Ankyloglossia, or tongue tie, is a congenital abnormality characterised by a short frenulum, which may restrict tongue motility. It is usually asymptomatic, but in some cases may cause problems during breastfeeding. These problems can be severe enough to make some women give up breastfeeding.
National Institute for Health and Care Excellence (NICE, 2005) guidelines considered frenotomy a safe procedure but highlighted a dearth of evidence of its efficacy in improving breastfeeding practice. Recommendations were made to monitor the outcome of the procedure in terms of successful long-term breastfeeding.
Since these recommendations, several studies have reported varying degrees of effectiveness of frenotomy. Some have shown that frenotomy brings subjective and objective improvements in breastfeeding and reduction in problems related to breastfeeding itself (Buahin et al, 2013; Brookes and Bowley, 2014). A recent retrospective 1-year study on the immediate outcome of frenotomy saw an 80% improvement in the breastfeeding rate immediately after the procedure (Gruber et al, 2013). In a randomised single-blinded controlled trial from 2014, although at 5 days post-frenotomy there was no significant objective improvement in breastfeeding, fewer mothers in the intervention group switched to bottle-feeding (Sutcliffe et al, 2014). A 2012 Dutch observational study saw a breastfeeding improvement of 89% at 1-week follow-up (Post et al, 2012). Timing of frenotomy seems to be important in its effectiveness as perceived by mothers: according to a 2012 cohort survey, frenotomy performed in the first week of life is more effective than if performed subsequently (Steehler et al, 2012). Two systematic literature reviews have found that frenotomy is a safe procedure that improves breastfeeding both objectively and subjectively, but most studies in the literature are not randomised (Constantine et al, 2011; Webb et al, 2013). It is often difficult to determine predictive factors of successful tongue-tie division (Dollberg et al, 2014).
Aims
The primary aim of this study was to assess the outcome of frenotomy. The authors looked at problems experienced by breastfeeding mothers both before and after frenotomy, the complications of the procedure, and the degree of parental satisfaction with the service offered.
Methods
We performed a 1-year retrospective cohort survey, contacting the parents of patients who attended the tongue-tie clinic (TTC) at the Evelina London Children's Hospital from October 2013 to September 2014.
The target population of this clinical service was infants with breastfeeding difficulties and suspected tongue tie. Mothers and infants were referred to the TTC either by the postnatal ward midwives or by health professionals working in the community such as community midwives, breastfeeding consultants, GPs, health visitors, general paediatrics consultants, paediatric surgery consultants and neonatal consultants. When they attended the TTC, every infant's breastfeeding was assessed by an experienced midwife from the breastfeeding team to ascertain that the breastfeeding problems being experienced were not due to positioning or attaching technique and that there was an actual restriction in the infant's tongue movement. Only those infants who had confirmed diagnosis of tongue-tie-related breastfeeding problems underwent frenotomy. After the procedure, the infants and their mothers met the midwife or neonatal nurse again for further support and advice on breastfeeding technique and positioning.
During the survey, three attempts were made, via telephone, to contact every infant's parents. Data were entered on a standard questionnaire for each infant. The first section of the questionnaire asked about breastfeeding methods and problems. Results were collected for three time periods: before the procedure, in the first 48 hours after the procedure, and at the time of follow-up. Breastfeeding problems may include maternal problems, such as breast pain, and issues affecting the feed such as frequent or long feeds, shallow latch, and fussiness or restlessness of the infant.
The second part of the survey collected information about the quality of the TTC service. This included parental perception regarding the information given about the condition, the frenotomy procedure, support during the process and the follow-up. Parents' overall satisfaction with the service was recorded on a Likert-type scale of 1–5, where 1 = not satisfied at all and 5 = very satisfied.
