Women experience specific physiological and psychological distress during pregnancy, leading to distinct physical and psychological requirements (Ngai and Chan, 2011; Curtis et al, 2012). This pregnancy related distress may be intensified when pregnant women encounter stressful events and external stressors, running the risk of numerous adverse perinatal and postnatal outcomes, including hypertensive symptoms, pre-eclampsia, gestational diabetes mellitus, preterm birth and low birth weight (Shahhosseini et al, 2015; Staneva et al, 2015).
Over the last decade, infectious diseases have threatened public physical and mental health across the world. The history of devastating environmental disasters with different geographical origins, including Ebola, West Nile encephalitis, severe acute respiratory syndrome (SARS), and avian flu indicate the global effect of infectious epidemics ([World Health Organization [WHO], 2020). Recently, COVID-19, as one of the most detrimental worldwide pandemics, has affected different countries from east to west (WHO, 2020). In terms of the psychological aspect, the response to the COVID-19 pandemic is suggested to be analogous to the response to natural disasters or other similar catastrophic events (Momoi et al, 2020), leading to permanent distress in the affected population (North and Pfefferbaum, 2013). Mental consequences of disasters may persist as long as 12 years in one out of six exposed people (Raker et al, 2019).
Pregnant women are considered a high-risk group for traumatic mental effects of any pandemic disaster risk since the pregnancy related physical and psychological changes as well as the motherhood transition intrinsically induce more maternal stress and anxiety (Lothian, 2009; Chan et al, 2013). Additionally, studies have shown a high mortality rate among infected pregnant women with respiratory infectious diseases (Kourtis et al, 2014). Hemodynamic and pulmonary adaptive changes during pregnancy, including increased stroke volume and heart rate, and reduced pulmonary residual capacity may enhance the risk of hypoxemia contributing to the increased severity of infectious diseases targeting the respiratory system during pregnancy. For example, during the influenza A pandemic in 1957, 50% of the mortality of reproductive-age women was represented by the pregnant population (Cervantes-Gonzalez and Launay, 2010). Also, in the 2009 H1N1 influenza A pandemic, pregnant women experienced more severe symptoms and consequences leading to hospitalisation, intensive care unit admission or mortality, as compared with nonpregnant women and the general population (Mosby et al, 2011). Regarding the COVID-19 infection, according to the recent Centers for Disease Control and Prevention ([CDC], 2020) report, pregnant women are at an increased risk for severe illness from COVID-19, compared to non-pregnant people. This may be explainable considering the cardiopulmonary changes in pregnant population. Additionally, the infected women may experience adverse pregnancy outcomes such as preterm birth (CDC, 2020).
Literature suggests that for coronaviral infections, including SARS and COVID-19, not only the infection itself but also the pertinent treatments are potentially fatal for both mother and the unborn baby (Cottreau and Barr, 2016). Awareness of these poor consequences of previous and present viral infection outbreaks that are from the same family may induce more maternal distress (Goodwin et al, 2015). This distress could be exacerbated when the severity of the potentially fatal consequences of the COVID-19 strain is not well-known yet.
Perceived risk of COVID-19 acquisition
Perceived risk is a determinant factor for the way people perceive, judge and react to the potential risks of specific hazards (Mitchell, 2015). People assess risks using a combination of cognitive-perceptual factors (arguing the evidence, potential damages) and personal emotional appraisals (intuition or imagination) (Kusev et al, 2017). A risk expert, in a review, has identified various confounding factors for risk perception, including risk origin, nature, awareness, cultural diversity (Brown, 2014), specificity, uncertainty and personal impact. According to this review, people are more concerned about risks that are imposed by strangers, man-made, novel, uncertain, personally harmful and affect publicity identified people (Ropeik, 2002). Relying on the aforementioned review, the perceived risk toward COVID-19 acquisition is expected to be significant as it covers most of the aforementioned potential confounding factors. This perceived risk may mediate the association between the COVID-19 pandemic and maternal mental health.
