Postpartum haemorrhage is a major cause of maternal morbidity and mortality worldwide (Knight and Paterson-Brown, 2017). It accounts for one-quarter of all maternal deaths and 100 000 deaths every year, with one woman dying every 4 minutes as a result of postpartum haemorrhage alone (Sentilhes et al, 2015a; Sebghati and Chandraharan, 2017; Shakur et al, 2017). The picture is particularly bleak in low-resource regions such as sub-Saharan Africa, where the absence of skilled birth attendants at births, under-use or lack of uterotonics, and delayed access to emergency obstetric provision makes postpartum haemorrhage a major problem (Mpemba et al, 2014; Sheldon et al, 2014). The mortality rate due to postpartum haemorrhage has dramatically fallen in the UK, such that it is now relatively rare, with a mortality rate of 0.4 per 100 000 maternities, but in sub-Saharan Africa the rate is closer to 150 per 100 000 maternities (Weeks, 2014). As well as the extremely worrying maternal death rate, postpartum haemorrhage can result in severe maternal morbidity, including anaemia, the need for multiple blood transfusions, organ failure, and hysterectomy (Sheldon et al, 2014; Sebghati and Chandraharan, 2017); and the incidence of postpartum haemorrhage is increasing worldwide (Weeks, 2014; Nyfløt et al, 2017), despite the established use of preventative interventions such as active management of the third stage of labour (Say et al, 2014). In fact, this increase may be due, in part at least, to the increasing use of intervention during labour and birth (Weeks, 2014).
The definition of postpartum haemorrhage according to the Royal College of Obstetricians and Gynaecologists (RCOG) (2016) and the World Health Organization (WHO) (2012) is a blood loss of 500 ml or more within 24 hours of birth: with 500-1000 ml representing a minor postpartum haemorrhage, and a blood loss of more than 1000 ml being classified as a major postpartum haemorrhage. The definition—particularly regarding the amount of blood loss that constitutes a postpartum haemorrhage—varies between studies and national guidelines (Dahlke et al, 2015), but additional clinical signs and symptoms of hypovolaemia (including tachycardia, tachypnoea, and altered mental state) are usually considered in the assessment. This is particularly important as bleeding can be concealed and because a given blood loss can have very different outcomes, depending on the pre-existing health status of the woman involved (Begley et al, 2015; Knight and Paterson-Brown, 2017). The most common cause of postpartum haemorrhage is uterine atony, where the uterine contractions that normally clamp down on uterine blood vessels to stem blood flow to the placental bed are insufficient, and postpartum bleeding continues or worsens (Weeks, 2014; Dahlke et al, 2017; Sebghati and Chandraharan, 2017). The incidence of postpartum haemorrhage due to uterine atony is increasing (Dahlke et al, 2015). However, an increasingly common cause for concern is abnormally adherent placentation, which is now a leading cause of postpartum haemorrhage and the need for peripartum hysterectomy, as well as an increasingly significant cause of maternal death associated with postpartum haemorrhage (Goh and Zalud, 2016; Knight and Paterson-Brown, 2017). This article will discuss the aetiology and risk factors for postpartum haemorrhage and abnormally adherent placentation, as well as the interventions used as prevention and those that can be associated with these severely adverse outcomes.
Postpartum haemorrhage: aetiology and risk factors
The most common causes for postpartum haemorrhage are uterine atony, abnormal adherent placentation, retained placental tissue, tears and clotting problems (Weeks, 2014; Sentilhes et al, 2015b). These and other causes and risk factors can be categorised as one of the ‘4Ts’: tone, tissue, trauma and thrombin (Table 1). Nyfløt et al (2017) found the most common aetiologies for severe postpartum haemorrhage to be uterine atony (60% of cases) and placental complications (36% of cases). Risk factors for the occurrence of postpartum haemorrhage have been identified (Table 1) and can be categorised according to whether they occur in the antepartum or intrapartum period (Table 2). These include a history of postpartum haemorrhage, anaemia, abnormally adherent placentation, induction and augmentation of labour, caesarean birth, and a prolonged third stage of labour (Weeks, 2014; Sentilhes et al, 2015b; Nyfløt et al, 2017; Sebghati and Chandraharan, 2017).
