Maternal and infant mortality and morbidity have progressively declined in the last decade throughout the world (Moller et al, 2019), and there have been many improvements in the quality of maternity care in the UK. However, disparities remain between ethnic groups (Ameh and van Den Broek, 2011; National Audit Office, 2013; Matthews, 2015). Black, Asian and minority ethnic (BAME) women face limitations in access to maternity services in the UK and experience poorer health outcomes compared to white British women (Garcia et al, 2015). The most recent confidential enquiry into maternal mortality reported that black women are five times more likely; mixed-ethnicity women are three times more likely; Asian women are twice as likely to die in pregnancy then white women (Knight et al, 2019). Moreover, black women are up to twice as likely to have a stillbirth at all gestational ages (Muglu et al, 2019).
The UK's maternity services face many challenges due to the changing landscape of the population they serve and their evolving needs. In the 2011 UK census, 14% of the UK's population identified as BAME (Office of National Statistics, 2012) and ethnically diverse populations were predominantly concentrated in cities. Ethnic minority groups are among the most disadvantaged in the UK facing various social determinants of health including unemployment, poverty, inadequate housing, social exclusion and lower levels of educational attainment (Jayaweera et al, 2007; Marmot et al, 2010). Social and economic differences in society affect health inequalities whereby the most disadvantaged face more significant illness, disability and distress, and a shorter life expectancy (Whitehead, 1999; Dahlgren and Whitehead, 2006; Marmot and Bell, 2012).
Aim
This literature review aims to explore the maternal health inequalities encountered by BAME women in the UK in relation to their experiences and use of services. Stark health inequalities remain long-standing challenges for which specific and actionable targets are required (Marmot, 2005). However, to date, a systematic literature review has not been undertaken in the UK to identify the types of health inequalities faced by BAME women during the antenatal, intrapartum and postnatal period. A better understanding of the maternal health inequalities that BAME women face and how they impact on their health is necessary because a gap in literature creates barriers for meaningful policy making, improvement of maternity services and reductions in poor outcomes.
Method
A research question was formulated using PICO and an appropriate search strategy was developed. Five databases (PubMed, MEDLINE, CINAHL, MIDIRS and British Nursing Index) were systematically searched and a series of keywords applied, due to the known limitations in the literature. The keyword search utilised Boolean operators and truncation as follows; ‘BAME’ or ‘BME’ or ‘ethnic minority’, and, ‘pregnan*’ or ‘matern*’ or ‘antenatal’ or ‘postnatal’ or ‘intrapartum’ or ‘labour” or ‘perinatal’, and, ‘inequ*’ or ‘social determinant’ or ‘disparity’ or ‘experience’ or ‘mortality’ or ‘morbidity’. For inclusion into the literature review, eligible papers were available in English; were full-text articles in peer-review journals; based in the UK; were published between 2013–2018 for applicability to the current maternity system.
After the initial screening, the remaining articles' abstracts and titles were reviewed for their application to the aim of the review. The search process is illustrated in a PRISMA flow diagram (Liberati et al, 2009) in Figure 1. The final inspection resulted in eight articles for inclusion in the review.