Protective behaviours
Existing research suggests that disease risk perceptions are a critical predictor of health behaviour, although the nature of the association between risk perceptions and health behaviour may be affected by the type and severity of the risk and the accuracy of the perceived risk (Ferrer and Klein, 2015). A piece of meta-analytic evidence demonstrates that affective risk perceptions as the essential determinant of optimal judgment and decision-making are related to protective behaviours (Hay et al, 2006), and those interventions that successfully target these perceptions produce subsequent changes in behaviour (Sheeran et al, 2014). In health decision-making, individuals are expected to navigate choices involving weighing the risk of disease with benefits of action.
Unfortunately, neither in the previous infection outbreaks nor in the worldwide COVID-19 pandemic, have maternal mental health and protective behaviours been well-studied. A study conducted during SARS indicated a higher tendency toward overestimating the risk of SARS, greater state anxiety and more behavioural changes among pregnant women exposed to the outbreak than in the unexposed group (Lee et al, 2006).
The shortage of studies in maternal mental and behavioural health is unsurprising (Topalidou et al, 2020). This is probably because reaching out to the community during an outbreak is unsafe and costly, if not life-threatening. This research is a unique opportunity to study the association between perceived risk toward COVID-19 acquisition and maternal mental distress as well as protective behaviours during the COVID-19 virus infection outbreak.
Method and materials
Design
A cross-sectional study was designed to study the intended association. This study was extracted from an under-process longitudinal cohort study that aimed to study the maternal and neonatal outcome of perceived risk mediated by maternal distress during the COVID-19 outbreak. The target populations were Iranian pregnant women during the COVID-19 outbreak who were recruited (April 2020 to June 2020) from a pool of pregnant women in the electronic health records in the Golestan University of Medical Sciences (Nab software).
Sample and setting
The eligibility criteria included being not infected with COVID-19 (previously or currently), ability to read and write in the Persian language, have accessibility to the internet for online questionnaire completion and not having risk factors that categorise the pregnancy in the high-risk group according to American Pregnancy Association (2020). The participants were excluded and referred to a relevant specialist if they experienced any complication that put the pregnancy in the high-risk category. Those who had severe distress and suicidal ideation were identified based on the cut-off points of the applied scales, then excluded and referred to a psychologist for more evaluation and potential interventions. Other exclusion criteria included not willing for any reason.