Results
In the period from October 2013 to September 2014, 308 referrals were made to the TTC. Most referrals came from breastfeeding classes and ward and community midwives (Table 1).
| Referrer | Number of referrals |
|---|---|
| Breastfeeding classes | 152 |
| Ward midwives | 74 |
| Community midwives | 27 |
| GPs | 7 |
| Specialist consultants (paediatric surgery, neonatology, general paediatrics) | 7 |
| Self-referral | 5 |
| Health visitors | 1 |
| Private lactation consultants | 1 |
| Unknown | 34 |
| Total | 308 |
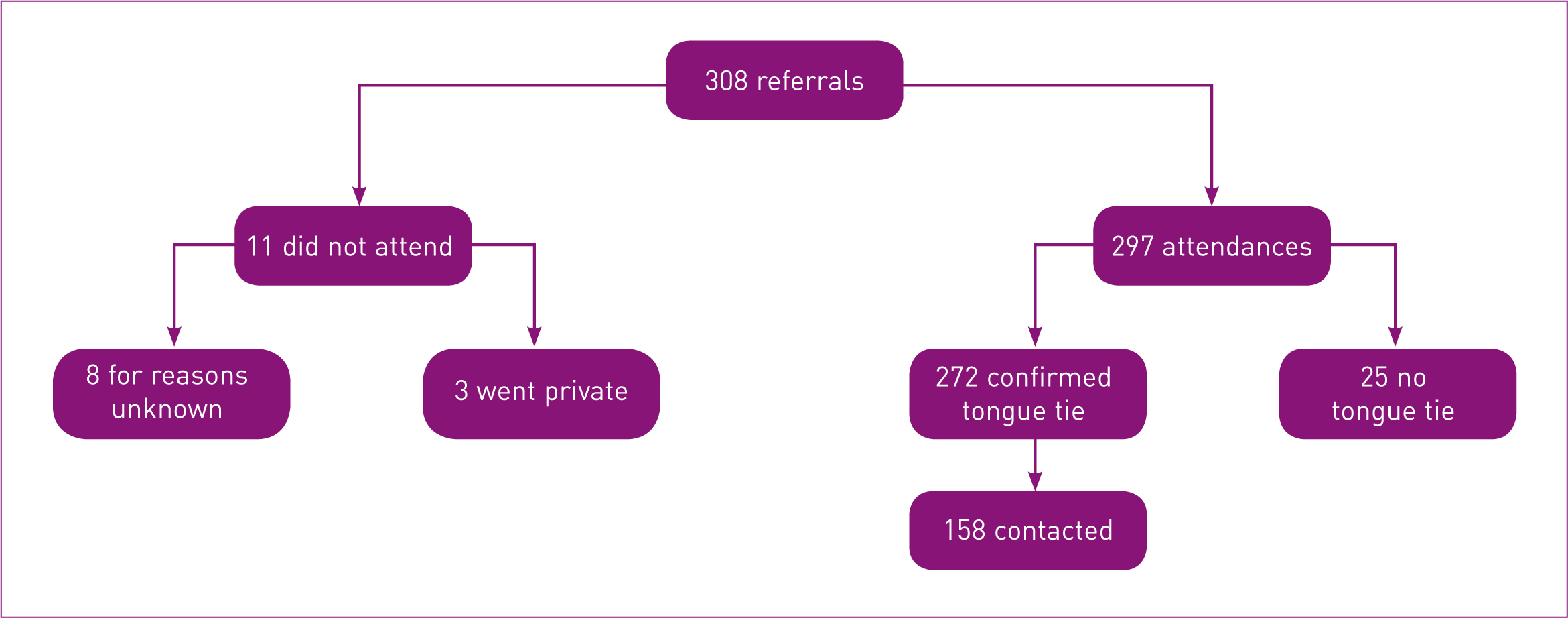
Of the 308 infants referred, 11 did not attend. Of the 297 cases that attended the clinic, in 25 infants no tongue tie was found, while a diagnosis of tongue tie was confirmed in 272 infants. We got complete follow-up data on 158/272 infants, as not all parents responded to the questionnaire (Figure 1).
