In the UK, one in three births between 2022 and 2023 resulted in a caesarean section (NHS Digital, 2023). For subsequent pregnancies, women/pregnant people who have had a caesarean section must decide whether to plan for an elective repeat caesarean or consider a vaginal birth (National Institute for Health and Care Excellence (NICE), 2023; NHS, 2023). The current success rate for vaginal birth after a previous caesarean section is 72–75% (Royal College of Obstetricians and Gynaecologists, 2015; NHS, 2023) although recent data from the national maternity and perinatal audit (Healthcare Quality Improvement Partnership (HQIP), 2022) clinical report indicate that the rate for England and Wales is 60%.
There is strict guidance on whether a vaginal birth after a previous caesarean section is in the best interests of both mother and child (NICE, 2023). Clinical guidance advocates thorough counselling for this cohort because of the risks associated with each mode of birth. Yet, there is no current standardised, national structure for advice, which can often vary between healthcare professionals (Fitzpatrick et al, 2019). During 2022–23, there were 547 244 births in the NHS, 210 492 of which were via caesarean section (NHS Digital, 2023; NHS, 2023). This equates to 38%, which is higher than the NICE (2023) guidance suggestion of 25–30%. This is a significant number of people potentially requiring informed and holistic tailored guidance on subsequent mode of birth options. The aims of this study were to examine whether there was an increased risk of adverse neonatal outcomes in women/pregnant people who elected to have a vaginal birth after a previous caesarean section, compared with those who choose to have an elective repeat caesarean section, in one NHS trust, providing local and meaningful data.
Methods
A retrospective cohort design was used to compare data from women/pregnant people who elected for a vaginal birth after previous caesarean section to those opting for elective repeat caesarean section. The study setting was one NHS hospital based in Kent. Data were examined over a period of 12 months from two sources that contain routinely collected patient data: E3 (a specialist maternity system) and BadgerNet (neonatal system). The study population comprised all women/pregnant people with a history of one previous lower segment caesarean section of a live singleton birth. Data included 5471 births during this period. The inclusion/exclusion criteria are shown in Table 1. A total of 392 births were included in the sample.
Table 1. Inclusion and exclusion criteria for study sample
| Inclusion | Exclusion |
|---|---|
| Parity 1 | Multiparity (<1) |
| Previous lower segment caesarean section | Previous caesarean section with inverted T uterine incision |
| Singleton pregnancy | Multiple birth |
| Cephalic presentation | Unstable/breech presentation |
| Term (37–42 weeks) gestation | Prematurity (<37 weeks' gestation)Post-maturity (>42 weeks' gestation) |
| Aged 18 years and over | Aged 17 years or under |
| No fetal anomalies (detected via ultrasound screening and blood tests during pregnancy) | Any antenatal detected fetal anomalies |
| No underlying medical disorders | Maternal comorbidities: diabetes, hypertensive disorders, epilepsy, medical history that may predispose to neonatal health issues/risks to the baby or identified fetal anomalies |
| Previous uterine surgery |
Data analysis
Data analysis was carried out in three stages. First, descriptive statistics were explored for the entire sample. Second, logistic regression was used to examine Apgar scores at 5 minutes (points scoring depending on physical health of the neonate; heart rate, respiratory effort, muscle tone, response to stimuli and skin colouration/perfusion) and neonatal unit admissions between the two groups (intended vaginal birth and intended elective repeat caesarean). Finally, further descriptive analysis was carried out to explore the characteristics of neonatal unit admission in relation to intended mode of birth.
Ethical considerations
Ethical approval for this study was granted by the ethics committee of the University of Greenwich (UREC/SREP-EH&HS-20-21M01-02.07.01) and the local NHS trust. This permission was granted on the 26 November 2020.