Ethics
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects/patients were approved by the Ethical Committee Center of Golestan University of Medical Sciences with an approval number of 111540 and ethic code IR.GOUMS.REC.1399.008.
Procedure
After obtaining institutional review board approval, the list of contact numbers of low-risk pregnant women in the centre was extracted from the e-health system and used for the recruitment. A total of 1 510 participants were called and, finally, 392 completed the questionnaires (Figure 1).
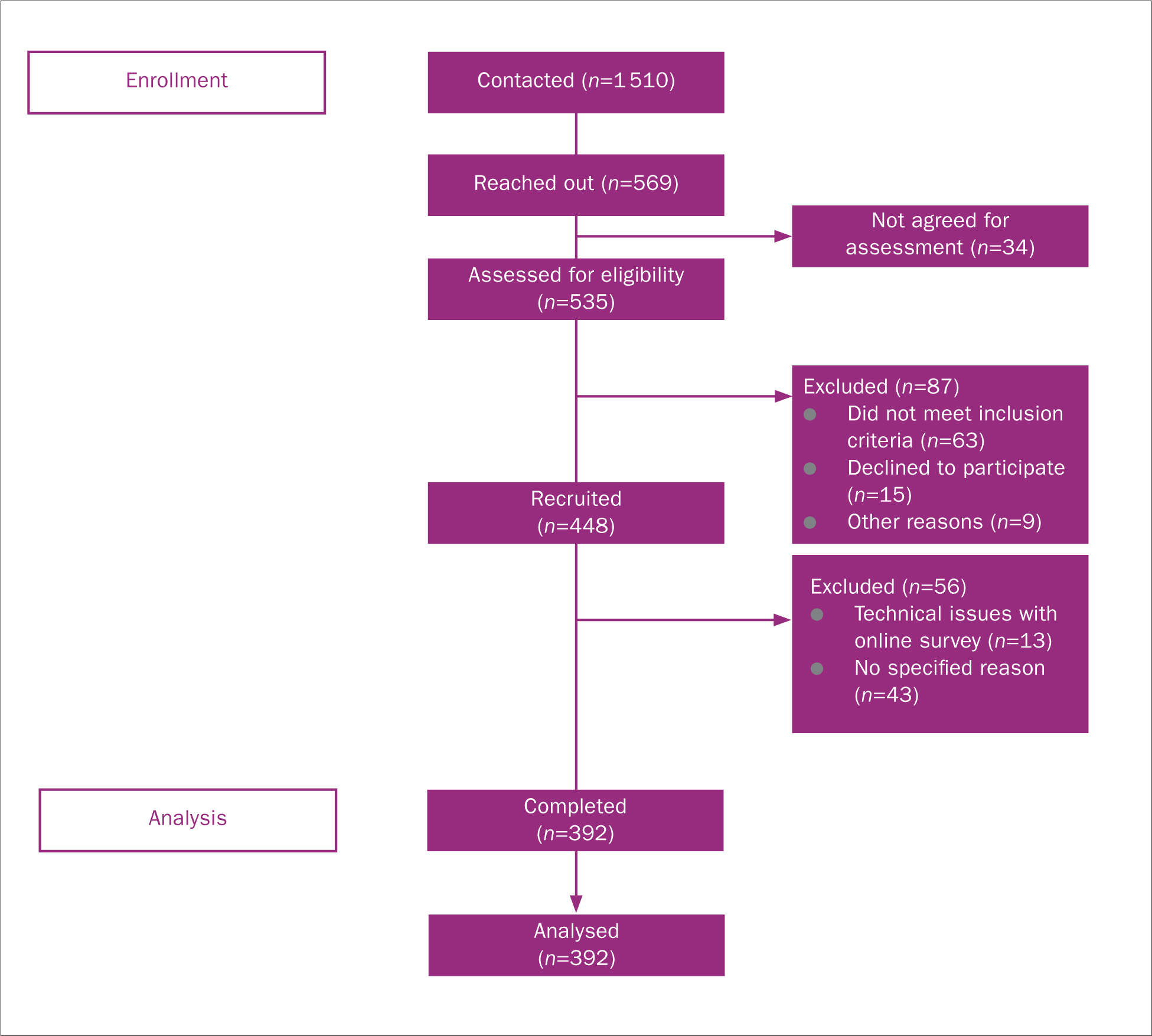 Figure 1. STROBE diagram depicting participant flow
Figure 1. STROBE diagram depicting participant flow
All potential participants were informed about the aim and study protocol. Verbal informed consent was witnessed and formally recorded. Women who met the inclusion criteria and desired participation were recruited by two trained certified midwives using phone interviews among the lists of low-risk pregnant women served in the intended centre. The potential participants were informed that they can leave the study at any time they want. For data assessment, the link related to the collection of online questionnaires were text to them using assigned smart cellphones.
Participants were asked to complete the questionnaires at the recruitment time. We reminded them for the second time by text if they did not complete the questionnaires within two weeks after recruitment. The relevant questionnaires and measures included demographic questionnaire (age, education, job, obstetric history), stress, anxiety and depression scales, as well as two questions assessing risk perception toward COVID-19 and 11 questions regarding the protective behaviours against COVID-19 viral infection. If the participants had severe distress based on the applied surveys, they were referred to a relevant specialist for more examination and treatment. We followed up the cases with severe symptoms once 2-4 weeks after recruitment at the assigned prenatal routine care.
Materials and measures
Perceived stress scale (PSS): for stress assessment, we used the Persian version of the PSS that includes 10 items measuring the frequency of perceived stress over the last month (Cohen et al, 1994). Items were designed to assess an individual's attitudes of her/his life being unpredictable, uncontrollable and overloaded. This five-point scale provides a possible response ranging from 10–50 with a higher score indicating higher stress levels. The possible responses ranged from zero (never) to four (very often). This scale is reliable and valid in various populations across the world, including Iranian (Cronbach's alpha=0.9) (Maroufizadeh et al, 2014; Kashanian et al, 2019).
