The national maternity review in England, Better Births, recommends that all women should have a named midwife to care for them through pregnancy, birth and the postpartum period, in order to provide safe, joined up services (National Maternity Review, 2016). This transformative work has an established evidence base, and has reduced regional anaesthesia, instrumental or caesarean birth, pregnancy loss and preterm birth. It has also provided women with the reassurance of having continuity of a midwife or midwifery team (Sandall et al, 2016).
The purpose of this evaluation was to measure changes that arose from implementing a continuity of carer approach, in terms of a complicated or uncomplicated birth. The original outcomes defined by the North-West London team included:
Other outcomes were:
Secondary outcomes included the place of delivery. This article concentrates only on changes to complicated births (ie caesarean or instrumental versus spontaneous vaginal birth), as the focus was on potential cost savings using the 2017-18 NHS tariff. A more detailed evaluation was carried out by Imperial College Health Partners, which looked at all the primary and secondary outcomes described; here the focus is only on outcomes affecting the complicated or uncomplicated tariff.
The North West London partnership serves over two million residents. There are more than 29 000 births each year, with marked ethnic diversity across the area, and high levels of deprivation (North West London Sustainability and Transformation Partnership, 2016). The area was allocated £900 000 of transformation funding in 2017-2018 to establish the early adopters programme across the six maternity units (NHS England, 2019). The programme started at different times across the maternity units, so data were obtained from the first 6 months to 1 year of implementation.
There was a dedicated central programme team, comprising an implementation lead, four midwifery project managers and a project support officer. Clinicians and managers from each Trust worked with commissioners, GPs and other allied professionals to test new models of continuity of carer according to the Better Births recommendation. Women and their families participated in designing the programme, so that it was strongly influenced by their views.
Background
The different continuity models are described in Table 1, with Model 1 further divided into bespoke care for low-risk women (1a), socially complex women (1b) and women with previous gestational diabetes (1c). The North-West London early adopters' steering group collaborated with each maternity unit to agree and deliver the different community- and hospital-based caseload continuity of carer models.
| Model | Maternity unit | Details |
|---|---|---|
| Model 1a: low-risk uncomplicated women | Chelsea and Westminster Hospital (6000 births per year), Chelsea and Westminster and West Middlesex Trusts (merged) |
|
| Model 1b: socially complex women | St Mary's Hospital (3000 births per year) and Queen Charlotte's Hospital (5000 births per year), Imperial College Healthcare NHS Trust | |
| Model 1c: women with previous gestational diabetes | West Middlesex Hospital (5000 births per year) |
|
| Model 2: delivering continuity of care to women in a hospital, birth centre-based, continuity model | Northwick Park Hospital (5000 births per year), London North West University Healthcare NHS Trust |
|
Methods
Imperial College Health Partners described the change management approaches involved in implementing the early adopters model in North-West London (Imperial College Health Partners, 2019). Better Births identified that teams of midwives working to provide continuity in autonomous units may need:
‘Educational support around how to work together successfully in a small team, how to be supportive, how to challenge, how to reach consensus, and how to self-manage.’
The project has been described in an Early Adopters Toolkit (North West London Local Maternity System, 2019), listed as ‘Case Study H’. As a result, Imperial College Health Partners (2019: 14), which described the change management approaches involved in implementing the early adopters model in North-West London, noted that:
‘The programme team aimed to meet this need through regular training events throughout the programme. Team coaching was delivered to 15 teams across North West London, reaching over 100 midwives. Coaching was provided by in-house change coaches and an experienced midwife team coach commissioned by the programme team. A separate evaluation of this intervention proved that coaching had a positive impact on building trust and stability within the teams. Additional funding provided by Health Education England enabled the Local Maternity System (LMS) to secure a bespoke training package to be delivered to approximately 100 midwives in the sector.’
Study settings and continuity of carer models
Low-risk women (Chelsea and Westminster Hospital)
This programme started in February 2018 with a team of six midwives. Most antenatal care, and all postnatal care, was provided at home. Data were obtained from March 2018 until September 2018.
Socially complex women (Queen Charlotte's Hospital and St Mary's Hospital)
Women with social issues were identified in the two intervention hospitals. A matched group (ie socially complex women not receiving continuity of care) was found in women at Chelsea and Westminster Hospital. Low-risk women with home births, whose data were interspersed in the caseload, were removed, as their outcomes were not directly relevant. Although the socially complex model in these hospitals was already well-established, the added funding enabled a broader approach to be taken for these vulnerable women. This cohort also included some women without risk factors who opted for homebirth, in order to reduce the pressures on community services.
Women with gestational diabetes (West Middlesex Hospital)
This programme started with six midwives. Most antenatal and all postnatal care was provided at home, and women were supported with the specialist intervention if they booked into the unit between March and October 2018 and had been previously affected by gestational diabetes. The cohort was matched by similar women booking into the unit in 2016-17.