Results
Descriptive statistics
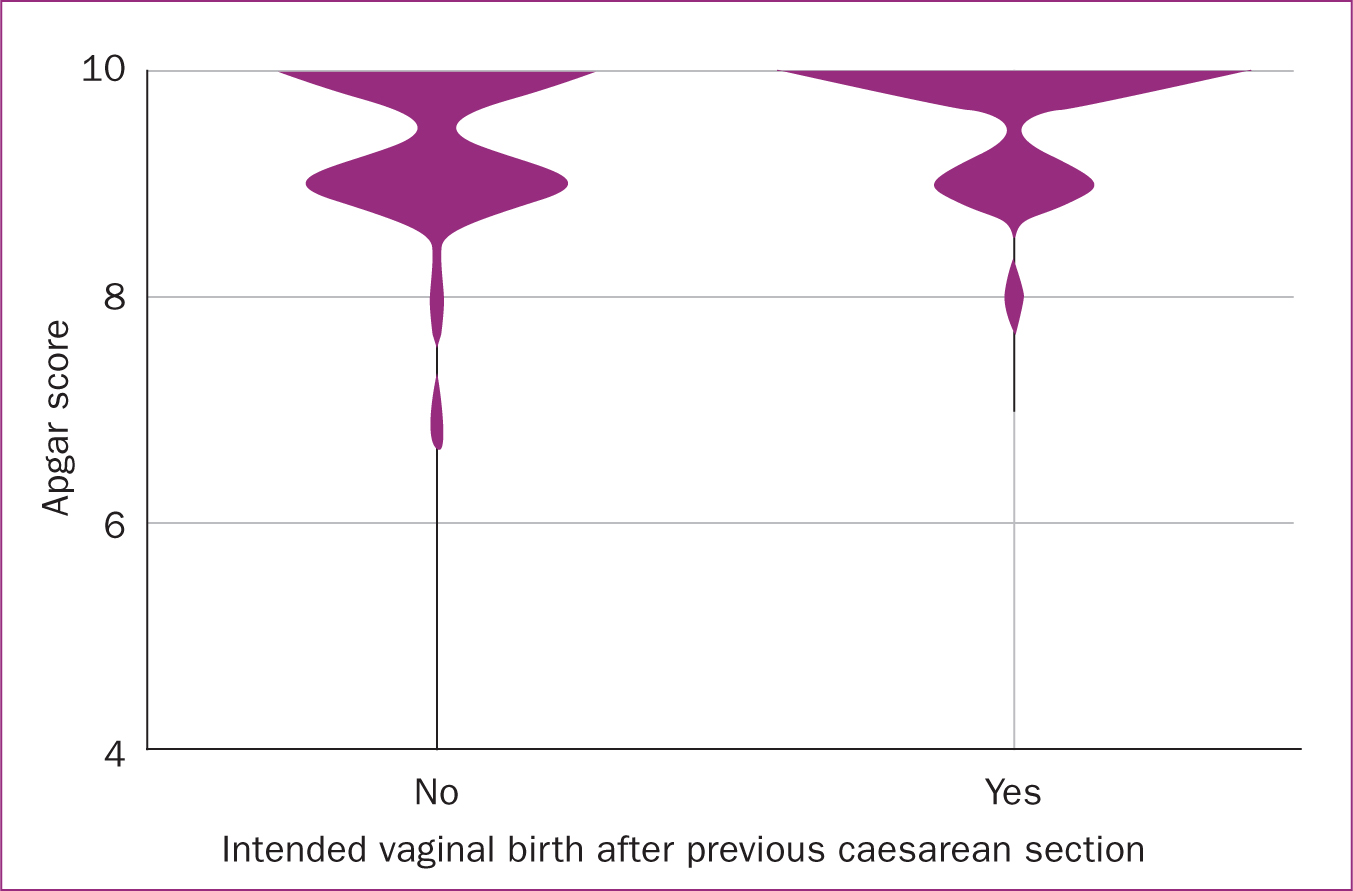
The sample contained 392 births, of which 266 were intended elective repeat caesarean sections, compared to 126 intended vaginal births. Their descriptive statistics are shown in Table 2. The majority of women/pregnant people (n=361; 92%) achieved their intended mode of birth, with only 6% (n=16) of intended elective repeat caesarean section and 37% (n=46) of intended vaginal birth after caesarean having an emergency caesarean section. The overall mean Apgar score at 5 minutes was 9.52 (standard deviation=0.68) for the sample. Apgar scores were slightly higher among the vaginal birth after caesarean group (mean=9.7, standard deviation=0.56) compared to the elective repeat caesarean group (mean=9.44, standard deviation=0.72).