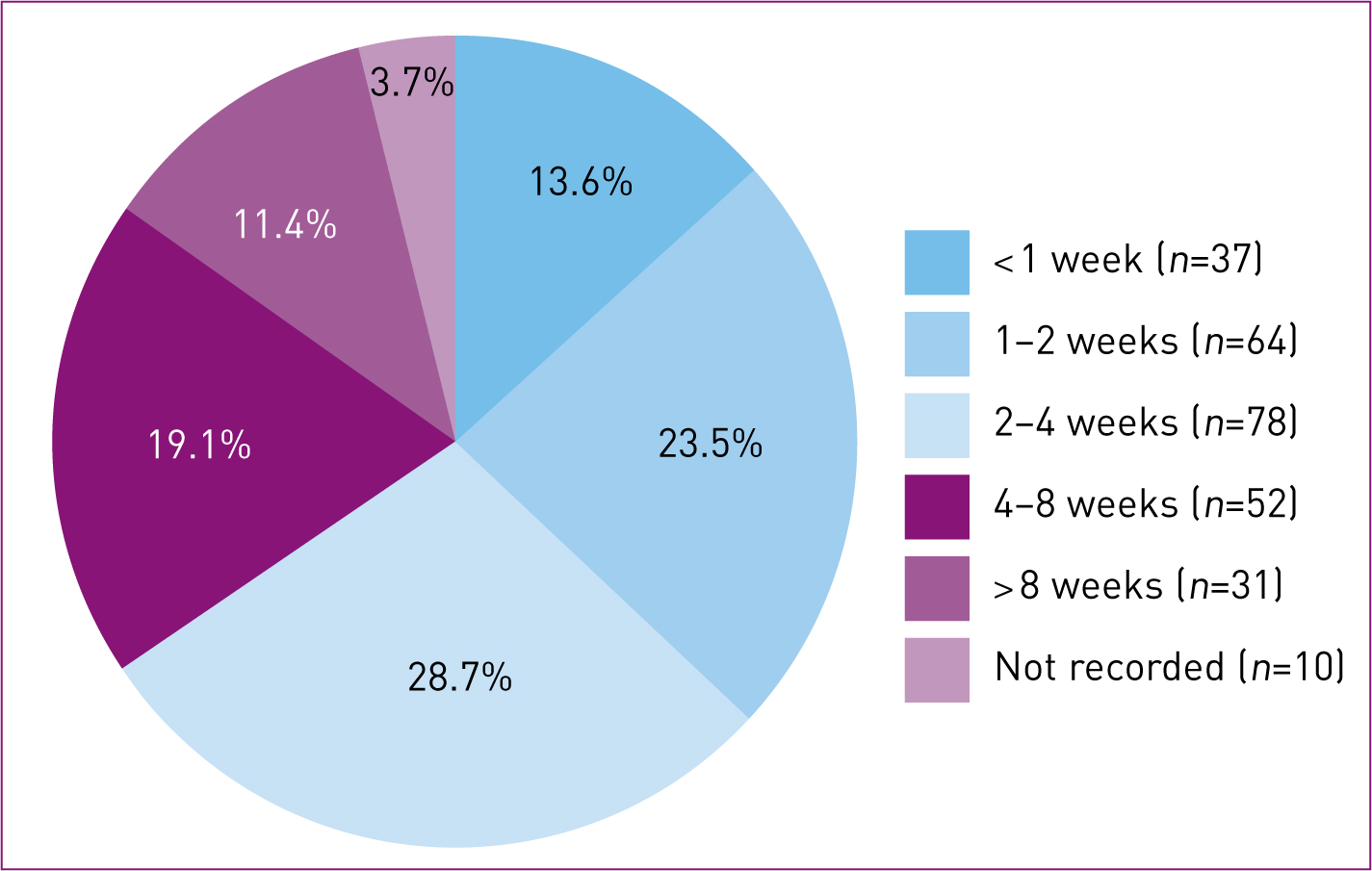
Age at the time of procedure
Among the 272 infants who attended the TTC, more than 50% of the infants were aged between 1 week and 4 weeks at the time of the frenotomy procedure, and in two thirds of cases the procedure was performed in the first 2 months of life. For 10 infants (3.7%) the age was not recorded and it was not possible to retrieve demographic details (Figure 2). The age at the time of procedure ranged from 1 day to 5 months (median 2 weeks).
