Postpartum haemorrhage is defined as blood loss of over 500ml from the genital tract in the first 24 hours of a baby's birth (Mavrides et al, 2016). It is a current global health concern, as it is a major cause of maternal mortality in low- and middle-income countries (World Health Organization (WHO), 2022). The sustainable development goals seek to decrease the global maternal mortality rate to under 70 per 100 000 live births by 2030, yet in 2017, the maternal mortality rates in low-income countries were 434.7 per 100000 (Sachs et al, 2021). The WHO (2022) states that, each year, postpartum haemorrhage occurs in 14 million women, leading to an estimated 70 000 maternal mortalities globally. Women in low- and middle-income countries are disproportionately affected by postpartum haemorrhage and the associated risk of morbidity and mortality, as it is estimated that 80% of maternal deaths from postpartum haemorrhage occur in sub-Saharan Africa and south Asia (WHO, 2023).
The WHO (2018) recommends oxytocin as the preferred prophylactic uterotonic for prevention of postpartum haemorrhage, to be administered as part of active management during third-stage labour. However, oxytocin has been found to be heat-sensitive, and a cold chain system is required of between 2–8°C. When oxytocin is not maintained in a cold chain, there is a risk of degradation and resulting ineffective prevention of postpartum haemorrhage (Nguyen et al, 2019). Consequently, this has implications for low- and middle-income countries, as they are frequently tropical climate countries and cold storage and distribution is not necessarily available in low-resource settings.
Carbetocin is a heat-stable, longer-acting uterotonic, currently licensed in the UK for the prevention of postpartum haemorrhage after caesarean section (Joint Formulary Committee, 2022). There are economic implications of using carbetocin as a substitute for oxytocin, as the supply cost is estimated at 20 times higher WHO (2018), on the agreement that if found to be non-inferior to oxytocin, then carbetocin could be provided in public sectors in low- and middle-income countries at an economical cost.
Methods
This review was carried out to determine if the use of carbetocin in low- and middle-income countries would reduce the risk of postpartum haemorrhage, and associated morbidity and mortality, in comparison to the use of oxytocin. The aim was to identify, critically evaluate, synthesise and interpret evidence from quantitative studies through a literature review.
The population, intervention, comparison and outcomes approach was applied to form a research question. This strategy enables a researcher to form a well-written and clearly formatted clinical question, and forms the key search terms for a literature review (Bermudez, 2021). A gap in current research was identified, as there was limited research comparing the use of carbetocin to oxytocin in low- and middle-income countries where the prevalence of postpartum haemorrhage is high and contributes to the increased maternity mortality ratio.
This review identified literature to address current research in this field, and the global priorities set out by the sustainable development goals. The research question was ‘does the use of carbetocin result in reduced blood loss in women during the third stage of labour, compared to oxytocin, in low- and middle-income countries?’.
Search strategy
The electronic databases searched were EBSCO, CINAHL, Medline and Global Health. The search terms are shown in Table 1. Although the population identified for this study was women in the third stage of labour in low- and middle-income countries, the terms ‘pregnancy’ and ‘women’ were not required, as the terms used for outcome would only incorporate this population. Search terms included synonyms, alternative spellings and abbreviations. The Boolean operators were used with ‘OR’ to connect terms in each component of the population, intervention, comparison and outcomes model, while ‘AND’ was used to connect search terms together in a single search string. Only studies written in English and produced within the last 10 years were included, as Rees (2011) emphasised that older research studies can be outdated and not always applicable to the present context.
Table 1. Search terms structured by population, intervention, comparison, outcome criteria
| Criteria | Search term |
|---|---|
| Population |
|
| Intervention |
|
| Comparison |
|
| Outcome |
|
Following the initial search, the terms ‘LMIC’, ‘low-income countries’, ‘middle-income countries’ or ‘developing countries’ were removed from the search, as limited research was found, further emphasising the gap in current research. The search terms in Table 1 were entered into the databases simultaneously, excluding the population terms.