| Tone: insufficient uterine contractility allows blood flow to the placental bed to continue and prevents proper control of bleeding |
|
| Tissue: retained placental tissue prevents the uterus from contracting down |
|
| Trauma: tears in the cervix, vagina or perineum can cause large blood losses, especially if they go unnoticed |
|
| Thrombin: coagulation abnormalities which may be congenital or acquired |
|
| Antepartum risk factors |
|
| Intrapartum risk factors |
|
Nyfløt et al (2017) found the strongest risk factor for postpartum haemorrhage to be a history of previous postpartum haemorrhage. The reasons for this increased risk of reoccurrence are unclear, but may involve factors such as undiagnosed coagulation disorders, underlying genetic predisposition, or a predisposition to receptor desensitisation or other forms of myometrial fatigue (Oberg et al, 2014). However, most women who have a postpartum haemorrhage have no identifiable risk factors, and it is therefore advised that postpartum haemorrhage should be anticipated at every birth in order for prepared management of this complication (Sebghati and Chandraharan, 2017). In fact, Sentilhes et al (2015a) suggest that, because of the high rate and unpredictability of postpartum haemorrhage, it should be prophylactically prevented in all women. However, a glance at the list of risk factors for postpartum haemorrhage (Tables 1 and 2) illustrates how maternity care can affect the risk of postpartum haemorrhage. This risk could therefore be reduced with the judicious use of obstetric interventions, including induction, augmentation, episiotomy, instrumental and caesarean birth, which are limited to situations where evidence supports their use (Hofmeyr and Qureshi, 2016; Nyfløt et al, 2017).
Abnormally adherent placenta
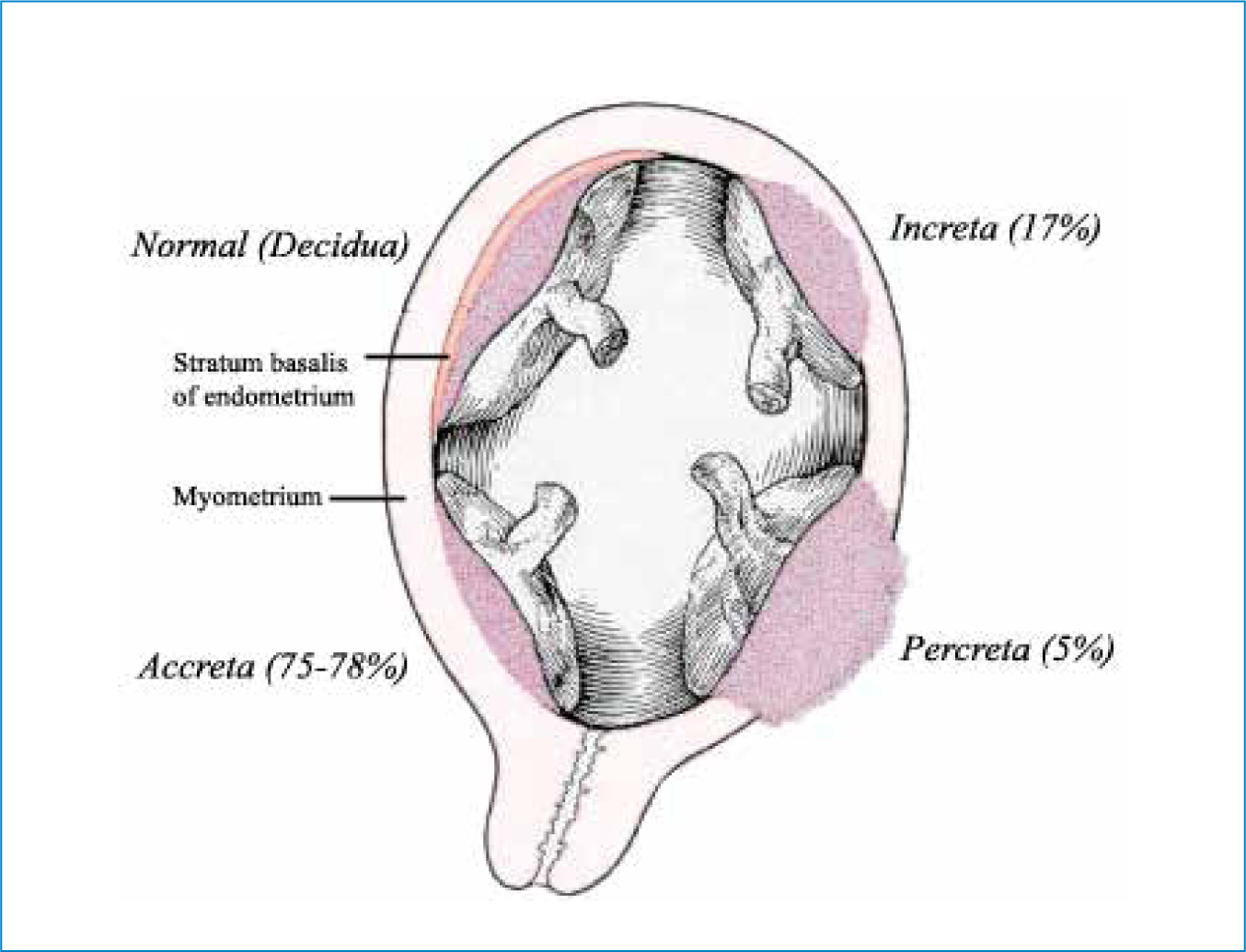
Invasive or adherent placentation is thought to result from a lack of, or insufficient decidua in the area of implantation (Goh and Zalud, 2016; Belfort et al, 2017) and is classified by one of three grades (accreta, increta, and percreta), based on how far into the uterine wall placental villi penetrate (Figure 1). Placenta accreta is the least severe form, where placental villi have penetrated the surface of the myometrium; placenta increta is where villi have invaded into the myometrium; and placenta percreta is the most severe form, where