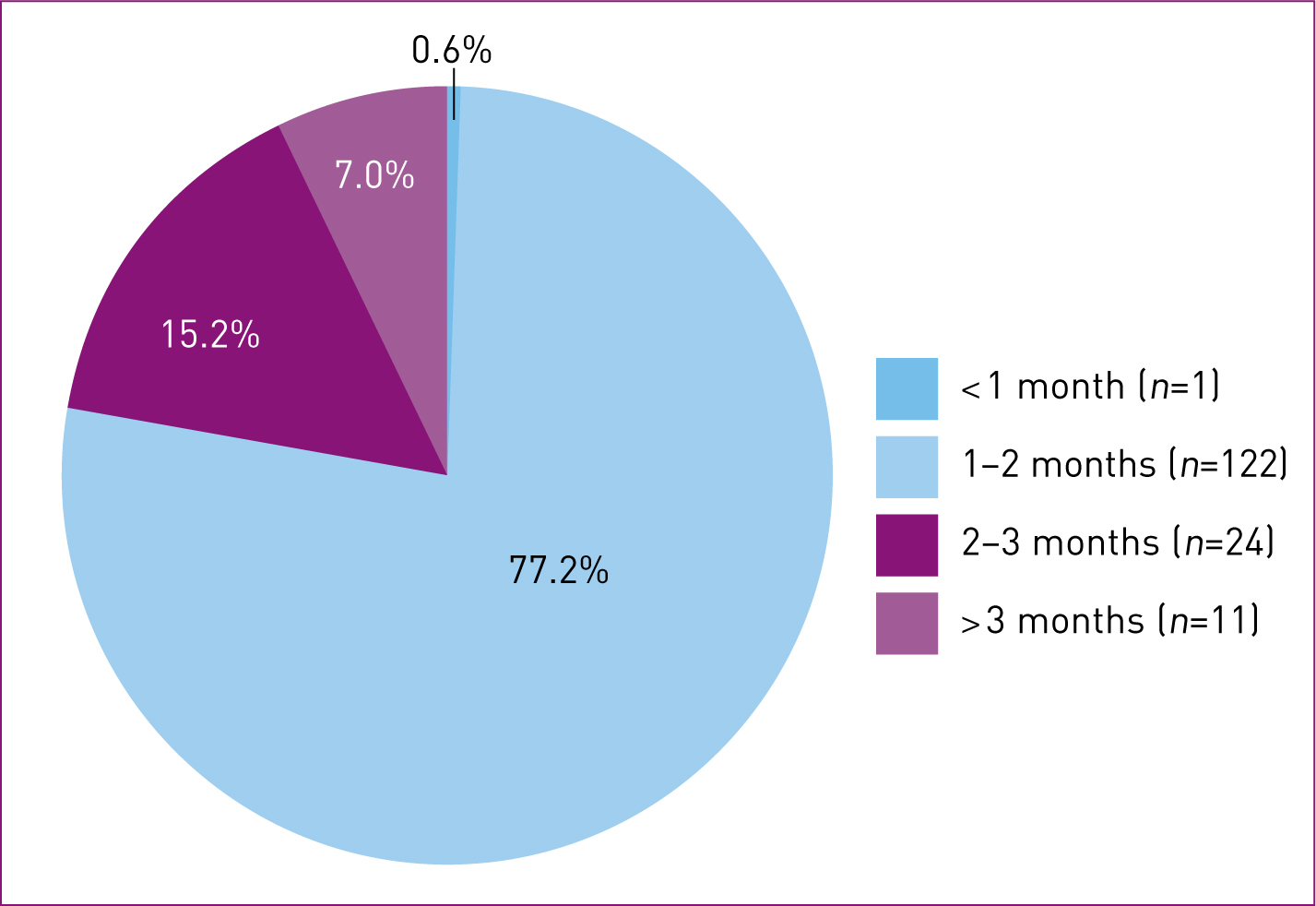
Age at the time of the telephone survey
Only one infant (0.6%) was younger than 1 month when the authors contacted parents for the telephone survey. Most infants were younger than 3 months at the time of follow-up. The age range was between 2 weeks and 9 months (median 4 months) (Figure 3).
