How to have the ‘ideal’ Down syndrome screening discussion at antenatal appointments
This paper discusses the findings of the previous three papers in this series (John et al, 2019a; 2019b; 2020). From the results, the authors make recommendations regarding the information that needs to be communicated in booking appointments and the approach midwives should take in order to accomplish an ‘ideal’ Down syndrome screening discussion (Figure 1). At the centre of an ‘ideal’ consultation is a woman-centred approach, which is recommended for midwifery care (Department of Health [DoH], 2007; Nursing and Midwifery Council [NMC], 2015; National Institute of Health and Care Excellence [NICE], 2019).
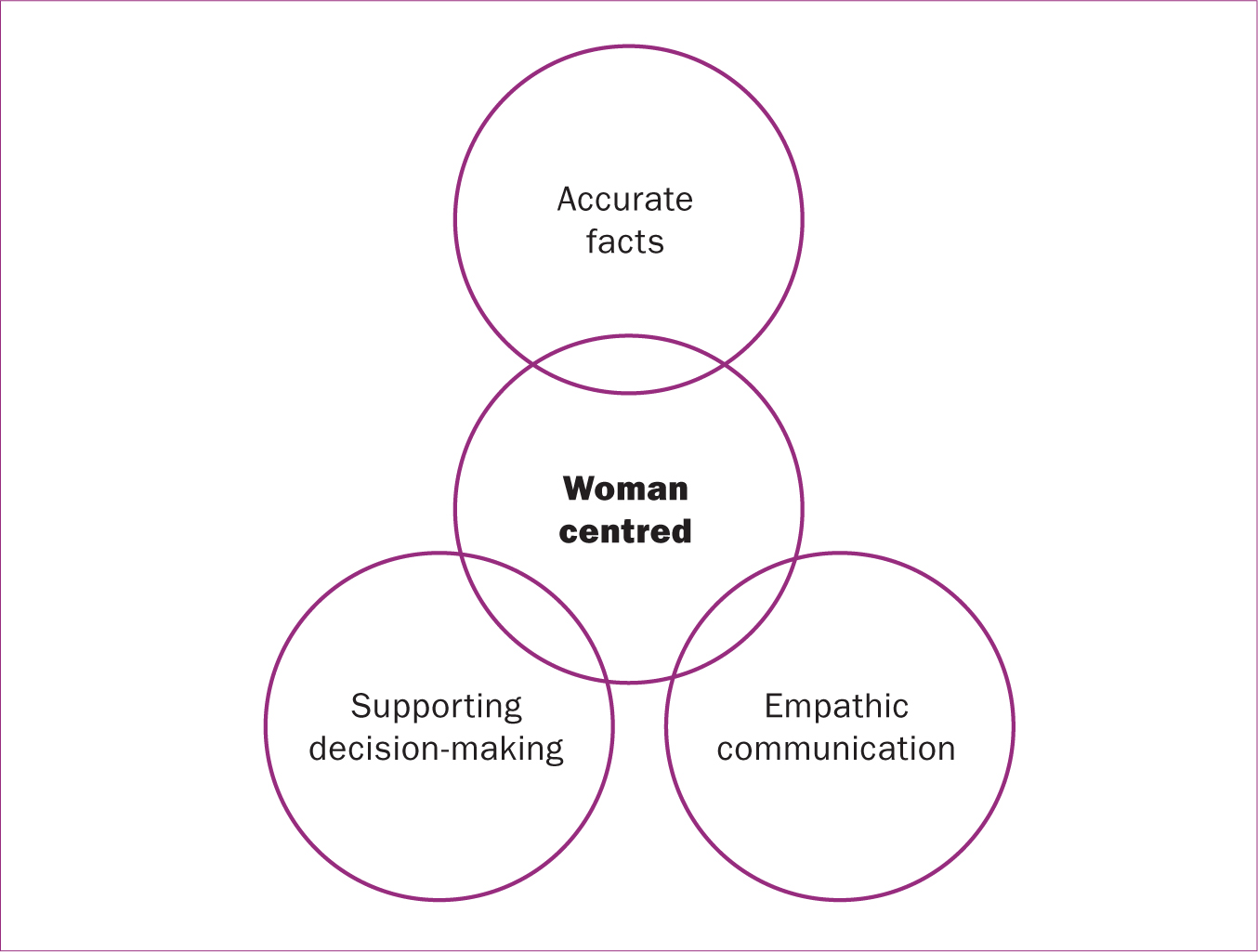 Figure 1. The components of an ‘ideal’ Down syndrome discussion
Figure 1. The components of an ‘ideal’ Down syndrome discussion
Three overarching conceptual themes have been identified which could constitute an ‘ideal’ Down syndrome discussion (Figure 1). Within each theme, different recommendations for midwife communication are outlined (bold text in Table 1). The proposed midwifery guidelines encompass the five aspects of midwife communication included in measuring understanding of screening information and communication (MUSIC) framework (John et al, 2019a), and incorporates guidelines that already exist from Antenatal Screening Wales (2015), NMC (2015) and NICE (2019), and new recommendations (Table 1), based on the results of this research, which are discussed further in subsequent sections.
Register now to continue reading
Thank you for visiting British Journal of Midwifery and reading some of our peer-reviewed resources for midwives. To read more, please register today. You’ll enjoy the following great benefits:
What's included
-
Limited access to our clinical or professional articles
-
New content and clinical newsletter updates each month