Study selection
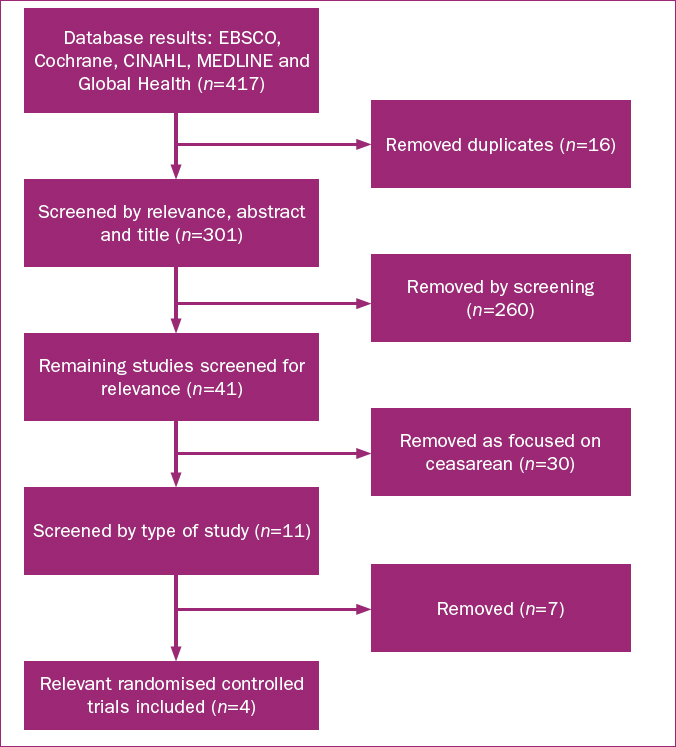
The search initially retrieved a total of 417 studies. During the selection process, duplicates were removed, and the titles and abstracts were screened for relevance to the author's question, and eliminated if irrelevant. This also included studies that focused on cost-effectiveness rather than clinical outcome. Studies that focused on caesarean section were removed, as the author believed that this clinical environment would have access to a cold chain system, and only studies involving vaginal birth were included. The study selection process is outlined in Figure 1.
Thematic analysis was applied using the Braun and Clarke (2006) size-phase process, which involves familiarising with data, generating initial codes, searching for themes, reviewing themes, defining and naming themes and producing the report.
Results and discussion
Four randomised controlled trials were selected for the study, and compared the use of carbetocin instead of oxytocin following vaginal birth for prevention of postpartum haemorrhage. Three of the four selected studies were associated with low- and middle-income countries. Details of the studies’ key findings, type of study, location, number of participants, aim, uterotonic dose and method of administration are shown in Table 2. Two were carried out a particular low- or middle-income country and one was carried out across 10 countries that included low- and middle-income countries; the location of the studies was key in answering the author's question.
Table 2. Summary of main findings from literature
| Authors | Type of study | Setting and participants | Aim, uterotonic dose and route | Main findings |
|---|---|---|---|---|
| Maged et al (2015) | Double-blind randomised study | Two hospitals in Egypt, n=100 participants | Aim: explore use of carbetocin vs oxytocin after vaginal birth for management of atonic postpartum haemorrhage. Dose: 100mcg carbetocin, 5IU oxytocin Route: intravenous | In women with vaginal birth, carbetocin associated with reduced blood loss and need for further uterotonics. No difference between two variables and number of majo poatpartum haemorrhages. |
| Amornpetchakul et al (2018) | Triple-blind randomised controlled trial | Thailand, n=350 participants | Aim: explore use of intravenous carbetocin vs oxytocin in prevention of atonic postpartum haemorrhage after vaginal birth in women at increased risk in singleton pregnancies.Dose: 100mcg carbetocin, 5IU oxytocinRoute: intravenous infusion | IV carbetocin more efficient compared to IV oxytocin in preventing postpartum haemorrhage. |
| Widner et al (2018) | Double-blinded randomized controlled trial | 23 hospitals across Argentina, Egypt, India, Kenya, Nigeria, Singapore, South Africa, Thailand, Uganda, and UK, n=29645 participants | Aim: non-inferiority trial comparing carbetocin vs oxytocin for prevention of postpartum haemorrhage after vaginal birth.Dose: 100mcg carbetocin, 10IU oxytocinRoute: intramuscular injection | Carbetocin non-inferior to oxytocin in preventing postpartum haemorrhage over 500ml or need for additional uterotonics.Not non-inferior for blood loss of over 1000ml in vaginal birth. |
| Hua et al (2020) | Double-blind randomised controlled trial | China, n=624 participants | Aim: research use of intravenous carbetocin vs oxytocin after vaginal birth in women at risk of postpartum haemorrhage (one risk factor).Dose: 100mcg carbetocin, 10IU oxytocinRoute: intravenous infusion | IV carbetocin no better than IV oxytocin in reducing blood loss over 500ml during vaginal birth. |
Study methods
The four studies identified were randomised controlled trials and an ABCDFIX mnemonic tool was used to individually critique each study. Randomised controlled trials have been identified as the second highest level of research, after systematic reviews, in the hierarchy of evidence, as the design is unbiased and leads to reduced systematic errors (Burns et al, 2011). Allocation of participants for all four selected studies was computerised; however, it was not stated if this was from an off-site location.