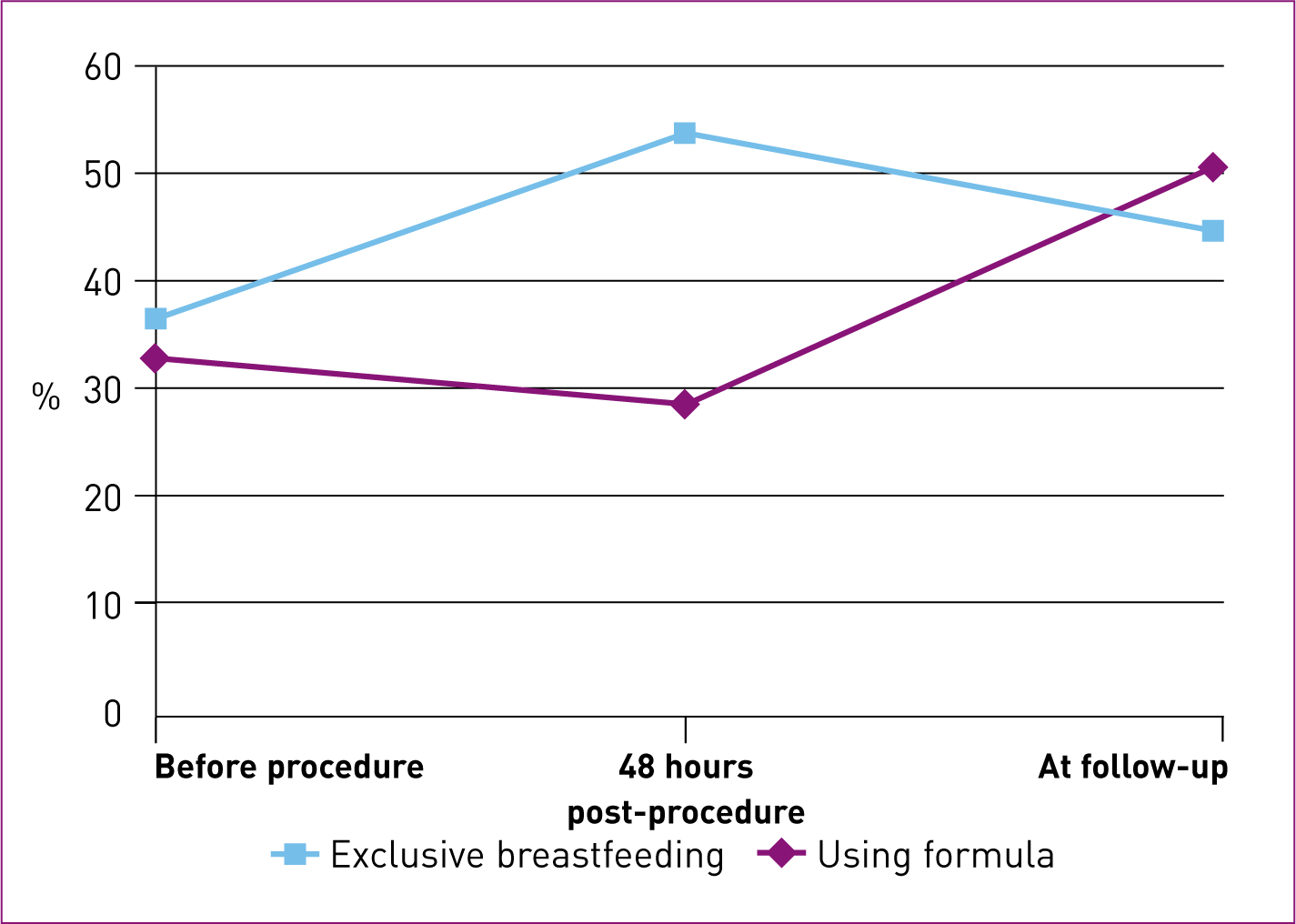
Feeding method
Rates of exclusive breastfeeding and formula feeding are shown in Table 2. There was a statistically significant increase in the exclusive breastfeeding rate from before frenotomy to 48 hours after the procedure (P < 0.0001, OR = 4.857, 95% CI 2.120–12.983). The decrease in formula milk use from before to 48 hours post-procedure was not statistically significant (P = 0.2812, OR = 0.632, 95% CI 0.280–1.370) (Figure 4).