Table 2. Descriptive statistics for mode of birth
| Birth | Mean Apgar score (standard deviation) | Neonatal unit admissions (%) | |
|---|---|---|---|
| Intended vaginal birth | Yes (n=126) | 9.52 (0.67) | 11 (8.7) |
| No (n=266) | 9.52 (0.67) | 16 (6.0) | |
| Actual birth | Vaginal birth (n=80) | 9.70 (0.56) | 6 (7.5) |
| Elective repeat caesarean (n=250) | 9.44 (0.72) | 15 (6.0) | |
| Emergency caesarean (n=62) | 9.61 (0.67) | 6 (9.7) |
Logistic regression
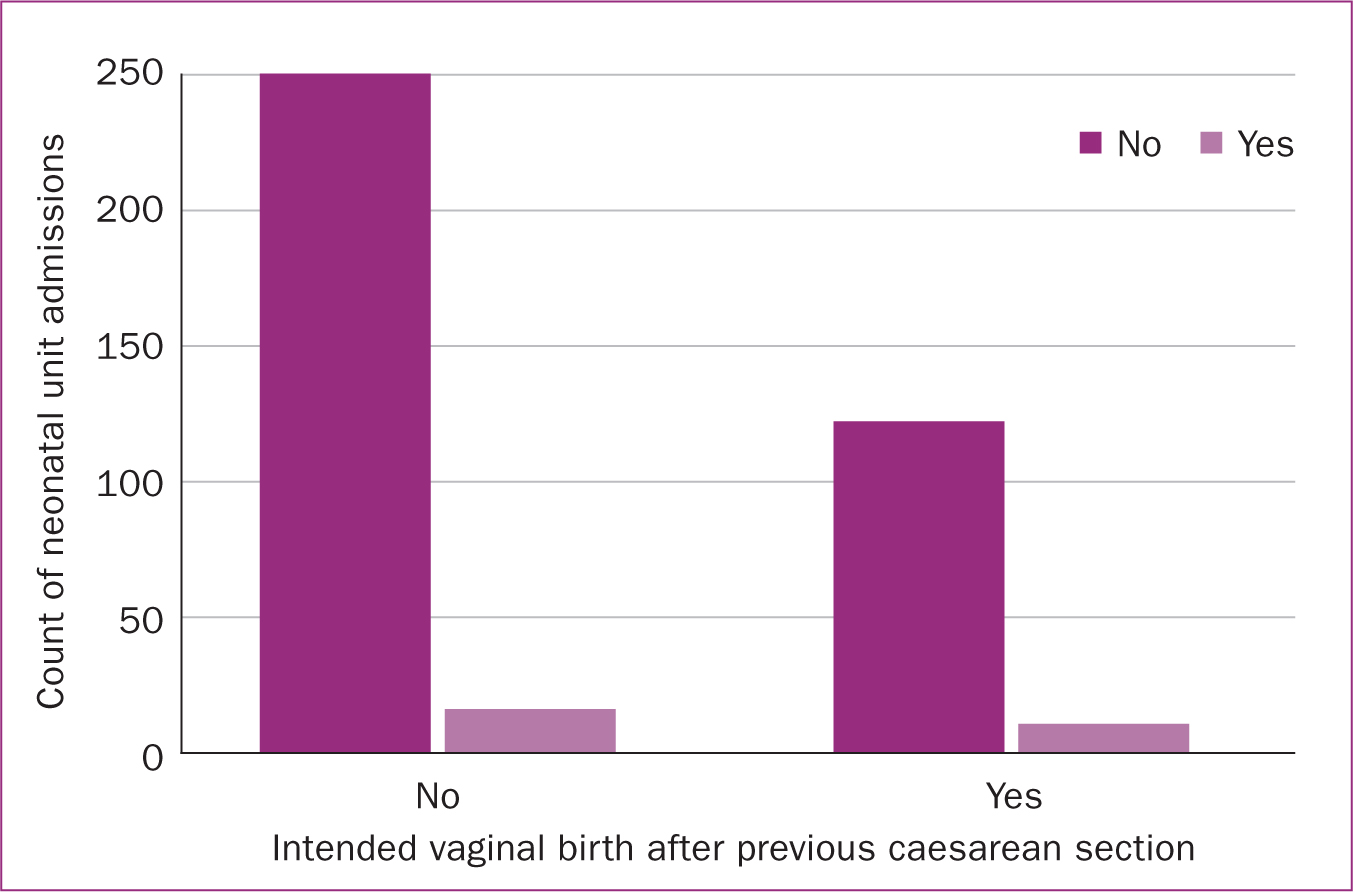
In the analysis for association between mode of birth, Apgar scores at 5 minutes and neonatal unit admissions, the full model showed that all predictors were statistically significant (P<0.001), as shown in Table 3. This indicates that there were significant differences between the two intended modes of birth in relation to neonatal outcomes based on Apgar at 5 minutes and neonatal unit admissions. The model explained between 3.4% (Cox and Snell R2) and 4.7% (Nagelkerke R2) of the variance in neonatal outcomes, and correctly classified 68.5% of cases. The analysis suggests that Apgar score was likely to be higher among those in the vaginal birth after caesarean group compared to the elective repeat caesarean group; however, admittance to the neonatal unit was not significantly different between the groups. Figures 1 and 2 show the distribution of Apgar scores and neonatal unit admissions between each group.
