
Midwives everywhere strive to provide the best care for women and their families, and make a significant contribution to reducing the stillbirth and maternal mortality rates. In England, the stillbirth rate for 2015 was 4.49 per 1000 total births, compared to 4.66 in 2014 (Office for National Statistics, 2016) (Figure 1). This represents a reduction of 3.6% in 2015 and, if this rate of reduction were to continue until 2020, we could expect a drop of around 20% in the stillbirth rate compared to 2014. The maternal mortality rate in the UK reduced from 14 deaths in 2003/05 to 9 deaths per 100 000 maternities in 2011/13 (Knight et al, 2015).
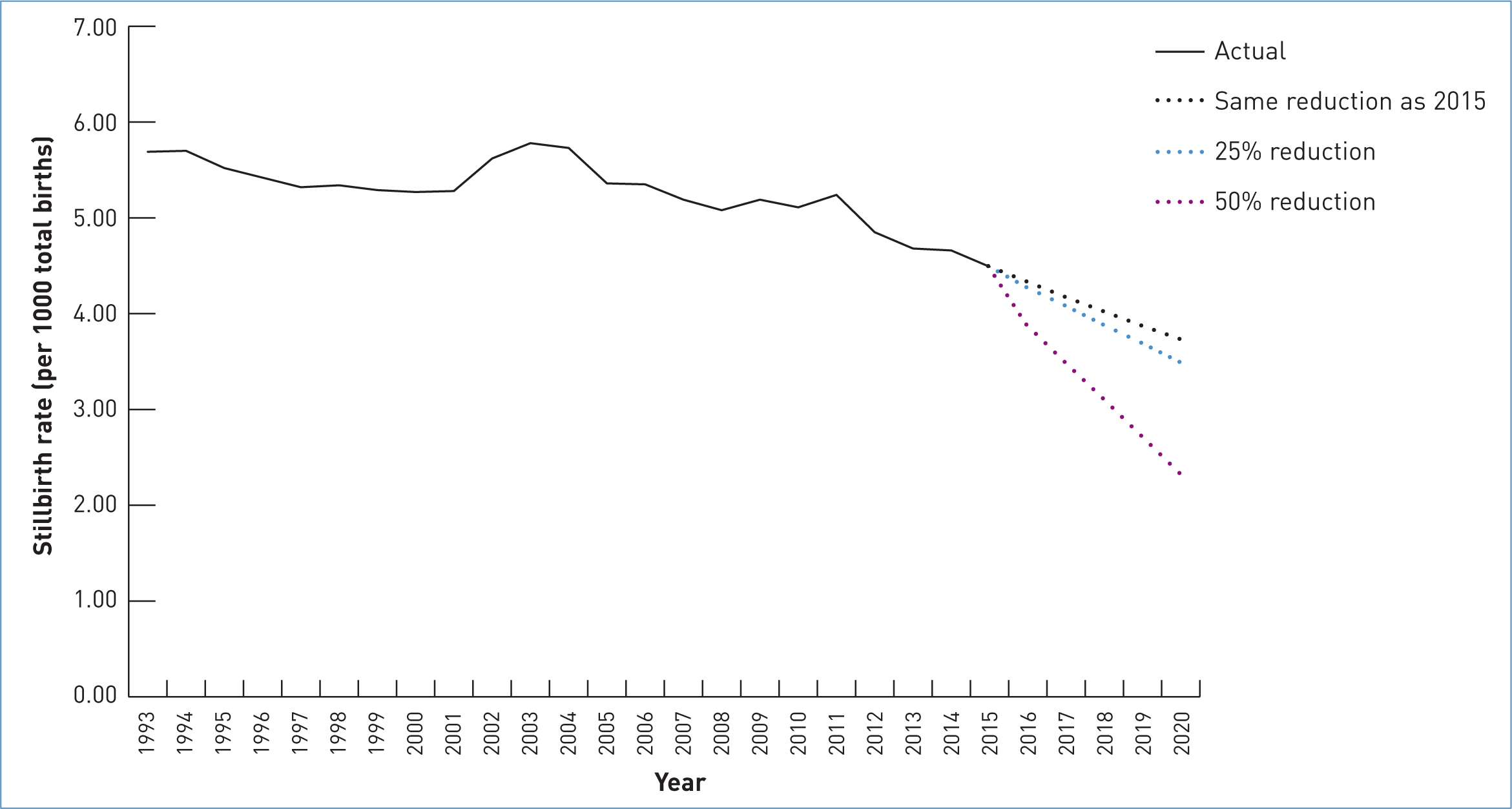 Figure 1. Stillbirth rates in England since 1993, including projections up to 2020.