| Exclusive breastfeeding | Formula use | |
|---|---|---|
| Before procedure | 58 | 52 |
| 36.7% | 32.9% | |
| After 48 hours | 85 | 45 |
| 53.8% | 28.5% | |
| Follow-up (median: 4 hours) | 71 | 80 |
| 44.9% | 50.6% |
Figures do not add up to 158 as some babies were fed a combination of breast milk and formula
Breastfeeding problems
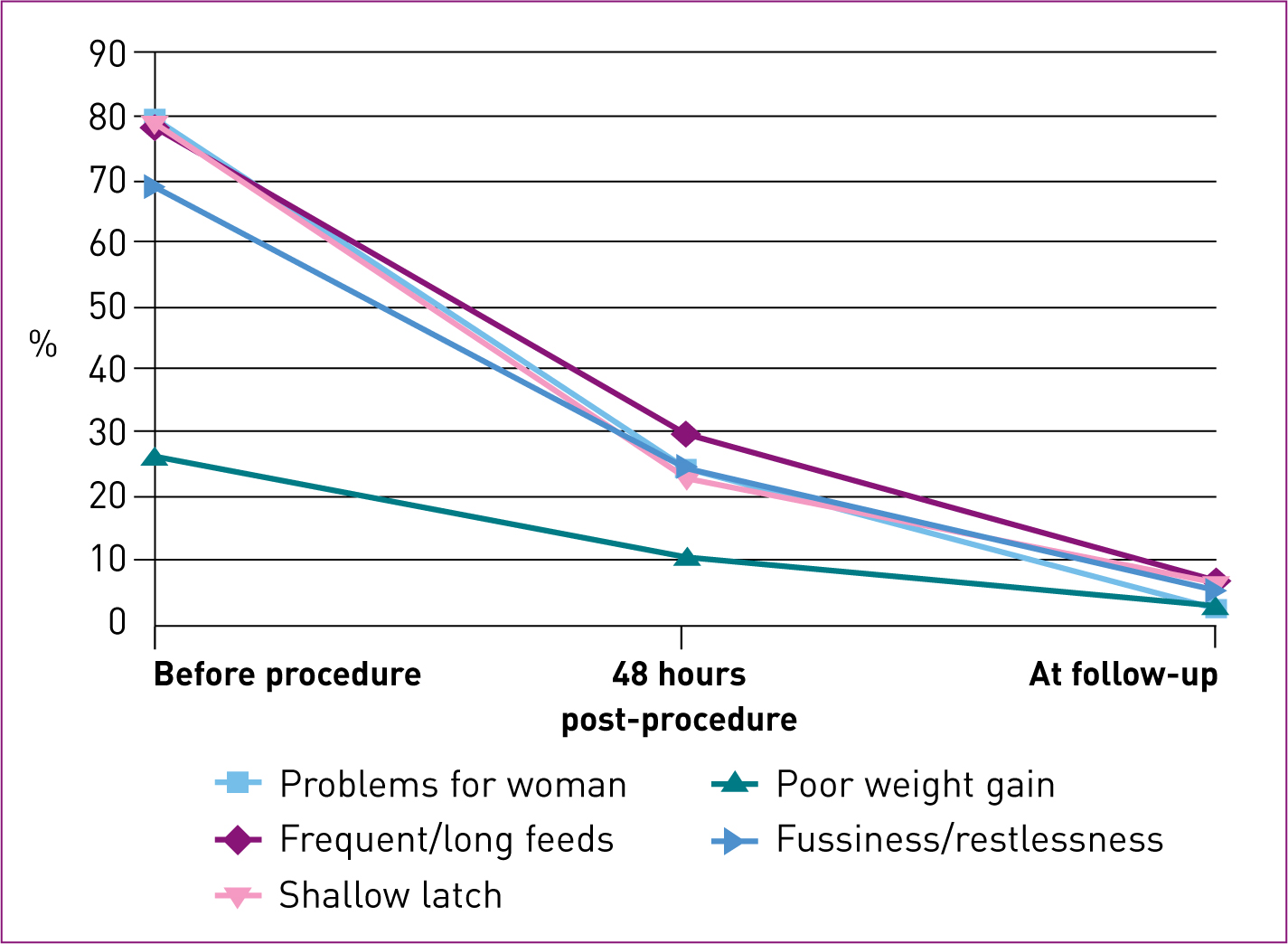
The number of infants exclusively or partially breastfed was 149/158 (94.3%) before frenotomy; the remaining 9/158 (5.7%) had never been able to establish breastfeeding and hence were unable to comment on breastfeeding-related problems. At 48 hours post-procedure, 147/158 (93.0%) were breastfeeding, and at the time of follow-up 113/148 (76.4%) were continuing to breastfeed. The authors reviewed breastfeeding-related problems only in those women who were breastfeeding their infants. Rates of reported breastfeeding problems showed a decrease from before the procedure to 48 hours post-procedure, and had further reduced by follow-up (Table 3) (Figure 5).
