The relationship between the Jane Crookall Maternity Unit on the Isle of Man and the University of Salford developed when midwives from the island accessed the post-qualifying Examination of the Newborn module. The aim of the new practice placement was to enable midwifery students to experience continuity models of care and provide increased mentorship opportunities for midwives who were undertaking the mentorship module. In addition, the students would have the unique opportunity to experience midwifery care and practice in an island setting.
Health Education North West was supportive of the university extending its placement network within the existing funding, so a visit was undertaken by the academic team to make plans. Prior to commencement of the first placement, a meeting took place with the senior midwives and mentors to provide a mentor update session, audit the placement (Nursing and Midwifery Council, 2008) and plan the experience for students. It was agreed that a placement of 3-4 weeks would facilitate a full range of exposure to care throughout the childbirth continuum, allowing the students to follow the women's journeys in a caseloading model that provides continuity of care. The Salford University practice assessment documents support and record the learning experience with competencies and statutory experiences being signed off by the mentors. The head of midwifery ensured that free accommodation was made available, but travel expenses were to be met by the students. This potential limitation may prevent some students from accessing this opportunity.
Jane Crookall Maternity Unit
The Jane Crookall Maternity Unit is the only maternity unit on the Isle of Man, with 51 practising midwives and four consultant obstetricians providing care to between 750 and 900 women annually. The unit comprises a 17-bed antenatal and postnatal ward, and a delivery suite with four birthing rooms, a pool room and an obstetric theatre. In the event of clinical indication, in-utero transfers to the UK are facilitated (Isle of Man Government, 2015).
Selection of students for the placement
Students who are in their second or third year of the BSc Hons Midwifery programme are eligible to access this placement. Those who wish to be considered are invited to submit a rationale to support their request and identify their proposed learning outcomes. The students demonstrate a clear understanding of the educational opportunities available to them in the following quotations:
‘Professionally, I would like to experience working in a small team of 51 midwives, with a birth rate of 900 compared to my training Trust which conducts around 4000 births a year. I will be interested to see if a smaller caseload increases the continuity of care women and their families receive, also the challenges working on a island presents.’ (Student 3)
‘My current placements are within a busy acute hospital… however, I am interested to experience midwifery in a smaller community setting. I would be willing to use both my current knowledge with the skills I observe in the Isle of Man to shape my future practice.’ (Student 1)
‘To represent Salford University Midwifery Department and to encourage links with maternity services that could enhance learning opportunities in the future.’ (Student 2)
Value for students: continuity of care
The NMC (2009) mandates that student midwives have the opportunity to experience continuity of care through caseloading practice. Studies show where students experience continuity models of care as part of their clinical experience, it enhances their competence and confidence and prepares them for future practice (Rawnson et al, 2011). Gray et al (2013) also reported students developing confidence in their skills in following women throughout the childbearing journey. Similarly Carter et al (2015) found that embedding students within continuity models of care contributes positively to their learning and students feel fulfilled and inspired by their experiences as student testimonials demonstrate:

‘Being able to provide women with full continuity of care throughout is a privilege and a great experience as a student midwife.’ (Student 3)
‘I was involved in my ideal philosophy of care, providing continuity and being able to deliver women-centred care.’ (Student 1)
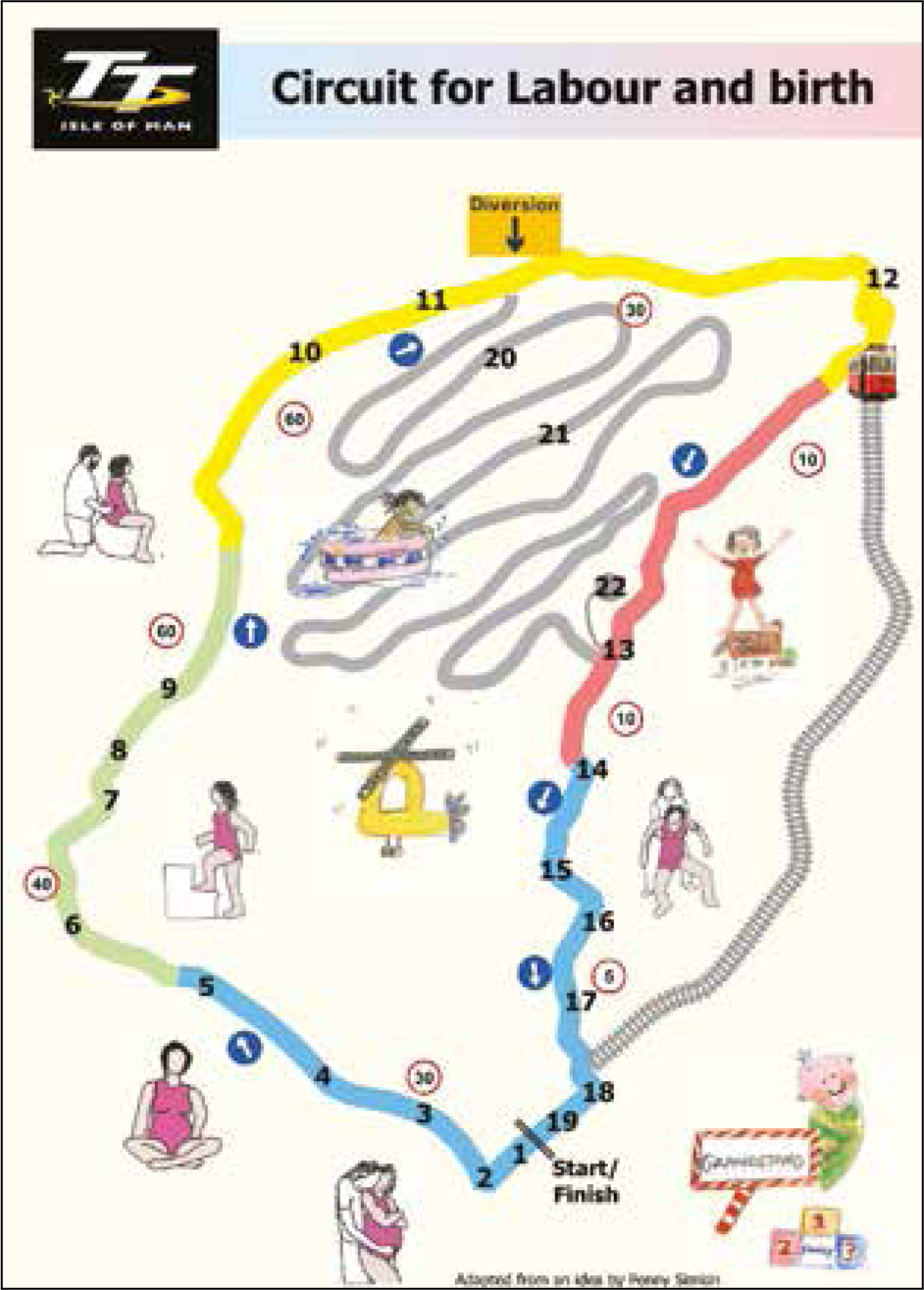
Students were particulary impressed with the Circuit for Labour and Birth developed by midwives at the maternity unit (Figure 1) based on the Isle of Man Tourist Trophy (TT) world-renowned racing course. This journey undertaken by women on the island resonated with them to the extent that they created a poster including representation of their student ‘circuit’ or journey on the island (Table 1).