Birth centre midwifery model (Hillingdon Hospital and Northwick Park Hospital)
Hillingdon and Northwick Park Hospitals tested a birth centre-based continuity model, with a dedicated midwife from the antenatal period, to the postnatal period.
Findings
Low-risk women (Chelsea and Westminster Hospital)
The proportion of women with a complicated (defined as a caesarean or instrumental birth) versus an uncomplicated (spontaneous vaginal) birth can be compared. In this cohort, 43 of 116 women (37% of those with known outcome, 32% of total) had a complicated birth, while 32 of the 77 matched women (42%) had a complicated birth. This difference was not statistically significant (Table 2).
| Type of birth | Intervention cohort | Matched cohort | P-value† | ||
|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | ||
| Complicated | 43 | 32 (25–41) | 32 | 42 (31–53) | 0.531 |
| Uncomplicated | 73 | 55 (46–63) | 45 | 58 (47–69) | |
| Outcome unknown | 17 | 13 (8–20) | 0 | 0 (0–5) | |
| Total | 133 | 100 | 77 | 100 | |
complicated vs uncomplicated
The feedback below summarises some reflections of women under their care:
‘She explained things really thoroughly and the conversation was continuous so we continued on where we left off.’
‘What was incredible was that I could text her if I was genuinely worried about something and that was really reassuring, just another efficiency [sic] that she could answer questions specifically about me.’
‘She involved my husband too, it made him at ease too … he was at all appointments so built up a relationship with her which helped him too, and how he could help me.’
‘If I hadn't had that relationship with her I think my whole birth experience would have been much more stressful and difficult.’
Socially complex women (Queen Charlotte's Hospital and St Mary's Hospital)
Comparing the proportion of women with a complicated and an uncomplicated birth shows that for the socially complex women with a caseload midwife, 43% of women (94 of 221) with a known outcome had a complicated birth, while 36 of the 69 women in the matched cohort (non-continuity model, known outcomes) (42%) had a complicated birth. This was not statistically significant (Table 3).
| Type of birth | Intervention cohort | Matched cohort | P-value† | ||
|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | ||
| Complicated | 94 | 31 (26–36) | 36 | 42 (32–53) | 0.160 |
| Uncomplicated | 127 | 42 (36–48) | 33 | 39 (29–49) | |
| Outcome unknown | 82 | 27 (22–32) | 16 | 19 (12–28) | |
| Total | 303 | 100 | 85 | 100 | |
complicated vs uncomplicated. Source: Queen Charlotte Hospital and Imperial maternity units
Women with gestational diabetes (West Middlesex Hospital)
Births among women with gestational diabetes are complex by definition, so having one-to-one support does not mitigate against a complicated birth. The findings showed that the proportion of complicated births did approach statistical significance, with a higher proportion of complications in the intervention group (48 of 98; 51%) than the control group (28 of 81; 35%) (Table 4).
| Type of birth | Intervention cohort | Matched cohort | P-value† | ||
|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | ||
| Complicated | 48 | 40 (32–49) | 28 | 35 (25–45) | 0.052 |
| Uncomplicated | 50 | 42 (34–51) | 53 | 65 (55–75) | |
| Outcome unknown | 21 | 18 (12–25) | 0 | 0 (0–5) | |
| Total | 119 | 100 | 81 | 100 | |
complicated vs uncomplicated
Number of antenatal and postnatal outpatient appointments
With the implementation of the new model, there was a reduction in obstetric antenatal clinic appointments, as women receiving support as part of the intervention had, on average, fewer outpatient appointments than women in the matched cohort (3.6 vs 5.3). Postnatal visits were at home with a midwife. Women who received bespoke support from a midwife as part of the intervention had, on average, fewer postnatal appointments than women in the matched cohort (4.8 vs 6.4). This allowed valuable midwifery time to be spent on other tasks.
Breastfeeding
The breastfeeding rates of the intervention cohort at West Middlesex Hospital cohort were greater than in the control group, with 56 of the 66 (85%; CI 76–94%) women exclusively breastfeeding when discharged to a health visitor, compared with 25 of the 69 women in the matched group (36%; CI 25–47%). This was statistically significant, although breastfeeding outcomes were not known for all women. This will have proven benefits in terms of mother to baby bonding and passive immunity (as well as reduced risk of complications such as future type 2 diabetes in mother and child).