State-Trait anxiety inventory (STAI): for anxiety assessment, we applied the STAI which consisted of 20 items, to assess the anxiety level following stressful situations. This inventory assesses dimensions, including apprehension, tension, nervousness, worry and activation/arousal of the autonomic nervous system for state anxiety and general states of calmness, confidence and security for trait anxiety. This four-point Likert scale, ranging from one (not at all) to four (very much so), assesses the anxiety experienced in the past weeks (Speilberger et al, 1970). The validated and reliable Persian version was used for this study with a Cronbach's alpha of 0.78 (Bastani et al, 2005). In current study, we applied factor analysis to divide the original scale into two factors, including factor 1 (positive affect: numbers of 1, 3, 6, 7, 10, 13, 14, 16, 19) and factor 2 (negative affect: numbers of 2, 4, 5, 8, 9, 11, 12, 15, 17, 18, 20). The internal consistency within each factor was assessed by Cronbach's alpha to be 0.86 for factor one and 0.84 for factor two.
Beck depression inventory (BDI-13): to assess depression, the Persian version of the BDI-13 was used (Beck and Beck, 1972). Attitudes including depressed mood, pessimism, lack of satisfaction, sense of failure, guilt, self-harm, self-hate social withdrawal, indecisiveness, work difficulty, distorted body image, fatigue and loss of appetite are assessed in this scale. This is a four-point scale from zero (symptom absent) to three (severe symptoms) that is valid and reliable (Cronbach alpha ranged from 0.89–0.94) scale among the Iranian population (Rajabi, 2005; Dadfar and Kalibatseva, 2016).
Risk perception toward COVID-19 acquisition: for risk perception of COVID-19, we used two questions developed in another relevant study (Kwok et al, 2020) including 1) how likely you will be infected by COVID-19 viral infection? 2) how likely your families will be infected by COVID-19 viral infection?. This five-point Likert scale ranging from one (not very likely) to five (very likely) assesses the protective behaviours against COVID-19 acquisition during pregnancy.
Protective behaviours: an 11-item questionnaire which was used in a study in SARS outbreak (Yang and Cho, 2017) was applied for protective behaviours to assess items including shelter in-house, hand washing, preventing hand contact with mucous membrane, avoiding straight contact with people, hand sanitiser application, mask protection, social distancing, unnecessary physician visits, public transportation avoidance, nutrient-rich food and exercise. The possible responses ranged from zero (never) to four (very often).
Sample size
The G-power software version 3.1.9.6 was used for the statistical power of the study. Considering the previous relevant study in the SARS pandemic, we applied a=0.05, power=0.8, proportion p1=0.4, and p2=0.2. The sample size was calculated to be 246 for the original study. However, since we had a chance to study more population, we preferred to recruit more participants (n=392).
Statistical analysis
SPSS version 26 was used for data analysis (SPSS Inc., Chicago, IL, US). The participants' characteristics were summarised in Table 1. The association between exposures and outcome variables were assessed using linear regression analysis in both unadjusted and adjusted models (Table 2 and Table 3). We also used explanatory factor analysis for the anxiety variable to uncover the positive and negative affects that were structured in the original scale (STAI). The Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy and Bartlett's test of sphericity was used to check the eligibility of the data for factor analysis. For this, a principal component approach (PCA) with Varimax rotation was applied to divide the STAI into two meaningful factors (F1: positive affect, F2: negative affect) based on the eigenvalues more than one (the amount of variance accounted for by each factor), and scree plot test (Kline, 1994). Items loading at ≥0.4 were retained for factor clarification and conceptual description. We checked the internal consistency via Cronbach's alpha as a measure of reliability statistics for the created factors. To measure the strength and direction of the linear relationship between pairs of continuous variables including exposure and outcome variables, we used bivariate Pearson correlation (Appendix).