placental villi invade through the myometrium and penetrate the uterine serosa, and potentially adjacent organs such as the bladder or bowel. (Goh and Zalud, 2016; Baldwin et al, 2017; Farquhar et al, 2017). Associated complications are largely a result of huge blood loss and include death, hysterectomy and multiple blood transfusions (which are also associated with complications, including consumptive coagulopathy and transfusion reactions) (Goh and Zalud, 2016; Belfort et al, 2017; Farquhar et al, 2017). Risks to infant health are largely related to preterm birth and include low birthweight and admission to neonatal intensive care (Belfort et al, 2017; Farquhar et al, 2017).
The importance of abnormally adherent or invasive placentation as an increasingly significant cause of morbidity and mortality related to postpartum haemorrhage is reflected by its specific discussion in national guidelines (Dahlke et al, 2015; RCOG, 2016) as well as the recent MBRRACE report (Knight and Paterson-Brown, 2017), which found that, of the 22 women who died from obstetric haemorrhage, 8 of the deaths (36%) were associated with abnormally adherent placentation. The authors also noted that more women than ever before were dying from this cause (Knight and Paterson-Brown, 2017). The incidence of abnormally adherent placentation is also increasing globally, such that it now represents a leading cause of perinatal morbidity (Goh and Zalud, 2016), and this is widely thought to reflect the worldwide rising caesarean rates (Baldwin et al, 2017; Belfort et al, 2017; Knight and Paterson-Brown, 2017). As caesarean section rates continue to rise, abnormally adherent placentation is likely to become an increasingly prevalent complication (Goh and Zalud, 2016). However, outcomes can be improved by accurate antenatal diagnosis, as this allows for comprehensive multidisciplinary intrapartum planning and management, as well as avoidance of potentially futile attempts to remove an undiagnosed abnormally adherent placenta (Fitzpatrick et al, 2014; Goh and Zalud, 2016; Belfort et al, 2017; Farquhar et al, 2017). As caesarean section increases the risk of adherent placentation occurring in future pregnancies, lowering the rates of unnecessary caesarean sections represents an important intervention to reduce the incidence of this severely adverse pregnancy complication (Hofmeyr and Qureshi, 2016).