Glycaemic control
In terms of glycaemic control, women under the specialist midwifery team had higher levels of diet-only control than the matched cohort (53% vs 35%). Of the 88 women in the specialist diabetes midwifery-supported cohort, a lower proportion were on metformin only (25%) compared with the control group (40%). The proportion of women on insulin, however, was higher in the women in the intervention cohort. These differences achieved statistical significance when tested (P<0.001) (Table 5).
| Type of birth | Intervention cohort | Matched cohort | P-value | ||
|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | ||
| Diet-only control | 47 | 53 (43–63) | 27 | 35 (24–44) | <0.001 |
| Metformin | 22 | 25 (17–35) | 32 | 40 (30–50) | |
| Metformin & insulin | 11 | 12 (7–21) | 21 | 25 (18–36) | |
| Insulin | 9 | 10 (5–18) | n=* small | <5 (0–7%) | |
| Total | 88 | 100 | >80 | 100 | |
Women had the following positive reflections on their support with their gestational diabetes care:
‘Yes, they were always there for me, understanding and friendly, they saw me at home which was helpful because I have children.’
‘This is my third baby, my first time being cared for by [intervention] team, and I wish I had had this care with them all!’
‘I loved everything about the care. The home visits were very convenient. The continuity of the care by the same midwife, who was a wonderful midwife, was also great’
‘Yes, I really built up a great bond with my midwife and instantly relaxed when she arrived’
This is similar to an Australian study of over 2300 women's views of their midwifery care, which showed that for low-risk women, continuity was associated with increased satisfaction antenatally, in birth, and postpartum (Forster et al, 2016).
Birth centre midwifery model (Hillingdon Hospital)
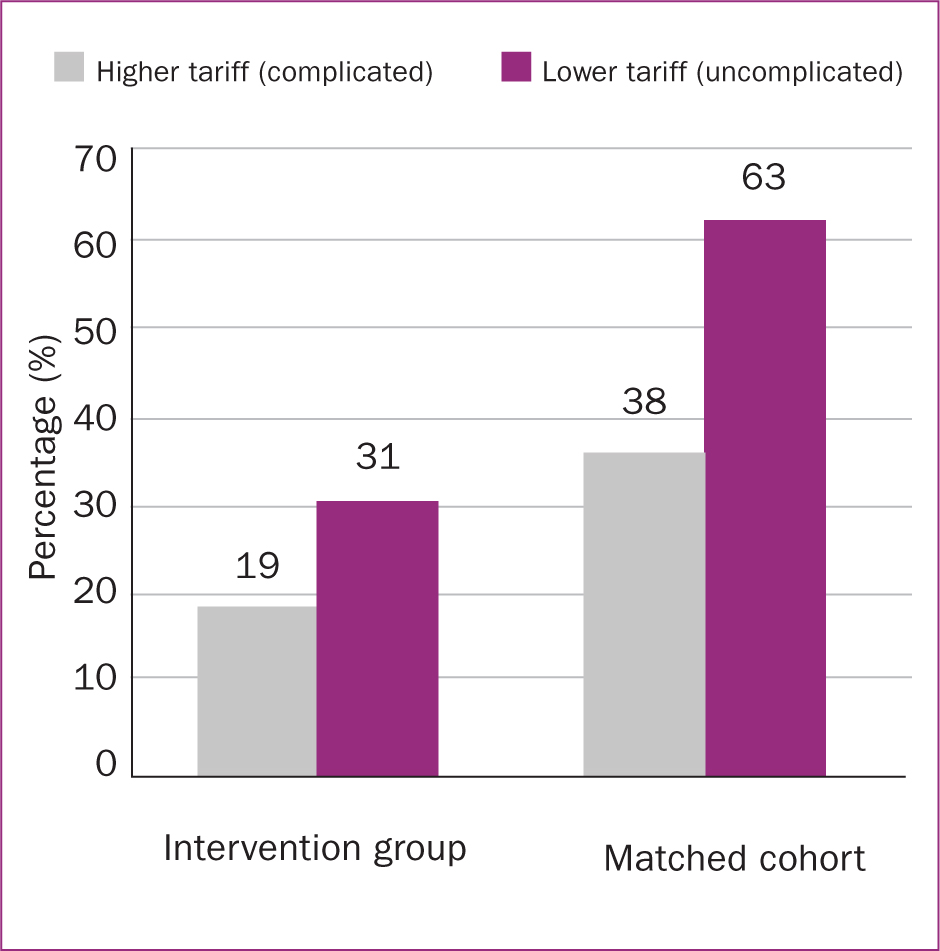
Comparing the proportion of women with a complicated and an uncomplicated birth shows that 36 of the 96 (38%) women with a named midwife at Hillingdon Hospital had a complicated birth, similar to the matched cohort (Figure 1 and Table 6).