Table 1. Descriptive statistics
| Characteristics | Statistics | |
|---|---|---|
| Age (mean; SD) | (26.72; 4.8) | |
| Education (year) (mean; SD) | (12.7; 3.22) | |
| Gestational age (mean SD) | (24.12; 8.83) | |
| Job (++/N (%)) | ||
| Yes | 47 (12.0%) | |
| No | 345 (88.0%) | |
| Income (N (%)) | ||
| Income (≤2 million Toman) | 331 (84.4%) | |
| Income (>2 million Toman) | 61 (15.6%) | |
| Gravidity (N (%)) | ||
| Primigravida | 162 (41.3%) | |
| Multigravida | 230 (58.7%) | |
| Abortion (N (%)) | ||
| Yes | 58 (14.8%) | |
| No | 333 (84.9%) | |
| Child death (N (%)) | ||
| 0 | 344 (87.8%) | |
| 1 | 35 (8.9%) | |
| 2 | 13 (3.3%) | |
| Trimester (N (%)) | ||
| First | 52 (13.3%) | |
| Second | 176 (44.9%) | |
| Third | 161 (41.1%) | |
| Stress (mean SD) | (26.72; 4.37) | |
| Anxiety 1 (mean SD) | (28.32; 5.54) | |
| Anxiety 2 (mean SD) | (22.50; 5.34) | |
| Depression (mean SD) | (19.96; 4.41) | |
Table 2. Regression analysis in unadjusted and adjusted models for stress and anxiety factor 1 and 2 (n=392)
| Stress | Anxiety factor I | Anxiety factor II | ||||
|---|---|---|---|---|---|---|
| Unadjusted (95%CI) | Adjusted (95%CI) | Unadjusted (95%CI) | Adjusted (95%CI) | Unadjusted (95%CI) | Adjusted (95%CI) | |
| Perceived risk | 1.23 (0.92, 1.53) *** | 0.86 (0.61, 1.10) *** | -1.05 (-1.37, -0.74) *** | -1.09 (-1.43, -0.78) *** | 0.54 (0.22, -0.86)*** | 0.55 (0.23, 0.88)*** |
| Age | 0.13 (0.02, 0.24)* | 0.1 (0.007, 0.2) * | 0.02 (-0.1, 0.13) | 0.03 (-0.1, 0.16) | -0.03 (-0.14, 0.08) | -0.05 (-0.17, 0.08) |
| Education (year) | 0.18(0.02, 0.35) * | -0.008 (-0.05, 0.04) | 0.14 (-0.03, 0.3) | 0.2 (0.02, 0.39) | -0.05 (-0.22, 0.11) | -0.04 (-0.23, 0.14) |
| Job | ||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Yes | 0.73 (-0.9, 2.37) | -0.41 (-1.77, 0.94) | -0.76 (-2.44. 0.93) | -1.19 (-2.96, 0.56) | -0.07 (-1.71, 1.76) | 0.46 (-1.3, 2.23) |
| Income | ||||||
| Income (2 million) | Reference | Reference | Reference | Reference | Reference | Reference |
| Income (>2 million) | 0.8 (-0.66, 2.26) | 0.19 (-1.19, 1.57) | 0.65 (-0.86, 2.16) | 0.56 (-0.94, 2.05) | -0.05 (-1.52, 1.41) | -0.01 (-1.51, 1.49) |
| Gestational age | 0.006 (-0.05, 0.07) | 0.05 (-0.08, 0.19) | -0.03 (-0.09, 0.03) | -0.02 (-0.09, 0.03) | 0.03 (-0.03, 0.09) | 0.03 (-0.03, 0.09) |
| Gravidity | ||||||
| Primigravida | Reference | 0a Reference | Reference | Reference | Reference | Reference |
| Multigravida | 0.32 (31.65, 33.04) | -0.3 (-1.28, 0.68) | -0.59 (-1.7, 0.52) | -0.9 (-2.17, 0.38) | 0.48 (-0.59, 1.56) | 0.35 (-0.93, 1.62) |
| Abortion | ||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Yes | 1.15 (-0.32, 2.62) | 1.14 (-0.15, 2.43) | -0.47 (-2.01, 1.07) | 0.1 (-1.58, 1.8) | 1.63 (0.14, 3.12) * | 0.77 (-0.92, 2.46) |
| Child death | ||||||
| 0 | -3.74 (-6.7, -0.78) * | -1.44 (-3.99, 1.11) | 1.05 (-2.02, 4.12) | 1.1 (-2.22, 4.42) | -3.76 (-6.71, -0.81) * | -3.52 (-6.85, -0.2) * |