| Before procedure (n=149) | After 48 hours (n=147) | Follow-up (median: 4 months) (n=113) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Problems for woman e.g. breast pain, cracked nipples | 118 | 79.2 | 36 | 24.5 | 3 | 2.7 |
| Frequent/long feeds | 116 | 77.9 | 44 | 29.9 | 8 | 7.1 |
| Shallow latch | 118 | 79.2 | 34 | 23.1 | 7 | 6.2 |
| Fussiness/restlessness | 102 | 68.5 | 36 | 24.5 | 6 | 5.3 |
Pain
Reduction in the rate of maternal breastfeeding problems from before frenotomy to 48 hours after the procedure was statistically significant (P < 0.0001, OR 0.013, 95% CI 0.000–0.074).
Frequent/prolonged feeds
Post-frenotomy there was a significant reduction in the rate of women reporting frequent or prolonged feeds (P < 0.0001, OR 0.027, 95% CI 0.003–0.101).
Shallow latch
There was a statistically significant decrease in the rate of shallow latch at 48 hours post-procedure (P < 0.0001).
Fussiness at the breast
The rate of women who reported fussiness of their infants at the breast significantly decreased following frenotomy (P < 0.0001).
Complications
No cases of major bleeding, infection or ulceration were reported. Five infants were brought back to the clinic with persistent breastfeeding problems following the first procedure. One infant attended the clinic four times with persistent breastfeeding problems and required a total of three procedures. Two infants re-attended once and underwent a second procedure. One infant attended twice for persistent breastfeeding problems after the procedure, but no residual or persistent tongue tie was found on the second occasion. One infant re-attended twice and underwent a second frenotomy procedure, and no tongue tie was found at the time of the third visit.
Quality of service
When asked about the quality of the service offered, 93.7% of parents (n = 151/161, including repeated procedures) said they received enough information about ankyloglossia and frenotomy prior to the procedure, 96.8% (n = 156/161) felt supported in giving their consent to the procedure, and 79.1% (n =125/158, as repeated procedures were not included) remembered receiving information on follow-up plans and on what to do in case of problems before leaving the clinic. A total of 120 parents (75.9%) said they were very satisfied with the TTC service (scored 5/5), 22 (13.9%) gave a score of 4/5, 10 parents gave 3 out of 5, while only five parents (3.2%) said they were unsatisfied with the quality of service (four (2.5%) scored it 2/5 and one (0.6%) gave 1/5). One parent said she was unable to give a satisfaction score to the service.
Discussion
The results show that frenotomy is a safe surgical procedure accompanied by a very low complication rate, as has already been described in previous studies (Constantine et al, 2011; Webb et al, 2013).
We saw a significant increase in the exclusive breastfeeding rate and a significant reduction in breastfeeding-related problems at 48 hours post-procedure. There was a substantial drop in the breastfeeding rate and increase in formula use at the time of follow-up. However, the authors have not statistically analysed this because it may be influenced by various factors (e.g. weaning, woman going back to work, lack of family and/or community support), which have not been considered in this study.
We also have not analysed the rate of breastfeeding problems at the time of follow-up. Although these rates are all low, the authors surmised that this is to be expected at about 4 months of age, as it is unlikely that women experiencing major problems would continue breastfeeding for this length of time. Furthermore, a decrease in the rate of problems after this amount of time may be a result of other factors not directly related to the effect of frenotomy.
Limitations
This study is limited by being a single-centre retrospective cohort study, and by the non-standardised, subjective nature of the questionnaire. We know that breastfeeding is a complex process and that several factors—physical, social, financial, emotional and educational—have an important role to play in infant-feeding decisions. A detailed study of these factors would help to elucidate the reasons for the resumption of formula-feeding after the initial significant improvement in breastfeeding rates.
Conclusion
In light of the safety of the procedure and its effectiveness in resolving a range of breastfeeding-related problems and increasing the rate of exclusive breastfeeding, the authors believe frenotomy should be offered to all infants with ankyloglossia who are experiencing breastfeeding problems. More research is needed to ascertain the reasons that, despite a significant initial success, there is a decrease in breastfeeding and increase in use of formula during the weaning period.
Key Points
Conflict of interest: The authors have declared no conflict of interest.