Induction, augmentation, and active management of the third stage
Use of oxytocin
Synthetic oxytocin (Syntocinon) is commonly used in labour and birth, either intravenously to induce or augment labour, or intramuscularly during the third stage as a prophylactic intervention to prevent postpartum haemorrhage (Gu et al, 2016; Khajehei, 2017). However, there are wide variations between guidelines and in practice, and decisions on oxytocin dosage and use are often subjective (Gu et al, 2016; Page et al, 2017).
In addition, while these interventions are often effective, the intrapartum use of oxytocin is not without its risks. In the short-term, the longer, stronger, more frequent contractions increase the resting tone of the uterus and can reduce blood flow to the fetus, resulting in fetal distress, uterine hyperstimulation and tachysystole (Gu et al, 2016; Page et al, 2017). The use of intrapartum oxytocin also increases the risk of uterine atony and thus postpartum haemorrhage (Erickson et al, 2017; Page et al, 2017). Syntocinon is structurally identical to endogenous oxytocin, and this adverse effect on uterine function is thought to be due to receptor desensitisation—where prolonged exposure to synthetic oxytocin results in oxytocin receptors no longer responding to endogenous or exogenous oxytocin—causing reduced contractility and an atonic uterus (Balki et al, 2013). This effect is thought to occur in a dose- and time-dependant manner, such that the longer the exposure to and the higher the dose of oxytocin, the greater the risk (Balki et al, 2016). Therefore, the minimal effective dose, for the shortest duration necessary is recommended (Page et al, 2017; Rousseau and Burguet, 2017). In the long-term, the effects of prolonged intrapartum exposure to synthetic oxytocin warrant consideration, as this has been linked to a range of adverse outcomes including postnatal depression and anxiety for the mother, poor cognitive development and bipolar disorder for the child, and reduced breastfeeding (Bell et al, 2014; Freedman et al, 2015; Gu et al, 2016; Burguet and Rousseau 2017; Erickson et al, 2017; Khajehei, 2017).
Active management of third stage
The third stage of labour is recognised as a key point during which to prevent postpartum haemorrhage, as the degree of blood loss may depend on how quickly the placenta separates from the uterine wall and is expelled through the birth canal (Westoff et al, 2013; Sentilhes et al, 2015a). Thus, active management of the third stage aims to reduce this time-period through a package of interventions which include the prophylactic administration of synthetic oxytocin, early clamping and cutting of the cord, controlled cord traction to remove the placenta, and uterine massage in some cases (Hofmeyr et al, 2015; Sentilhes et al, 2015a). While the efficacy of prophylactic oxytocin in reducing postpartum bleeding has been demonstrated (Westoff et al, 2013) and is recommended by the WHO (2012) and RCOG (2016), the other components of active management may provide little if any benefit (Sentilhes et al, 2015b; Hofmeyr and Qureshi, 2016). The efficacy of controlled cord traction and uterine massage have both been questioned (Deneux-Tharaux et al, 2013; Hofmeyr et al, 2013; Hofmeyr et al, 2015) and neither have demonstrated any significant benefit; while early cord clamping is likely to be potentially harmful for many reasons, including reducing the volume of blood transfused to the neonate, and affecting neurodevelopment as a result of iron deficiency (Ceriana Cernadas, 2017).
The oxytocin debate
While its efficacy is not in doubt, the need for prophylactic oxytocin to prevent postpartum haemorrhage in all women has been questioned. Erickson et al (2017) found that, among women who underwent labour without the use of oxytocin for induction or augmentation, while prophylactic oxytocin reduced what the authors called ‘normal postpartum blood loss’, it did not reduce the risk of having a ‘clinically significant’ postpartum haemorrhage. The authors suggested that when intrapartum oxytocin was not used, the same risks of uterine atony were not present (Erickson et al, 2017), as the uterus was unhindered in carrying out its function. The authors also questioned 500 ml as a cut-off for the diagnosis of postpartum haemorrhage, as for many healthy women, this may represent a physiologically normal blood loss, which has been accounted for by the increased blood volume during pregnancy. They also suggest that the widespread use of prophylactic oxytocin may have resulted in a misguided view of normal postpartum blood loss, and that research based on 500 ml as a cut-off for diagnosing postpartum haemorrhage may therefore be distorted by including women who have experienced a normal blood loss following birth (Erickson et al, 2017). However, the effect of blood loss on the individual woman needs to be considered, as factors such as a low BMI and pre-existing anaemia will compromise a mother's ability to withstand blood loss (Begley et al, 2015; Sebghati and Chandraharan, 2017). Thus, in low-resource countries, where many women have anaemia and are malnourished, postpartum blood loss has a significant effect, and postpartum haemorrhage is much more likely to result in severe morbidity and mortality (Begley et al, 2015).