| 1 | -3.14 (-6.54, 0.26) | -1.35 (-4.09, 1.4) | 0.83 (-2.7, 4.37) | 1.12 (-2.45, 4.69) | -2.57 (-5.96, 0.82) | -2.7 (-6.28, 0.87) |
| 2 | Reference | Reference | Reference | Reference | Reference | Reference |
Note:
***P-value<0.001,
**<0.01,
*<0.05
Table 3. Regression analysis in unadjusted and adjusted models for depression and protective behaviour (N=392)
| Depression | Protective behaviours | |||
|---|---|---|---|---|
| Unadjusted (95%CI) | Adjusted (95%CI) | Unadjusted (95%CI) | Adjusted (95%CI) | |
| Perceived risk | 0.87 (0.63, 1.12) *** | 0.9 (0.64, 1.15) *** | 0.15 (0.08, 0.22) *** | 0.15 (0.09, 0.22) *** |
| Age | 0.02 (-0.06, 0.11) | 0.01 (-0.09, 0.11) | 0.002 (-0.02, 0.03) | 0.007 (-0.02, 0.03) |
| Education (year) | -0.01 (-0.15, 0.12) | -0.04 (-0.18, 0.1) | 0.002 (-0.03, 0.04) | -0.02 (-0.05, 0.02) |
| Job | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 0.01 (-1.33, 1.35) | -0.05 (-1.46, 1.35) | 0.19 (-0.15, 0.54) | 0.15 (-0.22, 0.52) |
| Income | ||||
| Income (2 million) | Reference | Reference | Reference | Reference |
| Income (>2 million) | -0.2 (-1.41, 0.99) | -0.27 (-1.46, 0.92) | 0.01 (-0.3, 0.32) | -0.02 (-0.33, 0.3) |
| Gestational age | -0.003 (-0.05, 0.04) | -0.01 (-0.06, 0.04) | -0.005 (-0.02, 0.008) | -0.007 (-0.02, 0.006) |
| Gravidity | ||||
| Primigravida | Reference | Reference | Reference | Reference |
| Multigravida | 0.66 (-0.23, 1.54) | 0.63 (-0.39, 1.64) | -0.07 (-0.3, 0.15) | -0.09 (-0.36, 0.18) |
| Abortion | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 1.1 (-0.12, 2.32) | 0.85 (-0.49, 2.19) | 0.05 (-0.27, 0.36) | 0.13 (-0.22, 0.49) |
| Child death | ||||
| 0 | -1.67 (-4.1, 0.77) | -1.24 (-3.87, 1.4) | 0.2 (-0.43, 0.82) | 0.27 (-0.34, 0.97) |
| 1 | -1.45 (-4.25, 1.35) | -1.42 (-4.26, 1.42) | 0.17 (-0.55, 0.89) | 0.25 (-0.5, 1.004) |
| 2 | Reference | Reference | Reference | Reference |
Note:
***P-value<0.001,
**<0.01,
*<0.05
Table 4. Correlation of features
| Risk perception | Stress | Anxiety I | Anxiety II | Depression | Prevention | |
|---|---|---|---|---|---|---|
| Risk perception | 1 | 0.38 *** | -0.31 *** | 0.17 *** | 0.33 *** | 0.23 *** |
| Stress | 0.38 *** | 1 | -0.27 *** | 0.44 *** | 0.43 *** | 0.1 * |
| Anxiety I | -0.31 *** | -0.27 *** | 1 | -0.4 *** | -0.58 *** | -0.24 *** |
| Anxiety II | 0.17 *** | 0.44 *** | -0.4 *** | 1 | 0.59 *** | 0.17 *** |
| Depression | 0.33 *** | 0.43 *** | -0.58 *** | 0.59 *** | 1 | 0.3 *** |
| Prevention | 0.23 *** | 0.1 * | -0.24 *** | 0.17 *** | 0.3 *** | 1 |
Note:
***P-value<.001,
**<0.01,
*<0.05
Results