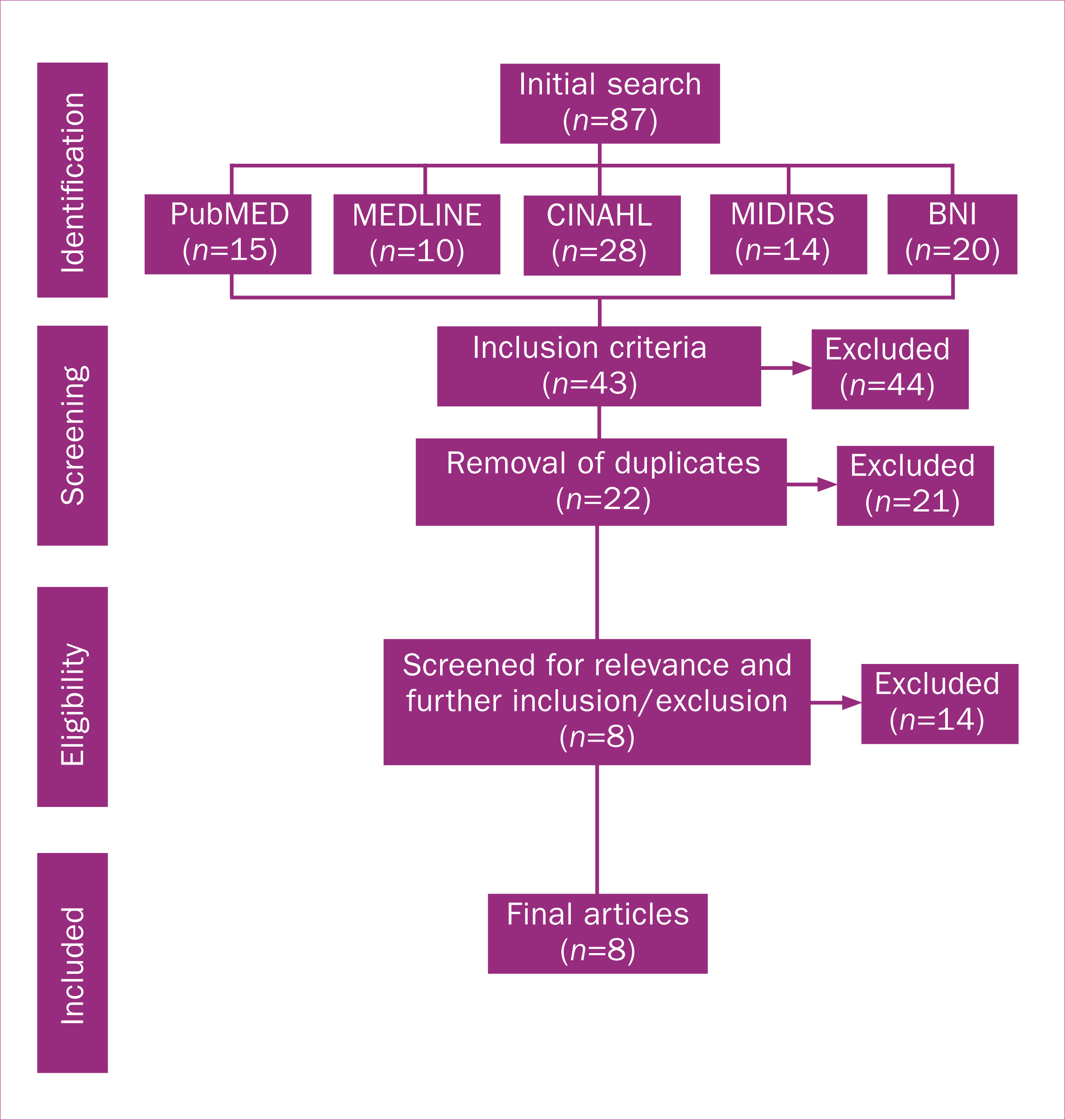 Figure 1. PRISMA flow diagram
Figure 1. PRISMA flow diagram
A data extraction template captured key methodological detail for each paper. Key findings were extracted, tabled and thematically analysed. During this iterative process, data was ordered and coded to identify preliminary themes that could be synthesised across the studies. Findings from the individual studies were indexed against these themes which were refined down to a second order. The methodological quality of the eight research papers was critiqued using two instruments; the Critical Appraisal Skills Programme (CASP, 2018) 10-item checklist for qualitative research and the National Heart, Lung and Blood Institute's (2018) 14-item quality assessment tool for cross-sectional studies. All eight studies demonstrated sound methodological quality.