All four studies included blinding, with double-blinding of both patient and providers used in three of the studies (Maged et al, 2015; Widner et al, 2018; Hua et al, 2020). Amornpetchakul et al (2018) used triple-blinding, as the patient, providers and statisticians analysing the results were blinded. However, Penić et al (2020) explored the definitions of blinding in randomised controlled trials, and found that studies involving triple- or quadruple-blinding in masking registration were associated with the most discrepancies.
Maged et al (2015) and Amornpetchakul et al (2018) did not mention any follow up, and Widner et al (2018) reported that participation in the study concluded at discharge, transfer or death of participant. Hua et al (2020) reported that participants were followed up for 42 days. All studies ensured that groups were comparable to reduce the risk of bias and, consequently, any differences in outcomes between the two groups could be attributed to the intervention used.
Widner et al (2018) reported that four participants withdrew consent and outcomes were missing, equivalent to 0.2% participants in both the oxytocin and carbetocin group. All four studies clearly outlined the number of participants that were withdrawn for clinical reasons including emergency caesarean section, thrombocytopenia, non-atonic postpartum haemorrhage (Amornpetchakul et al, 2018) or treatment given after 3 minutes (Widner et al, 2018).
All studies focused on the outcome of preventing or managing postpartum haemorrhage. Key themes identified in the review included blood loss, postpartum haemorrhage over 500ml, postpartum haemorrhage over 1000ml, need for blood transfusion, retained placenta, haemoglobin levels and need for additional uterotonics. All studies provided details of how blood loss was collected and measured, except for Maged et al (2015); therefore, there may be a discrepancy in the reliability of this study.
Study results
Management of postpartum haemorrhage was in line with local protocols for each study; however, Amornpetchakul et al (2018) stated that management also depended on the clinician on duty at the time.
Amornpetchakul et al (2018) and Maged et al (2015) reported that carbetocin resulted in reduced postpartum blood loss. Furthermore, a meta-analysis found that carbetocin was as effective as oxytocin in preventing postpartum haemorrhage following a vaginal birth (Jin et al, 2019). It is important to note that both Amornpetchakul et al (2018) and Maged et al (2015) used a reduced dose (5IU of oxytocin given intravenously), compared to the other two. Widner et al (2018) stated that carbetocin was non-inferior to oxytocin, with 14.5% of participants allocated carbetocin experiencing a postpartum haemorrhage over 500ml, compared to 14.4% in the oxytocin group with a relative risk of 1.01. However, a recent study by Korb et al (2023), including 4832 women, found that carbetocin reduced the rates of postpartum haemorrhage over 500ml in comparison to oxytocin. Widner et al (2018) involved a larger number of participants compared to the three other studies, as shown in Table 2. A small sample is associated with reduced reliability and validity, and can be unrepresentative, highlighting further limitations to Maged et al (2015), Amornpetchakul et al (2018) and Hua et al (2020).