A total of 392 women was returned a completed questionnaire for a response rate of 87% (completed/recruited) and an average completion time of 15 minutes. The flow of the recruitment of participants and data analysis is specified and reported (Figure 1). As demonstrated in Table 1 (descriptive characteristics), women were 27-years-old on average with 13 years of education history, starting from primary school. About 59% of women were multigravida with a gestational age of 24 weeks on average, with no history of abortion (85%) and child death (88%). They were mostly in the second trimester (45%) or third trimester (41%). About 88% were currently not working and 85% had monthly income less or equal to two million Toman (MT) (equal to US$100 based on the updated rate on 15 July 2020). Total score (mean±SD) for stress (26.72±4.37), anxiety factor 1 (28.32±5.54), anxiety factor 2 (22.50±5.34), depression (19.96±4.41), protective behaviour (11.95±1.13) was measured.
The anxiety variable (STAI) was excellent eligible for factor analysis (KMO statistic=0.92). Considering factors with eigenvalues larger than one and scree plot, our two factors accounting for a total of 51% of the variability were selected. Internal consistency, as assessed by Cronbach's alpha, was 0.86 for factor 1, and 0.84 for factor 2. For the other three outcome variables, we considered the total score without factor analysis.
In unadjusted models, perceived risk of COVID-19 acquisition as the main exposure was highly significant in all five models, including stress (b=1.23, [95%CI:0.92, 1.53]), anxiety factor1(b=-1.05, [95%CI: -1.37, -0.74]), anxiety factor two (b=0.54, [95%CI:0.22,-0.86]), depression (b=0.87, [95%CI:0.63, 1.12]), and protective behaviour (b=0.15, [95%CI:0.08, 0.22]). Variables, including age (b=0.13, [95%CI:0.02, 0.24]), education (b=0.18, [95%CI:0.02, 0.35]), and no child death for (b=-3.74, [95%CI:-6.7,-0.78]) were statistically significant predictors in unadjusted model for stress outcome. Abortion (b=1.63, [95%CI:0.14, 3.12]) had significant association with anxiety factor two in unadjusted model. In all five adjusted models, except for age for stress (b=0.1, [95%CI:0.007, 0.2]) and child death (b=-3.52, [95%CI:-6.85, -0.2]) for anxiety factor 2, perceived risk of COVID-19 acquisition remained highly significant predictor for stress (b=0.86, [95%CI:0.61, 1.10]), anxiety factor 1 (b=-1.09, [95%CI:-1.43, -0.78]), anxiety factor 2 (b=0.55, [95%CI:0.23, 0.88]), depression (b=0.9, [95%CI:0.64, 1.15]), and protective behaviours (b=0.15, [95%CI:0.09, 0.22]).
Correlation of features using bivariate Pearson analysis indicated a statistically significant correlation between pairs of continuous exposure and outcome variables (Appendix).
Discussion
Our results demonstrated that the perceived risk of COVID-19 acquisition in all five models in unadjusted and adjusted models was a statistically highly significant variable predicting maternal mental distress during pregnancy (P<0.001). This increased distress can be due to the vulnerability of the pregnant population that is resulted from cardiopulmonary system adaptations during pregnancy, amplifying the fatal consequences of any infectious disease that targets the respiratory system.