| 1 | A three-week placement on the Isle of Man during second or third year, does not have to be during free allocation |
| 2 | How to get there: ferry (on foot or by car) or fly (45-minute flight) |
| 3 | Free accommodation arranged for you: nurses' home in Douglas—close to the town centre and beach |
| 4 | Single private room with free Wi-Fi and washing/drying facilities, in-house cleaners, shared bathrooms and kitchens |
| 5 | Welcome pack on arriva |
| 6 | Place of work: Jane Crookall Maternity Unit at Nobles Hospital in Douglas |
| 7 | Midwifery team: head of midwifery Jane Sloane and sign-off mentors Kirsty and Anne-Marie |
| 8 | Warm and friendly welcome |
| 9 | Provide hands-on care, not just observation |
| 10 | Practice competencies completed |
| 11 | Opportunity to deliver a Manx baby! |
| 12 | Four delivery rooms, one pool room, one theatre, combined antenatal/postnatal ward. Integrated service |
| 13 | Daddy daycare classes |
| 14 | Participate in parentcraft and aquanatal classes |
| 15 | Opportunities for in-house training, e.g. suturing and epidural workshops |
| 16 | Spend time with the community team, extended visits till 28 days |
| 17 | Close-knit community |
| 18 | Time off to explore the island, scenic walks, tourist attractions |
| 19 | Multidisciplinary team working and referrals |
| 20 | True continuity of care encouraged |
| 21 | Missing home? Flexible shifts to allow for visitors or flights back to the UK |
| 22 | Enhance your portfolio while representing Salford University |
Developed by Karen Boylan, Jane Cockroft, Lesley Graham and Carly Gunn-Anderson
Mentorship: value for practitioners
Midwives are professionally obliged to complete an approved mentor preparation programme to be an accredited mentor and contribute to an environment conducive to learning (NMC, 2008; Murray et al, 2010; Walsh, 2010). Studies show that mentors value their mentoring role in clinical practice and consider themselves vital in the delivery of the practical component of the midwifery programme (Moran and Banks, 2016). This was supported by testimonials from the Isle of Man mentors who said that they found it rewarding to see a student qualify and then practise knowing that they had participated in that student's training or development:

‘Privileged to be part of the cycle of passing on the narrative of midwifery knowledge.’ (Midwife 1c)
‘Thrilled to have students involved.’ (Midwife 2a)
‘I feel the students have enhanced our unit and all the midwives look forward to them coming. It is lovely to see their enthusiasm and it has made the unit have a fresh feel as the midwives here are beginning to look at midwifery through the fresh eyes of the students. The students we have had so far have been a credit to your university. They are keen to learn and asking their question has made us revalue our practice.’ (Midwife 3)
Value for women
The literature also highlights the value of continuity models of care from the parents' perspective. Williams et al (2010) reported high levels of maternal satisfaction and value associated with continuity of care. Aune et al (2012) found that when students provided continuity of care, parents viewed the relationship as therapeutic and they felt connected with the student. This enhanced their sense of trust and women felt self-confident and empowered by their experiences. This is evident in the students' comments, the service-user case studies presented below and the views of the midwives:
Women ‘Feel this benefits women as it improves service for them.’ (Midwife 1d)
‘Heard a comment “the student was absolutely fantastic”.’ (Midwife 2c)
Parents' perspectives
Vignette 1
Hattie: first baby, accompanied by partner, admitted as an induction of labour, epidural, artificial rupture of membranes, Syntocinon infusion, emergency caesarean failure to progress, cared for all day by student and midwife.
Hattie was reluctant to have a student involved at first, unsure and nervous as this was her first baby. ‘She was fantastic. Examinations had to be repeated by the midwife but she was lovely and kind and nice to talk to—squeezing my hand. It meant there was a second person, with more time to dedicate. I couldn't thank her enough—stayed with me all the time and talked me through the caesarean section. She made the experience 100% better, extra time and attention, talking to you.’
Vignette 2
Kate: first baby, accompanied by partner, ventouse birth and manual removal of placenta, student midwife cared for woman and partner with the midwife all day.
Partner said he ‘didn't think of her as a student, she was part of the team. Someone who was always there, could ask her anything, she appeared competent and answered all questions. The only thing she didn't know was where some of the equipment was, but it was her first day.’ When Kate was taken to theatre, the baby was left with dad. He was impressed that the student came to update him and say goodbye at the end of the shift; she had noticed he was worried so she stayed to offer further reassurance and get further updates beyond her shift time: ‘acting well beyond the call of duty.’ Kate was impressed that she offered her lots of choices on leaving theatre, including whether to have the baby on her own for a while or to bring waiting family in, which was very insightful.
Conclusion
This article highlights the positive experiences of the University of Salford student midwives on the Isle of Man. It is evident that the students, mentors and service-users benefitted from this innovative placement opportunity. The students have gained from a flexible approach to practice learning, being able to follow the family through to discharge into the community, and the opportunity to learn new skills and take an active role in the unit. They have also benefitted the staff and families with their knowledge. The mentors enjoyed facilitating the learning of a diverse group of students, and service users have provided personal insights into the impact of receiving continuous care from a student midwife.