Findings
A summary of the study characteristics of the final eight studies is presented in Table 1. The studies collectively sampled 24 645 women and 33 midwives. Three of the studies had large multi-ethnic samples (Henderson et al, 2013; Jomeen and Redshaw, 2013; McLeish and Redshaw, 2017) and five studies sampled women of specific ethnic backgrounds (Alshawish et al, 2013; Gardner et al, 2014; Aquino et al, 2015; Chinouya and Madziva, 2017; Goodwin et al, 2018). Most studies did not report whether participants were born in the UK or not. Five studies used exploratory, descriptive designs with qualitative methods (Alshawish et al, 2013; Gardner et al, 2014; Aquino et al, 2015; Chinouya and Madziva, 2017; McLeish and Redshaw, 2017), two were cross-sectional surveys (Henderson et al, 2013; Jomeen and Redshaw, 2013) and one remaining study was an ethnography (Goodwin et al, 2018). One of the surveys was of qualitative free-text responses and the other was a secondary analysis of a large quantitative dataset.
Table 1. Summary of study characteristics
| Author(s) and date | Sample and location | Research design | Identified themes | |
|---|---|---|---|---|
| 1 | Alshawish E, Marsden J, Yeowell G, Wibberley C (2013) | 22 Palestinian women in Manchester |
|
|
| 2 | Aquino MRJV, Edge D, Smith DM (2015) | 20 midwives in Manchester |
|
|
| 3 | Chinouya MJ, Madziva C (2017) | 23 black African women in London |
|
|
| 4 | Gardner PL, Bunton P, Edge D, Wittkowski A (2014) | 6 West African women in Manchester |
|
|
| 5 | Goodwin L, Hunter B, Jones A (2018) | 9 Pakistani women and 11 midwives in South Wales |
|
|
| 6 Henderson J, Gao H, | Redshaw M (2013) | 24 319 multi-ethnic women across the UK |
|
|
| 7 | Jomeen J, Redshaw M (2013) | 219 multi-ethnic women across the UK |
|
|
| 8 | McLeish J, Redshaw M (2017) | 47 multi-ethnic women across the UK |
|
|
Table 2 presents the five overarching themes that emerged from the synthesis of the eight studies and indicates inclusion of a theme within and between studies.
Table 2. Identified themes for each study
| Study | Themes | ||||
|---|---|---|---|---|---|
| Communication | Midwife-woman relationship | Maternity services and systems | Culture | Social needs | |
| Alshawish et al, 2013 | √ | √ | √ | ||
| Aquino et al, 2015 | √ | √ | √ | √ | √ |
| Chinouya and Madziva, 2017 | √ | √ | √ | ||
| Gardner et al, 2014 | √ | √ | √ | √ | |
| Goodwin et al, 2018 | √ | √ | √ | √ | √ |
| Henderson et al, 2013 | √ | √ | √ | √ | |
| Jomeen and Redshaw, 2013 | √ | √ | √ | √ | |
| McLeish and Redshaw, 2017 | √ | √ | √ | √ | |
Communication
Communication issues create barriers and are often oversimplified and misunderstood. Alshawish et al (2013) found that while Palestinian women's self-assessed, below-average language abilities contributed to poor health experiences in pregnancy, women who felt they had above-average language abilities also had poor experiences due to the use of medical terminology. Similarly, in a study by Gardener et al (2014), differences in the expression of symptoms and the terminology used meant that the identification of illness was often delayed or untreated. For example, West African women substituted the word ‘depressed’ with ‘stressed’, and despite describing the symptoms and experiences of postnatal depression (Gardener et al, 2014), they did not perceive this as an illness.
Aquino et al (2015) reported that midwives also use non-verbal communication during their assessments. Midwives report poor verbal and non-verbal communication as a significant barrier to establishing meaningful interactions and relationships with BAME women (Aquino et al, 2015; Goodwin et al, 2018). In addition to that, midwives' interpretation of non-verbal communication relies on their subjective experiences with BAME populations (Aquino et al, 2015).