Throughout the pregnancy, pulmonary residual volume decreases leading to increased risk for hypoxia and insufficient gas exchange, especially during the second and third trimesters. Additionally, pregnancy is a critical course for women to be adapted for the motherhood role for a new family member. The transition to motherhood comes with a range of challenges, including emotional, social and financial requirements. Becoming a mother means adjusting to many changes in life and this process of psychological adaptation can place a strain on one's mental health and, in turn, quality of life. Despite its wide negative impact on the wellbeing of pregnant women and their family, the psychological situation of pregnant women during the COVID-19 outbreak is not well studied. Cameron et al (2020) assess the psychological maternal distress during the COVID-19 pandemic indicating that the stress level among mothers of children of different ages varied ranging from 33.16%–43.37%. However, as there is no previous record of the pre-pandemic distress level of participants, the pure COVID-19 impact on current distress is unclear.
According to a rapid response survey, the rate of depression and anxiety among 900 participants, including both pregnant and postpartum women, has increased 25.7% and 43% respectively, as compared with pre-pandemic scores (Davenport et al, 2020). This study is in accordance with our study in terms of the significant indirect and direct effects of the COVID-19 pandemic on maternal mental health. However, the exact variable that may mediate this association needs a conservative assessment as the COVID-19 pandemic is a wide subject containing a various spectrum of personal, social and economical problems, inducing mental distress. Numerous factors play important roles in triggering mental distress during pandemics, including insufficient supply, job loss, financial problems, social isolation, indoor negative discussion with family or partner (Nicola et al, 2020).
Additionally, studies concer ned with the psychological impact of the pandemic often considered the general mental distress during COVID-19 and ignored intended mediators between COVID-19 outbreak and subsequent mental distress that may explain how much current distress is specifically related to the COVID-19 pandemic. This is important, especially if there is no specific scale to assess the COVID-19-induced distress to distinguish it from different sources of distresses. In the current study, we had to use existing general psychological health scales as no validated COVID-19-specific psychological distress scale was available at the time being. However, the application of perceived risk as COVID-19-specific variables helped explain how current mental distress is significantly correlated with COVID-19 outbreak. We also performed adjusted analysis for potential confounding variables, including job and income as additional distress sources during the COVID-19 outbreak. The results showed that of all adjusted variables, only two variables including age and the child death may confound the association between perceived risk of COVID-19 and some components of maternal distress (P<0.05).
Research on the mental status of pregnant women who are home-bound under dramatic effects of an acute epidemic disease seems to be more complicated but still worthy. The emerging studies are mostly focused on either infected individuals or hospital staff who are under the direct impact of the infection. However, investigating the mental and psychosocial effects of the infection outbreaks, including COVID-19 seems to be essential for pregnant women who are under mental pressure of the problem affecting both mother and unborn baby. The results of the studies may be useful to plan for mental support and behavioural regulation in case of future occurrence of any pandemics to help reduce adverse consequences caused by induced perceived risk.
Conclusion
The findings from the current study revealed that pregnant women experience significant mental distress, including stress, anxiety and depression during the course of COVID-19. This distress may also increase the tendency of pregnant women in applying the relevant preventive behaviours against COVID-19 acquisition. Although the application of the behaviours is intrinsically beneficial in the prevention of COVID-19 infection acquisition, it may also amplify mental distress during pregnancy. COVID-19 may be an important additional stress source for pregnant women who already are under the negative effect of various pregnancy induced physical and mental distress. More studies are needed to investigate the impact of the perceived risk toward COVID-19 during pregnancy in different populations. We suggest that clinicians and practitioners consider more precautions regarding the mental tensions that may affect the maternal physical and mental health during pandemics.
Key points
- Pregnant women encounter with mental distress including stress, anxiety and depression during the COVID-19 pandemic
- The perceived risk of COVID-19 infectious disease may increase the mental distress in pregnant women
- The adherence to protective behaviours in pregnant women may be increased due to the increased risk perception toward COVID-19 viral infection acquisition
CPD reflective questions
- What are the potential stress sources for pregnant women during COVID-19?
- What are the potential consequences of the mental dysregulation in pregnant population during COVID-19?
- What are the effective interventions to decrease the increased mental disorders in pregnant population during COVID-19?