As well as reducing tolerance to blood loss, anaemia is itself a risk factor for postpartum haemorrhage (Weeks, 2014; Frass 2015; Nair et al, 2016), and therefore represents an important target for intervention. This increased risk of postpartum haemorrhage may be due to reduced oxygen supply to the myometrium as a result of anaemia (Frass, 2015), which would reduce its ability to contract in the short-term, and may have an additional long-term effect on myometrial function if oxygen supply has been chronically compromised. In low-income countries, interventions to target to pre-existing conditions such as anaemia (such as de-worming, increasing iron intake, and delayed cord clamping) may be particularly important in reducing the incidence, morbidity, and mortality associated with postpartum haemorrhage (Weeks, 2014; Tort et al, 2015; Ceriana Cernadas, 2017).
Tranexamic acid
As the placenta shears off the uterine wall during the third stage of labour, strong myometrial contractions clamp down on uterine blood vessels, stemming the flow of blood to the placental bed. Simultaneously, the clotting system is activated resulting in the formation of a fibrin clot that seals off wounds, preventing bleeding. However, clot formation is a dynamic process and the clot is broken down and moulded in order to prevent occlusion of blood vessels (McCormack, 2012; Sentilhes et al, 2015a) (Figure 2). While oxytocin is used to enhance the ‘mechanical’ effect of uterine contractions in reducing bleeding following birth, the complimentary use of a