According to Jomeen and Redshaw (2013), poor active listening skills by health professionals resulted in women feeling dismissed and unsafe. This lessened their involvement in decision-making; restricted the women's rights to make informed choices; and resulted in less pain relief and sub-optimal positioning during labour, regardless of whether the woman had experience from a previous pregnancy (Henderson et al, 2013; Jomeen and Redshaw, 2013). This is supported by McLeish and Redshaw (2017) that found the positive impact of active listening, or otherwise known as non-directive listening, meant that women were able to talk openly about concerns including any emotional distress.
The midwife-woman relationship
In a study by Goodwin et al (2018), the midwives and women who were interviewed recognised that any difficulty establishing a relationship between them could result in adverse pregnancy outcomes. However, midwives and women had different expectations for this relationship. Aquino et al (2015) noted that midwives tended to take a holistic approach whereas the women they cared for preferred professional and task-orientated relationships.
Jomeen and Redshaw (2013) found that predominantly negative previous experiences with midwives meant that women found it difficult to establish a relationship. The ‘condescending’ and ‘dismissive’ attitudes of midwives experienced by some women led to feelings of isolation and a perceived lack of care. Those who had previously positive encounters with a midwife were more likely to report positive pregnancy and labour experiences (Jomeen and Redshaw, 2013; Henderson et al, 2013). Furthermore, McLeish and Redshaw (2017) reported that a perceived lack of genuine interest in the women's emotional wellbeing, often due to a midwife's busy workload, resulted in distrust. Women also felt stereotyped if they had a diagnosed mental health problem and felt they were being observed for signs of failure which generated feelings of vulnerability.
Conversely, Aquino et al (2015) and Goodwin et al (2018) reported that midwives felt family relationships and cultural/religious practices affected their ability to develop relationships. Traditions and advice from matriarchs were given importance over their professional role. However, the women reported that it was the lack of early pregnancy contact and their poor understanding of the UK midwife's scope of practice that contributed to a poor midwife-woman relationship.
Maternity services and systems
Maternity services and systems refer to the logistical and organisational structures that contribute to the inequalities faced by BAME women. Midwives recognised that short appointment times created barriers for women due to time pressures and lack of flexibility from interpreting services (Aquino et al, 2015). Reportedly, it was difficult for interpreting services to be accessed and utilised effectively by women and midwives, especially in urgent situations, which meant family members had to interpret in their place (Alshawish et al, 2013; Aquino et al, 2015). The women interviewed by Alshawish et al (2013) felt that the lack of an interpreter resulted in postponement or delay in appointments which they perceived to affect the quality of their antenatal care.
Generally, BAME women had lower levels of engagement with maternity services in comparison to white women (Henderson et al, 2013). Goodwin et al (2018) reported that non-attendance at an appointment or a late booking was often misinterpreted by midwives as the women deliberately avoiding care and showing disregard for the maternity services. However, the attendance patterns could be explained by transport, domestic or interpreter difficulties. Some midwives acknowledged that disengagement was likely due to women not understanding verbal or written information about their appointments, which was exacerbated by poor interpretation services (Aquino et al, 2015).
Henderson et al (2013) identified that rates of late booking with maternity services were much higher amongst BAME women compared to white women. In studies by Chinouya and Madziva (2017), and Alshawish et al (2013), some women were unaware of the importance of booking before 13 weeks gestation, citing a lack of information, unfamiliarity with the UK's health system, cultural pressures and uncertain immigration status as causative factors. McLeish and Redshaw (2017) reported that women expected information to be openly advertised in GP settings or local community facilities, and noted that orientation to local services would have empowered and enabled the women to access them. Differences in the UK maternity services compared to a woman's native country contributed to poor engagement levels and late booking; the women were not used to scheduled appointments or being solely under midwifery led care (Alshawish et al, 2013; Goodwin et al, 2018).