Figure 1. Stillbirth rates in England since 1993, including projections up to 2020.
Room for improvement
When comparing maternity safety outcomes in the UK to other high-income countries, it is clear that improvements must be made. The Lancet (2016) stillbirth series shows that the UK was ranked 24/49 high-income countries for stillbirth rates, and the rate of progress in reducing stillbirth is slower than most of these countries, placing the UK 114/164 countries overall.
We also know that the unwarranted variation in stillbirth rates across England requires a dedicated focus to understand the actions required for improvement (Knight et al, 2015).
The newly launched Spotlight on Maternity, a policy document that contributes to the Government's national ambition to halve the rates of stillbirths, neonatal and maternal deaths and intrapartum brain injuries by 2030 (Department of Health (DH), 2016), outlines plans for maternity providers to ‘Sign Up to Safety’. This initiative sets out five high-level themes which are known to make care safer (Berwick, 2013). These are:
- Building strong leadership in maternity services by: ensuring a board-level focus on safety in maternity; setting up your maternity team to ensure a focus on safety; developing a bespoke Safety Improvement Plan for maternity
- Building capability and skills for all maternity staff by: improving communication within and across teams; ensuring that all maternity staff complete and implement multi-disciplinary training
- Sharing progress and lessons learnt across the system by: sharing your Safety Improvement Plan and progress publicly; sharing what you are learning so that others can benefit; helping to create a national picture by contributing to the Government's annual report
- Improving data capture and knowledge in maternity services by: improving the collection and reporting of high-quality data to national data collections; ensuring that your service follows national guidelines for patient safety reporting
- Focusing on early detection of the risks associated with perinatal mental illness by: ensuring that all staff working in maternity services are trained to identify the risks and symptoms of mild to severe perinatal mental illness; ensuring that all staff working in maternity services are aware of the local perinatal mental health pathways of care (DH, 2016).
‘Initiative fatigue is fuelled by the launch of a plethora of maternity safety initiatives, which all aim to improve outcomes… but place a burden of responsibility on frontline staff for implementation’
The fundamental aim of the Sign up to Safety initiative is that safety becomes an intrinsic part of everyone's job, all of the time, in all parts of the system. It is a policy that outlines implementation support including, for example, safety webinars and a range of helpful resources. While this approach to improving safety is proving to be an invaluable resource for some, initiative fatigue is felt by others. The latter is fuelled by the launch of a plethora of maternity safety initiatives—including the Royal College of Obstetricians and Gynaecologists national quality improvement programme, Each Baby Counts; NHS England's Saving Babies' Lives Care Bundle; and the recommendations outlined in Better Births, the report of the National Maternity Review. These initiatives all aim to improve outcomes for women and babies, but place a burden of responsibility on frontline staff for implementation.
System leaders should support midwives and obstetric colleagues to recognise the benefits of safety campaigns that will be implemented by their organisation, and develop an implementation infrastructure that does not increase the burden on frontline staff.
Successful implementation of health policy includes a requirement for:
- Adequate time and sufficient resources
- Levers and/or incentives that are demonstrable
- Clarity and explanation to staff regarding how policy translates into practice
- Involvement of user groups and Maternity Services Liaison Committees
- Implementation barriers must be recognised and removed
- Co-design and local modification may be necessary
- Coordination and collaboration between those responsible for implementation
- System-wide stakeholders and collaborators; meaningful progress does not happen in isolation
- Sustainability plans that inform the provider's strategic operational and business planning.
Together, we can make a difference. With collaboration and the right implementation, safety will truly be an intrinsic part of everyone's job, all of the time, in all parts of the system.