| Type of birth | Intervention cohort | Matched cohort | P-value† | ||
|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | ||
| Complicated | 36 | 19 (14–25) | 36 | 38 (28–47) | 1.00 |
| Uncomplicated | 60 | 31 (25–38) | 60 | 63 (53–72) | |
| Not known | 97 | 50 (43–57) | 0 | 0 (0–4) | |
| Total | 193 | 100 | 96 | 100 | |
complicated vs uncomplicated. Source: Hillingdon Hospital
Birth centre midwifery model (Northwick Park Hospital)
Comparing the proportion of women with a complicated and an uncomplicated birth shows that 58 of the 149 (39%) women at Northwick Park Hospital had a complicated birth, while 34% of the matched cohort had a complicated birth. This was not statistically significant (P=0.402) (Table 7).
| Type of birth | Intervention cohort | Matched cohort | P-value† | ||
|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | ||
| Complicated | 58 | 29 (23–35) | 39 | 34 (26–43) | 0.402 |
| Uncomplicated | 91 | 45 (38–52) | 76 | 66 (56–74) | |
| Not known | 53 | 26 (21–33) | 0 | 0 (0–3) | |
| Total | 202 | 100 | 116 | 100 | |
complicated vs uncomplicated. Source: Northwick Park Hospital
Discussion
There is strong evidence for continuity of carer: Sandall et al (2016) demonstrated reduced need for regional analgesia and instrumental birth, as well as an improved experience for women. Evidence shows that giving birth in midwifery-led settings is as safe as giving birth in an obstetric led unit, with a significantly decreased chance of interventions (Birthplace in England Collaborative Group et al, 2011).
This study shows that setting up models of care mirroring those in North-West London is possible, with good investment in infrastructure and clinical commitment from a multidisciplinary team. There was no significant difference in complicated births in Chelsea and Westminster Hospital with the new model, although this maternity unit cares for a particularly affluent cohort of women, with lower levels of social complexity, so it may be more difficult to effect changes in outcomes.
The literature shows that for women with complex social needs—especially for teenagers under the care of Family Nurse Partnership programmes—there is an established evidence base (National Institute for Health and Care Excellence, 2010) to show that continuity of carer works. Such trusted midwifery care enables long term benefits, including better pregnancy and parent outcomes, and improved child health outcomes, such as school readiness and educational attainment (Family Nurse Partnership, 2019). For women with complex needs at Queen Charlotte's and St Mary's hospitals, there was also no statistically significant difference in the number of complicated births with the specialist support, although for such a vulnerable group of women, more complex interventions including from social care, may be needed in order to make a difference.
Although diet-only control for women with gestational diabetes increased with the specialist intervention, insulin use was also significantly higher for those who had the bespoke care. The use of metformin reduced significantly for women in the intervention group, possibly because women who ordinarily needed metformin were able to be control their diabetes using diet. In an East London audit of midwife-led multidisciplinary care versus acute Trust-led multidisciplinary care for women with gestational diabetes, the authors found that clinic attendances during the first 6 months were reduced by 50% (Jones and Wilson, 2010).
A systematic review of 15 trials (17 674 women) showed that women with midwife-led continuity experienced a significantly lower probability of regional anaesthesia, episiotomy, instrumental birth and fetal loss before 24 weeks' gestation (Sandall et al, 2016). These findings were not supported by the data from Hillingdon or Northwick Park hospitals, where the new team model reduced the proportion of complicated births, but not to a significant level. It would be interesting to explore why, although the difference could be spurious given the large number of missing outcomes for women.
Limitations of this study
A large number of outcomes could not be ascertained for women in the intervention groups. This will have the effect of reducing the proportion of births in both the uncomplicated and complicated groups, although it is not known whether the effect was unequally distributed so as to under- or overestimate the difference with the control group. Tests for statistical significance have been performed comparing complicated to uncomplicated births only, so as not to be skewed by the differences in missing outcomes data between intervention and control groups. However, the potential for bias in these results must be acknowledged. In addition, some of the comparison groups had small sample sizes, so there may not have been sufficient power to detect a statistically significant difference in birth outcomes.
From a logistical perspective, each midwife had to manually enter the data onto a Microsoft Excel spreadsheet that was then analysed, and this method means that it may be easy to miss data. Hospital maternity IT systems that can extract data and populate the fields automatically are recommended in order to inform future audits, to save midwives' time and ensure the datasets are more complete.
Conclusions
The findings were mixed in terms of being able to support the Better Births findings on reducing complicated birth. However, this evaluation wass limited by incomplete datasets, short time frames of 6-12 months, smaller comparison groups and unknown outcomes. Given the context of the evaluation in checking whether reduced complicated births would lead to reduced tariffs, no differences were found in each hospital. Some positive findings were found, including women's views, increased breastfeeding and increased dietary control in women with gestational diabetes. In future, evaluations would be easier if data entry did not have to be manually and retrospectively entered by midwifery staff, and if it could be extracted automatically from hospital records.