Persistent staff shortages and time constraints in services meant that women's expectations of support were not met, leading to feelings of isolation, especially among women with mental health needs (Jomeen and Redshaw, 2013; Gardner et al, 2014; McLeish and Redshaw, 2017). Expectations of postnatal support were not met because BAME women were less likely than white women to see a midwife post-discharge from the hospital (Henderson et al, 2013; Gardener et al, 2014). Some women had also expected to see a midwife more often in the early stages of pregnancy, and as this service was not available to them, it led to perceptions of inadequate care (Jomeen and Redshaw, 2013; Goodwin et al, 2018).
Culture
In studies by Goodwin et al (2018) and Aquino et al (2015), midwives noted how some cultural and religious practices contradicted their policies and health advice, causing women and families to be dissatisfied with their care and the relationship with their midwife. Midwives, who were not able to establish a positive relationship with the women in their care, judged them harshly for their cultural choices. On the other hand, if a positive relationship had been established, the midwives viewed cultural practices more positively (Goodwin et al, 2018).
Stereotyping and a lack of cultural awareness by health professionals contributed to late bookings and a sense of feeling isolated among some women (Henderson et al, 2013; Jomeen and Redshaw, 2013). BAME women's attendance rates to antenatal classes were also lower than white women because men were in attendance, which was viewed as culturally inappropriate and made some women feel uncomfortable (Alshawish et al, 2013; Henderson et al, 2013). Lack of available childcare was another reason identified by the women for non-attendance.
Requests for cultural adjustments, such as requesting a female doctor, were not positively received by health professionals who found such requests time-consuming and a burden to their workload (Jomeen and Redshaw, 2013; Aquino et al, 2015). Disregard for women's cultural or religious needs resulted in a lack of individualised care that was neither sensitive nor responsive (Aquino et al, 2015).
Social needs
In the study by Goodwin et al (2018), some midwives felt frustrated by women who had complex social needs, such as referrals to housing or financial authorities, which led to negative stereotyping by the midwives. Nevertheless, women living in deprivation with social and financial difficulties found it difficult to access services (Gardner et al, 2014). Limited social connections and the lived experience of asylum, trafficking or recent migration created further social complexities. The lack of support from local communities or family meant that for some women, their expectations of the support they were to receive from health services, were raised (Gardner at al, 2014; McLeish and Redshaw, 2017) but not met.
Immigration status was also associated with late booking and presentation to maternity services, in the study by Chinouya and Madziva (2017), because women feared to alert authorities and risking deportation. GP services required women to present a passport but, instead, they would attend the hospital late or at the time of delivery. However, in the study by Aquino et al (2015) midwives did recognise the complex needs of pregnant, undocumented migrants and felt a commitment to advocate on their behalf.
Discussion
Health inequalities experienced by BAME women in maternity services are complex in and of themselves, and each identified theme overlaps with another. However, maternity services and systems are a principal theme across all studies with relationships to the remaining four themes of communication, midwife-woman relationship, culture and social needs. For example, due to service demands, midwives do not have the time, resources or flexibility to meet the needs of women who may require additional support because of communication needs, social complexities and accessibility challenges. Logistical problems, such as inadequate interpretation services or short appointment times (Alshawish et al, 2013; Aquino et al, 2015), create barriers between some BAME women, midwives and maternity services and systems. This subsequently impacts negatively on the type of relationship and rapport between women and their midwives. BAME women are at risk of feeling muted, irrespective of their language abilities, and it disrupts the midwife's ability to provide holistic care. Midwives need time to gauge the language and communication needs of women (NHS England, 2016) to provide effective care.
Furthermore, difficulties understanding the heterogeneous socio-cultural context of BAME women can foster stereotypical views in midwives (Henderson et al, 2013; Jomeen and Redshaw, 2013) which leads to service expectations being unmet among BAME women (Jomeen and Redshaw, 2013; Goodwin et al, 2018). Respecting women's cultures and circumstances can lead to greater engagement with services (NHS England, 2016). This requires services to engage with local communities and stakeholder groups to better understand these socio-cultural needs and improve organisational and interpersonal cultural competency.