haemostatic agent such as tranexamic acid to prevent or stop postpartum haemorrhage has also been suggested (Sentilhes et al, 2015b) (Figures 2 and 3). Tranexamic acid acts on the coagulation process to prevent the breakdown of the fibrin clot, and although it has long been used to prevent haemorrhage associated with caesarean delivery, its use is now being suggested for postpartum haemorrhage following vaginal birth, along with the usual prophylactic uterotonic (Novikova et al, 2015; Sadek et al, 2018; Sentilhes et al, 2018). However, caution has been advised to due to concerns around the quality of some of the evidence supporting its use, as well as the potential for thromboembolism (Sentilhes et al, 2015a; Ker et al, 2016). These doubts however, may be abrogated by the recent results of the WOrld Maternal ANtifibrinolytic (WOMAN) trial (Shakur et al, 2017; Weeks, 2018).
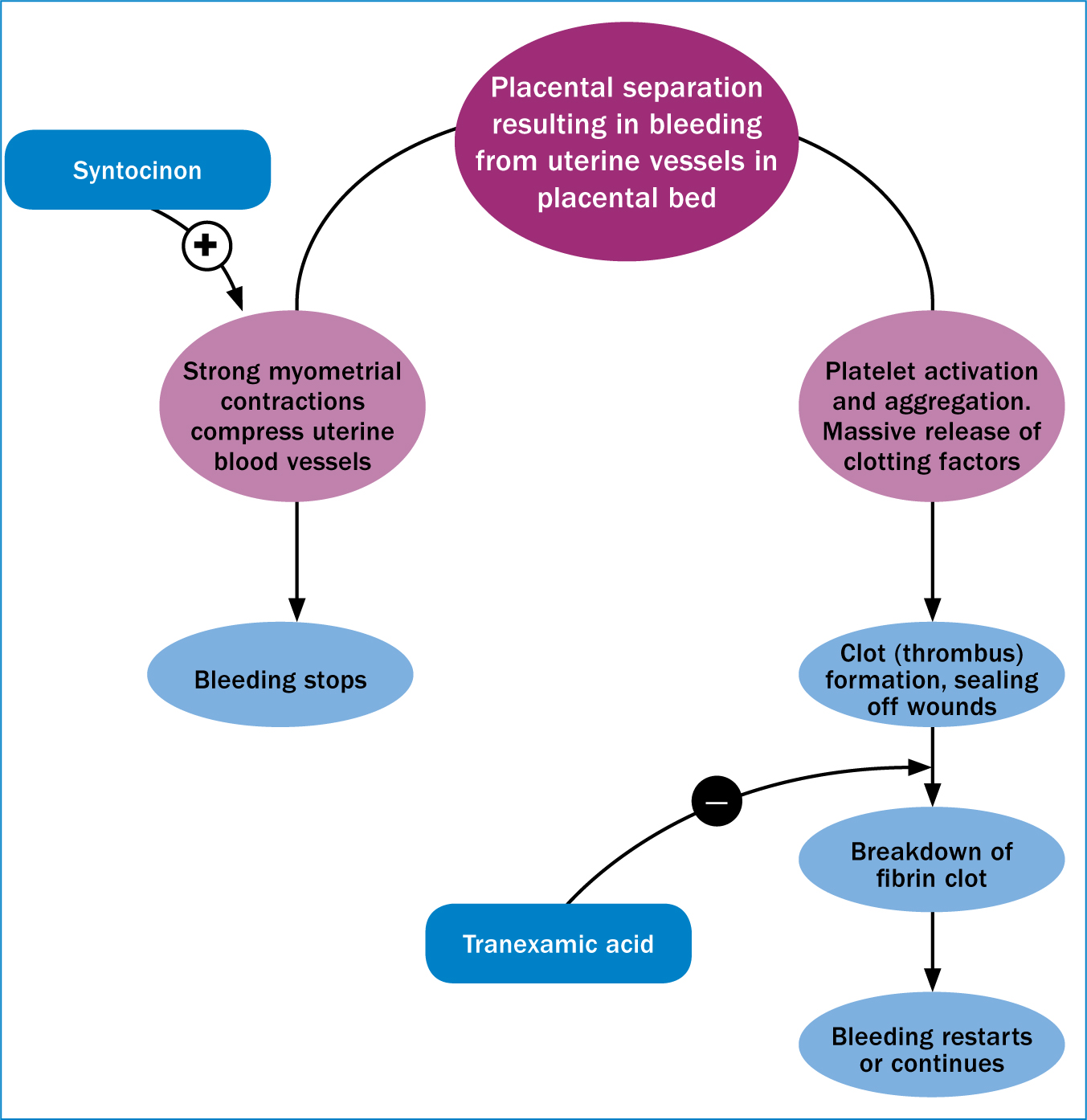
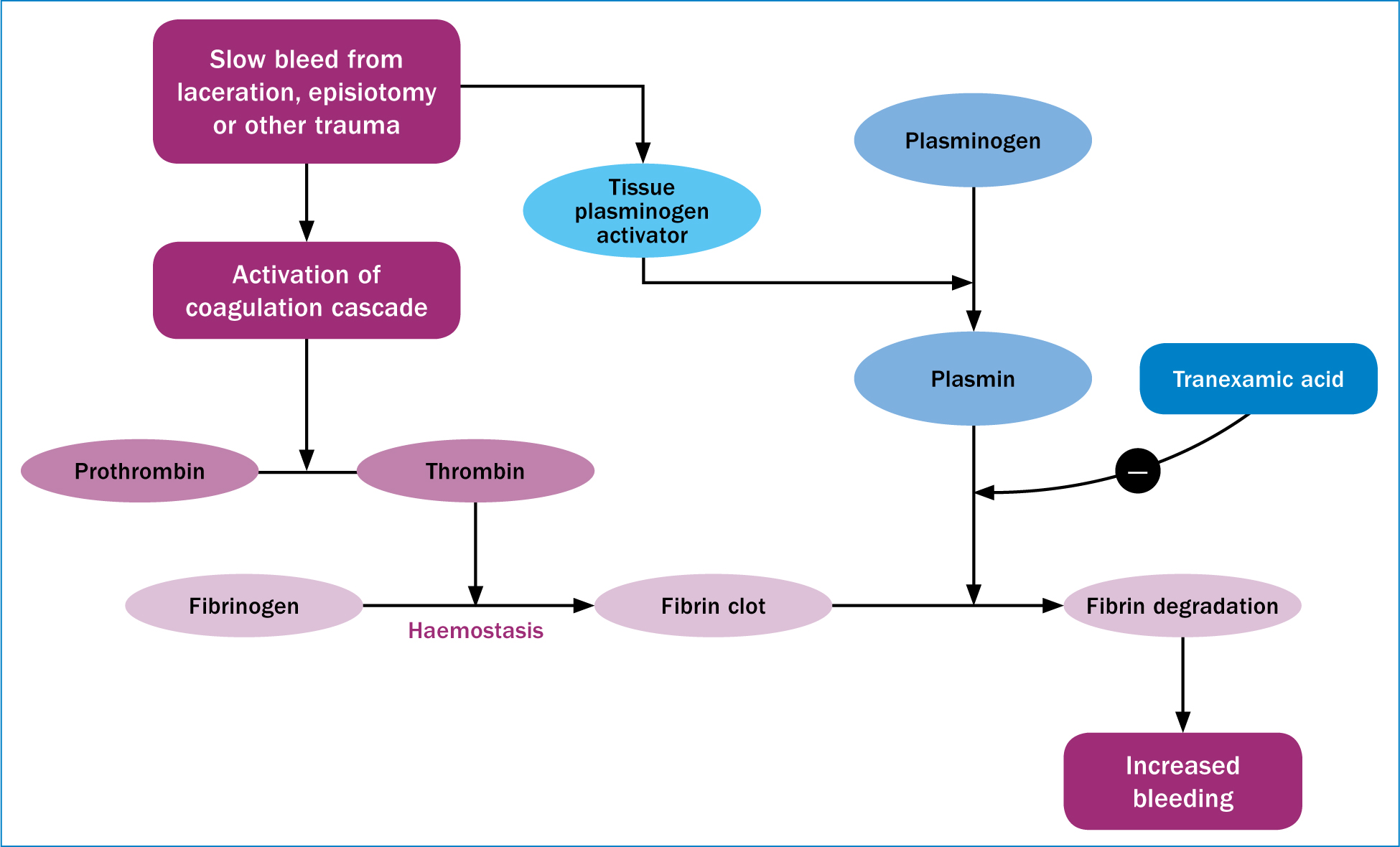
The WOMAN trial (Shakur et al, 2017) was a large, multi-country study, involving more than 20 000 women who were diagnosed as having a postpartum haemorrhage following vaginal or caesarean birth, and aimed to determine whether the early intravenous administration of tranexamic acid improved outcomes associated with postpartum haemorrhage. Administration of tranexamic acid was found to significantly reduce deaths due to postpartum haemorrhage (Shakur et al, 2017) and WHO guidelines have been updated accordingly (Vogel et al, 2018). Importantly, it has been found to be cost-effective in countries where there is a high risk of death due to postpartum haemorrhage (Weeks, 2018). Due to its mechanism of action that results in stabilisation of blood clots, tranexamic acid may be particularly effective in preventing the slow, but potentially life-threatening bleeds that can result from tears or trauma to the birth canal (Figure 3), and which often go unnoticed (Weeks, 2018). It may, however, be less effective in preventing normal postnatal blood loss or heavy loss from large open vessels, which relies primarily on strong uterine contractions to stem blood flow (Weeks, 2018).
Conclusion
Tranexamic acid represents an extremely promising intervention to prevent deaths due to postpartum haemorrhage. Primary intervention also needs to be tackled, to restrict intervention to situations where it is required and where its use is evidence-based. Caesarean section is a prime candidate for this, with its rising rates, because it is in itself a risk for postpartum haemorrhage, and because it poses a risk to future pregnancies of abnormally adherent placentation, uterine rupture, and the huge postpartum blood losses that can be associated with these. In addition, the widespread use of intrapartum oxytocin should perhaps be reconsidered, given the diverse short- and long-term adverse outcomes potentially associated with its use. Finally, the definitions of physiological postpartum blood loss may need to be reconsidered, so that research and guidelines for prevention and treatment are aimed at pathological and not physiological blood loss.

