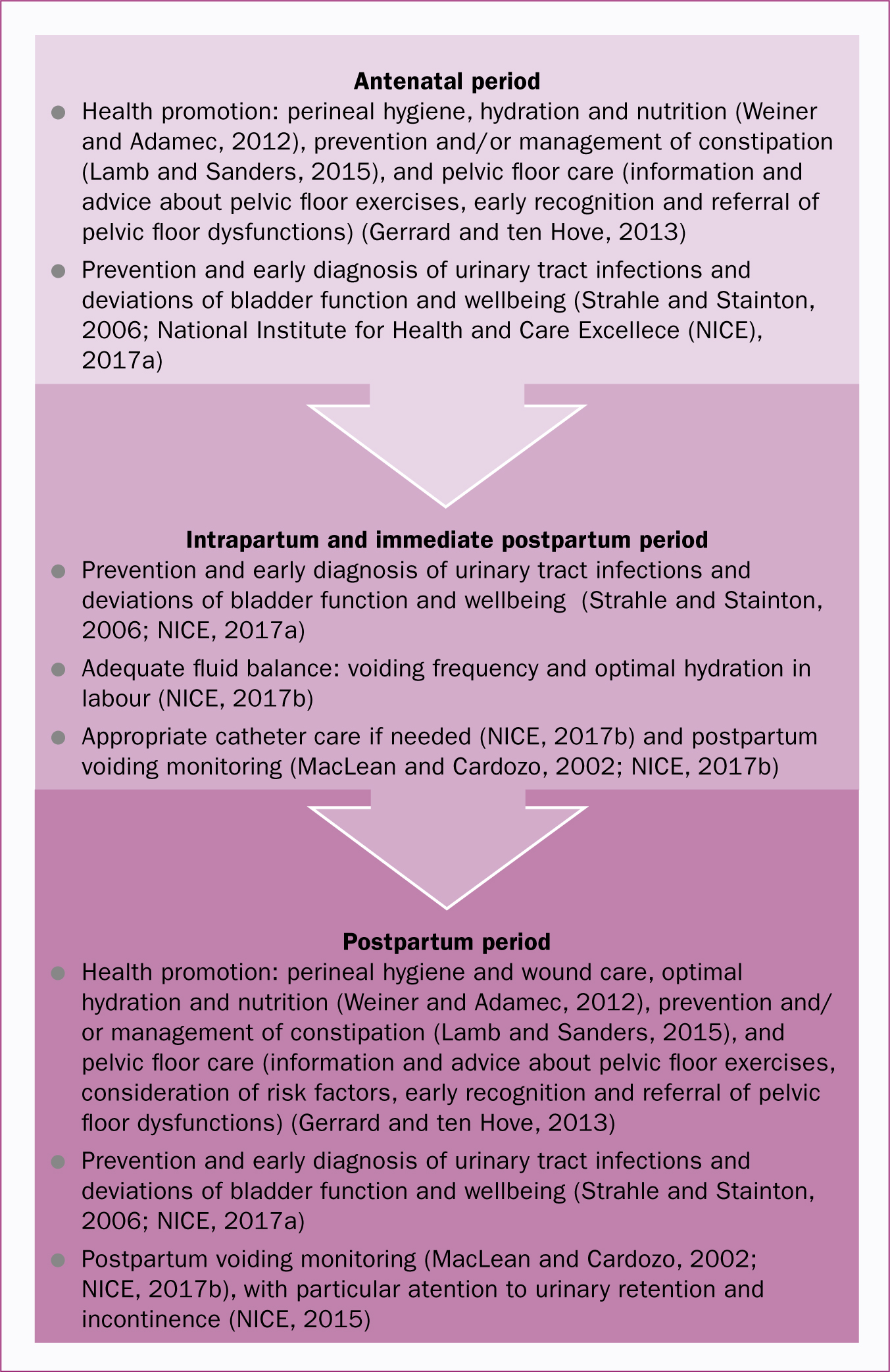
Moreover, professional neglect is exacerbated by the self-neglect that women apply to themselves when a new baby becomes the primary focus of their attention. Haines et al (2013: 431) highlighted that ‘women's beliefs and attitudes regarding pregnancy and birth are likely to influence what aspects of care are important to them’. Haines et al (2013) demonstrated the minimal expectations that women have regarding their own bladder care, resulting in the devaluation of bladder changes in the postpartum period. The authors also identified three attitudinal profiles (self-determiners, ‘take it as it comes’, and fearful) based on women's satisfaction with the quality of antenatal and intrapartum care received. These profiles could be extrapolated to the women interviewed in the present study, as their attitudes towards unforeseen events exhibited similar patterns according to their personal characteristics. Women may therefore benefit from bladder care tailored to their particular attitudes and priorities. A flow chart summarising key characteristics of bladder care drawn from the literature (Figure 4)(Lamb and Sanders, 2016) may help midwives and health professionals to prepare for and engage in bladder care for women in during pregnancy and childbirth.
Limitations
Apart from one participant, all women recruited in this study were Caucasian and originally from the UK. This research could have been enriched by the inclusion of different cultural and ethnic backgrounds. This research encompassed women who had given birth up to 6 months before the interview; hence, some recall and social desirability bias could have been included.
Implications for practice
Best practice implies a proactive delivery of information and the promotion of a healthy bladder during pregnancy, labour, after birth, and beyond. Bladder care represents an essential aspect of a holistic maternity package, and clinicians must incorporate strategies to improve the exploration of potential urinary problems. Special consideration should be given to the standardisation of language used when communicating with women in a direct and unequivocal manner. More detailed information regarding the reasoning behind PFE is needed, as opposed to the current superficial recommendations. Clinicians must be reminded of the physiological changes related to childbirth, particularly in relation to the urinary system and pelvic floor, in order to prepare women.
The findings of this study could be taken further to develop a qualitative improvement strategy focused on health professionals.
Conclusions
Three themes were identified in this study: ‘muddling through to earn “a badge of honour”’, ‘caring for a baby, but who cares for me?’ and ‘Do you speak “bladder language”?’, but the overarching theme was ‘Lack of care’. This study found that bladder care was very limited for women during the antepartum, intrapartum and postpartum periods, although reports of urinary incontinence were frequent. These findings indicate that clinicians should become more proactive in delivering information and promoting bladder health during these periods but that attention needs to be paid to communication methods. A flow chart to encompass key priorities for bladder care is proposed. This study would also suggest that there should be a more prominent focus on maternity bladder care incorporated into pre-registration midwifery education.