Ethnicity based health inequalities can lead to differences in health status and access to services in multiple areas of maternity care. BAME women and midwives alike acknowledge that inequalities have an impact on health (Goodwin et al, 2018). However, the perceptions, expectations and experiences differ among women, midwives and services. To foster a cohesive understanding between women, midwives and services, a co-design approach is recommended (NHS England, 2017), and should be applied to address ethnicity based inequalities and improve women's experiences of care.
The formation and implementation of clear and inclusive national health policies and guidelines are imperative if maternity services are to be supported in tackling ethnicity based health inequalities. A small handful of policies broadly address ethnic minority women but the content and detail vary considerably (Puthussery, 2016) demonstrating a disconnect between policy and BAME women and communities.
The various health inequalities outlined in this review have been known for at least the last two decades (D'Souza and Garcia, 2004; Bharj and Salway, 2008) and are likely to have worsened (Marmot et al, 2020), yet, the review brings to light the lack of progress made to improve these known inequalities of BAME women accessing and receiving care from maternity services in the UK. The lack of progress highlights a failure towards BAME women and communities in the UK. Any future national policies must consider the needs of BAME women and communities, specifically and holistically, as well as supporting maternity care providers to modify the systems and services to meet these needs.
Limitations
The author acknowledges that the term BAME does not encapsulate the heterogeneity of people, ethnicities, or cultures in the UK. The acronym has been adopted in this review to remain consistent to the terminology and metric used in current literature. Additionally, the eight studies reviewed did not capture all ethnic minority groups that reside in the UK, nor did they cover a wide geographic area, hence limiting transferability of the results. However, the studies did demonstrate consistency amongst the themes identified in this review. Furthermore, all eight studies included in the review did not aim to study health inequalities, rather the inductive thematic analysis of this review generated these themes. This review was conducted in part-fulfilment of a master's qualification and was therefore bound by time and resource restrictions. Lastly, the lack of literature exploring health inequalities experienced by BAME women accessing maternity care in the UK is the main limitation of this review.
Conclusion
In conclusion, this review identified BAME women encounter five persistent areas of inequality that could impact their experiences and use of services. The review has highlighted that maternity services and systems, as a predominant theme, perpetuates inequalities yet it can be modified through effective policy making and service implementation. A recommendation for future research would be to explore maternity service or system interventions that aim to reduce the aforementioned ethnicity based health inequalities. All five themes begin to offer a potential explanation to known differences in morbidity and mortality rates of BAME women in the UK, compared to white women, though detailed analysis and robust research is required to understand causality.
Lastly, this review offers a renewed understanding of experiences and health inequalities from the perspectives of midwives and BAME women as sampled in the eight studies. The findings and themes presented in this review may well inform midwives, researchers and policy makers of priority areas for research and service improvement, and finally begin to reduce the gap in ethnicity based health inequalities.
Key points
- While black, Asian and minority ethnic (BAME) women have significantly higher rates of maternal morbidity and mortality in the UK, it is not fully understood why
- There is a lack of robust literature in relation to the inequalities experienced by BAME women in the UK
- This literature review found five persistent themes; communication, midwife-woman relationship, maternity services and systems, culture and social needs, which impacted BAME women's experiences and use of services
- Maternity services and systems is a predominant theme that overlapped and influenced with the remaining four themes
- Although maternity services and systems are modifiable through policy, there has been no improvement in the experiences and use of services for BAME women in the last decade and beyond
- The author recommends a co-design approach with BAME women and communities to improve experiences and use of maternity services
CPD reflective questions
- What competing challenges do midwives face when caring for black, Asian and minority ethnic (BAME) women?
- What are some of the reasons for BAME women's reduced engagement with maternity services?
- As a midwife how can you improve your professional relationship with BAME women?
- Reflecting on the maternity service you provide, are there similarities with the literature reviews findings?
- After reading this literature review, what is one change you will make to improve the experiences of BAME women?