Table 3. Logistic regression output prediction of neonatal oucomes based on intended mode of birth
| B | Standard error | Wald | df | Odds ratio (95% confidence interval) | P value | |
|---|---|---|---|---|---|---|
| Apgar | 0.654 | 0.201 | 10.537 | 1 | 1.923 (1.296–2.854) | 0.001 |
| Neonatal unit admission | 0.698 | 0.434 | 2.586 | 1 | 2.010 (0.858–4.707) | 0.108 |
| Constant | -7.053 | 1.946 | 13.134 | 1 | 0.001 | <0.001 |
Neonatal unit admissions
Further descriptive analysis was carried out to explore factors related to neonatal unit admission. Only 27 (6.8%) neonates were admitted to the neonatal unit from this sample.
The majority of neonatal unit admissions had a primary and secondary reason for admission recorded. Respiratory distress syndrome was the most common reason followed by suspected sepsis. These results are summarised in Table 4. Despite having higher Apgar scores, the intended vaginal birth after caesarean group had a higher proportion of admissions to the neonatal unit (n=11, 8.7%) compared to the elective repeat caesarean group (n=16, 6.0%). Admissions for suspected sepsis as the primary reason were more common in the intended vaginal birth group (n=3, 2.3%) than the intended elective repeat caesarean group (n=1, 0.3%). Suspected sepsis as a secondary admission reason was more common in the elective repeat caesarean group.
Table 4. Reasons for neonatal unit admissions based on intended mode of birth
| Reason | Intended vaginal birth (n=11) | Intended elective caesarean (n=16) | ||
|---|---|---|---|---|
| Primary reason | Secondary reason | Primary reason | Secondary reason | |
| Respiratory distress syndrome | 5 (4.0) | 0 (0.0) | 14 (5.2) | 0 (0.0) |
| Suspected sepsis | 3 (2.3) | 5 (3.9) | 1 (0.3) | 11 (4.1) |
| Cardiac | 0 (0.0) | 0 (0.0) | 1 (0.3) | 0 (0.0) |
| Feeding concern | 0 (0.0) | 2 (1.5) | 0 (0.0) | 1 (0.3) |
| Other | 3 (2.3) | 1 (0.7) | 0 (0.0) | 2 (0.7) |
Admission for feeding concerns was never a primary reason for admission and was more common in the vaginal birth after caesarean group (n=2, 1.5% compared to n=1, 0.3%) as a secondary reason. The sole admission for cardiac-related reasons was an outlier and an isolated case, similar to the three suspected genetic disorders that were recorded as part of the ‘other’ category (full data for ‘other’ were not extracted).
Discussion
This study explored whether there was an increased risk of adverse neonatal outcomes for women/pregnant people who chose to have a vaginal birth after a previous caesarean section, compared with those who chose elective repeat caesarean section. The results suggest that those who opted for vaginal birth had higher Apgar scores, while admissions to the neonatal unit did not differ by intended mode of birth. Overall mean Apgar scores were similar between both groups; both intended vaginal birth and elective repeat caesarean had generally high Apgar scores. It may be the case that other factors are more salient in impacting Apgar scores and neonatal unit admissions.
The present study's findings are reflected in the broader literature; vaginal birth after a caesarean section is generally considered a safe option for neonates (Royal College of Obstetricians and Gynaecologists, 2015; NICE, 2023). The national maternity and perinatal audit for England 2019–2020 stated that 98.6% of term neonates scored an Apgar >7 at 5 minutes (HQIP, 2022). While this evidence does not probe further into the data regarding modes of birth, the results from the present study appear to be similar.
One notable difference between the groups, albeit slight (and not significant), was that the emergency caesarean section group had higher mean Apgar scores than the elective repeat caesarean section group. While this could be a chance finding resulting from the sample size, an explanation can be found in the broader literature; for elective repeat caesarean section, the neonate is exposed to contractions prior to birth, which can have a positive physiological effect in preparing the neonate for ex-utero adaptation (Boxwell et al, 2019).
The total number of neonates admitted to the neonatal unit was 27, equivalent to 6.8% of the sample. Reviewing outcomes and modes of birth indicated that neonatal unit admissions were highest in the emergency caesarean section group and lowest in the elective repeat caesarean section group. This is reflected in the literature (Young et al, 2018). However, the mean Apgar score for emergency caesarean sections was higher than elective repeat caesarean sections. The reasoning behind this is unclear and further research is recommended.