Maged et al (2015) found no considerable difference between the use of oxytocin and carbetocin in the incidence of major postpartum haemorrhage. Hua et al (2020) reported no notable difference between carbetocin and oxytocin in postpartum haemorrhage of over 500ml, 1000ml or in terms of average blood loss. However, Hua et al (2020) was the only study included in the review that was not carried out in a low- or middle-income country; therefore, there may be limitations when considering these results’ applicability to these settings. Widner et al (2018) stated that carbetocin was non-inferior to oxytocin in postpartum haemorrhage over 1000ml. This was the only study where the medications were given intramuscularly. However, it should be noted that Oladapo et al (2020) reported that oxytocin reduced the number of women with postpartum haemorrhage over 500ml when given intravenously, compared to intramuscularly, calling into question the validity of Widner et al's (2018) results.
Widner et al (2018), Maged et al (2015) and Hua et al (2020) found no notable differences between the oxytocin and carbetocin groups in terms of the number of participants who needed blood transfusions. Maged et al (2018) (P=0.401) and Hua et al (2020) (P=0.62) reported no statistically significant association between the variables and the requirement for blood transfusion. A study by Voon et al (2018) found that the use of carbetocin in caesarean deliveries reduced the need for transfusion, however more research would be required in relation to vaginal births. Hua et al (2020) reported that manual removal of the placenta occurred in 6.1% of participants in the oxytocin group, compared to 1.9% in the carbetocin group (P=0.01). Widner et al (2018) reported that 0.5% of participants in the carbetocin group required manual removal of placenta, compared to 0.6 in the oxytocin group, with relative risk of 0.83. Further research is needed into the use of carbetocin and oxytocin in relation to manual removal of the placenta.
Amornpetchakul et al (2018) reported that the carbetocin group was associated with a reduced rate of postpartum anaemia (P≤0.05). This is supported by Sotillo et al (2018), who found during caesarean sections in twin pregnancies, carbetocin was associated with a smaller reduction in haemoglobin level compared to oxytocin and hence led to fewer blood transfusions and uterotonics. However, Maged et al (2015) and Hua et al (2020) stated there were no differences in postnatal haemoglobin between the two groups. As these studies used small sample sizes, more research is needed into the use of carbetocin and oxytocin in relation to postnatal haemoglobin levels.
Maged et al (2015) and Amornpetchakul et al (2018) reported that the use of carbetocin decreased the need for additional uterotonics, with both reporting P<0.017. However, Widner et al (2018) found no substantial differences between the medications and the need for further uterotonics. Although Maged et al's (2015) and Amornpetchakul et al's (2018) studies reported statistically significant results, Widner et al (2018) was a large-scale study and discovered no substantial variation between the carbetocin and oxytocin groups, with a relative risk of 1, demonstrating reduced risk of bias. Furthermore, a study in Canada by Ben Tareef et al (2021) found that there was no difference in the need for additional uterotonics in the use of carbetocin or oxytocin. Additionally, Maged et al (2015) and Amornpetchakul et al (2018) used a lower dose (5IM) of oxytocin (compared to 10IM) than the other two studies making it difficult to compare results between the four studies. Additional research is required to assess the need for further uterotonics associated with oxytocin and carbetocin.
Conclusions
The use of carbetocin, instead of oxytocin, in low- and middle-income countries may reduce the risk of postpartum haemorrhage after vaginal birth and the need for additional uterotonics, but further research is required. However, the studies in this review assessed giving oxytocin and carbetocin via different routes and different doses, making it difficult for the author to compare findings. The literature available in low- and middle-income countries is limited, indicating a need for more research in this area. In low- and middle-income countries, where being able to maintain a cold chain to ensure the effectiveness of oxytocin can be challenging, carbetocin has been found to be non-inferior to oxytocin.
Key points
- Oxytocin is the preferred prophylactic uterotonic for postpartum haemorrhage.
- However, oxytocin is not heat-stable and requires a cold chain to avoid the risk of degradation, which is not always possible in low- and middle-income countries.
- Based on this literature review, the use of carbetocin could reduce the risk of postpartum haemorrhage; however, further research is needed.