Respiratory distress syndrome was the primary admission reason for all neonates, regardless of intended mode of birth. Among the intended elective repeat caesarean group, there was a slightly higher number of respiratory distress syndrome cases (although this difference was not statistically significant). Respiratory distress syndrome in caesarean section cases is caused by surfactant deficiency combined with the neonate not being exposed to the usual hormone changes that occur in labour. As a result, neonates born by caesarean section are potentially at risk of respiratory distress syndrome (Edwards et al, 2013; Li et al, 2019) and therefore potentially increased neonatal unit admissions. However, the latest NICE (2023) review suggests that there is not enough evidence to confirm this risk.
Admission for suspected sepsis was the second most common primary reason for neonatal unit admission and the most common secondary reason for admission. Sepsis admissions were higher in the intended vaginal birth after caesarean group as a primary admission reason. Vaginal birth after caesarean risk factors for sepsis include prolonged rupture of membranes, Group B Streptococcus, multiple vaginal examinations or maternal suspected infection (Morgan et al, 2016). All these reasons could predispose the neonate to infection in the birth canal (Grassham et al, 2021). The present study did not explore the infection status of these neonates further, which should be noted and is recommended in future studies. In addition, thresholds for treating suspected infections can vary between trusts based on parameters and local guidance (Crocker et al, 2021).
The reasons for admission to the neonatal unit for all other conditions are also generally accounted for in the current literature. For example, feeding concerns (which was the secondary reason for 11.1% of admissions) were likely related to the primary reasons for admission: respiratory distress syndrome or sepsis (Crocker et al, 2021; Grassman et al, 2021).
In practical terms, the present study suggests that while there were differences, both vaginal birth and elective repeat caesarean were safe for women/pregnant people giving birth after a previous caesarean section. Both vaginal birth and elective repeat caesarean had similar rates of neonatal unit admissions. However, uptake of elective caesarean section may be higher at this NHS trust than the rate across England. The HQIP (2022) clinical report for 2022 reported that between 1 April 2018 and 31 March 2019, 38% of cases were eligible for vaginal birth after caesarean section, compared with only 32.1% at this NHS trust. While this is an incidental finding, this remains useful background information in the context of this study for women/pregnant people and trust practitioners. The findings from this study could be presented to at antenatal appointments to aid informed, collaborative decision making.
Limitations
There are a number of limitations to this study that are worth noting. First, demographics and potential confounding variables, such as comorbidities, age and ethnicity were not included in the analyses, meaning that it was not possible to account for their impact on neonatal outcomes. Care should be taken in generalising these findings and future studies should aim to include these variables. Furthermore, this study did not include any person who underwent induction of labour and did not investigate neonates who were ward attenders into neonatal unit, only those admitted (stays for longer than 4 hours). These groups should be considered in any future analyses. Finally, while the sample included almost 400 people, there was a small number of births that resulted in particularly low Apgar scores and neonatal unit admissions. To fully investigate the factors that impacted Apgar scores and neonatal unit admissions for these groups, a much larger sample is needed.
Conclusions
The results suggest that both vaginal birth after a previous caesarean section and elective repeat caesarean section are safe options for neonates. The gold standard for healthcare professionals is to empower women/pregnant people and their families to support them in their decision making with evidence. This study contributes to this knowledge base. Gaps in present knowledge of local outcomes exist; from here, a suggested future initiative is to undertake a broader study with a larger cohort of participants, including compounding variables such as co-morbidities, age, ethnicity, to fully explore factors influencing neonatal outcomes in depth.
Key points
- The evidence related to neonatal outcomes after a caesarean section birth is limited.
- This study sought to examine neonatal outcomes among women/pregnant people after a previous caesarean section, comparing outcomes between those opting for vaginal birth and elective repeat caesarean.
- While the vaginal birth group had slightly higher Apgar scores, the difference was generally minimal. Neonatal admissions did not differ between the groups.
- The present study's results show that both modes of birth are safe.
- As practitioners, it is important to improve the information available, based on the best evidence that can be provided to counsel women/pregnant people in informed decision making.
CPD reflective questions
- In everyday practice, how could midwives enhance the informed decision-making process for vaginal birth after caesarean section versus elective repeat caesarean section?
- How could midwifery and obstetric healthcare professionals combine expertise to apply this in a multidisciplinary team approach with women/pregnant people and their families?
- How could the decision-making process to support women/pregnant people as part of a multidisciplinary team be improved?
- Does your maternity service share local outcomes? How can local outcomes be shared more readily with service users?


