There has been a resurgence in pertussis, with the highest incidence and complication rates in young infants, and deaths occurring mainly before 3 months of age (Healy, 2016). The most effective way to protect young infants, who are disproportionately burdened by pertussis, is through maternal vaccination (Omer, 2017). In response to increasing pertussis incidence in infants in New South Wales (NSW), Australia (Nicholl et al, 2018), NSW Health implemented a maternal pertussis vaccination scheme, offering diphtheria, tetanus and pertussis vaccines to all women in their third trimester of pregnancy.
Previous studies have reported on the importance of educating health professionals to improve maternal vaccination rates (Eppes et al, 2012; 2013; Kfouri and Richtmann, 2013), which is vital to the success of a vaccination programme (Wiley et al, 2013a). The decision of a pregnant woman to consent to vaccination relies on how much importance the midwife places on the vaccine, which also determines the midwife's level of engagement in programme implementation (Robbins et al, 2011). An Australian study found that midwives' perceived self-efficacy regarding vaccination was the most important factor in the vaccination of postpartum mothers (Robbins et al, 2011). When discussing immunisation with pregnant women, it is important to state that it offers protection for both the infant and the woman, as this may increase vaccine uptake (Wiley et al, 2015). Midwives therefore need to be well informed and prepared to address women's concerns as well as increasing women's confidence and trust.
Before implementing the new programme, NSW Health liaised with clinical midwives in the local health districts to seek their assistance with programme development. There was a need for an online educational module for midwives (Nicholl et al, 2018); a 30-minute online module was therefore developed in collaboration with the Health Education and Training Institute (HETI), a statutory health corporation that offers education and training to improve the health of NSW people and the working lives of NSW Health staff.
Unpublished data from the 2012 NSW Perinatal Data Collection (accessed via Secure Analytics for Population Health Research and Intelligence (SAPHaRI) on 30 January 2015) on the models of care used by women were provided to Health Protection NSW to review and indicated that more than 40% of women were attended by a hospital-based midwife and more than 61% used a hospital medical/midwife model of care. In comparison, 17% were attended by their doctor and 32% by their private obstetrician. Therefore, during the planning phase of the new vaccination programme, it was considered important to provide support and guidance to midwives, to enable consistent and effective implementation and to promote optimal vaccine uptake.
Introducing a new antenatal vaccination programme to an already busy clinic routine is a challenge and requires midwives' knowledge, confidence, acceptance and motivation to embed it into routine antenatal care. It is acknowledged that introducing a new vaccination programme will require time to become widely accepted as a standard of care (Castagnini et al, 2012). An Australian study in NSW found that, compared to other hospital nurses and primary care immunisation providers, midwives had a lower confidence in vaccination requirements and safety (Leask et al, 2008). A successful programme can be achieved if midwives are confident and competent in all aspects of vaccination management, including vaccine storage, pre-vaccination assessment, vaccine administration and post-vaccination care. Although registered nurse and midwifery accreditation standards for education providers must include the appraisal of competence in medication administration (Nursing and Midwifery Board of Australia, 2017), vaccination management requires specialist knowledge to ensure vaccine acceptance, safe and efficacious administration and high vaccine uptake (Kfouri and Richtmann, 2013; Meharry et al, 2013; Kharbanda et al, 2014; Maertens et al, 2016a).
Education module
A 30-minute online educational module was developed in consultation with HETI and an expert reference group that included midwives. Module production included an instructional strategy, design plan and storyboard that included aspects such as the subject area, key learning outcomes, performance gaps, artwork style and project plan. Seven key learning outcomes associated with vaccination management for pregnant women were identified, namely:
The importance of influenza vaccination during pregnancy was also included in the module, although this is not a new recommendation for pregnant women. The interactive training was scenario-based, to encourage learners to explore different responses and uncover pockets of knowledge at various encounter points. All components of the module needed to be undertaken before a completion certificate was granted. The module was released on 31 March 2016 and all local health district Chief Executives were requested to disseminate it to midwives employed in their district. Although the module predominately targeted midwives as the key clinicians responsible for implementing the antenatal pertussis vaccination programme in NSW Health public facilities, other clinical staff such as doctors and registered nurses also had access.
Aim
This study aimed to determine if a new online education module for antenatal pertussis vaccination was effective in meeting the needs of midwives and maternity staff in NSW, and whether it increased their confidence to deliver the NSW antenatal pertussis vaccination programme and promote high vaccine uptake.
Methods
Pre- and post-surveys
Pre- and post-surveys were developed, each consisting of six closed questions with additional free-text fields. Both surveys were completed anonymously and no personal identifying information was collected. The pre-survey asked respondents about their previous experience in vaccinating adults and children; their level of confidence in managing the various components of vaccination management; and how they viewed providing advice to the woman regarding future immunisation requirements for her and her infant. The post-survey asked respondents to rate the components of the module and their confidence in conducting a vaccination appointment with a pregnant woman. It also requested demographics of their age, role and work location. The survey responses were not linked to each other and users were provided with the option of completing one or both. The surveys were available online between 31 March 2016 and 21 April 2017 for any clinician employed in a NSW Health facility. Participants were invited to complete the module via a letter from the Chief Health Officer to each district's Chief Executive Officer, who was asked to disseminate information about the module to all relevant staff. Once participants logged into the learning management system, they were invited to participate in the surveys via a link to a participant information sheet. Participation was voluntary and respondents were advised that clicking on each survey link and completing the survey was considered valid consent. Following closure of the surveys, data were extracted into Excel, checked for completeness, cleaned and transferred to SPSS version 24. Descriptive statistics of the responses were generated and expressed as absolute and relative frequencies. Free-text field data were grouped in categories and cross-checked by the authors. A P value of <0.05 was considered significant for results on chi-squared (c2) tests of association between categorical data.
Ethics approval was granted by the Human Research Ethics Advisory Panel, University of New South Wales, Sydney, Australia (approval number HC15642).
Results
Module completions
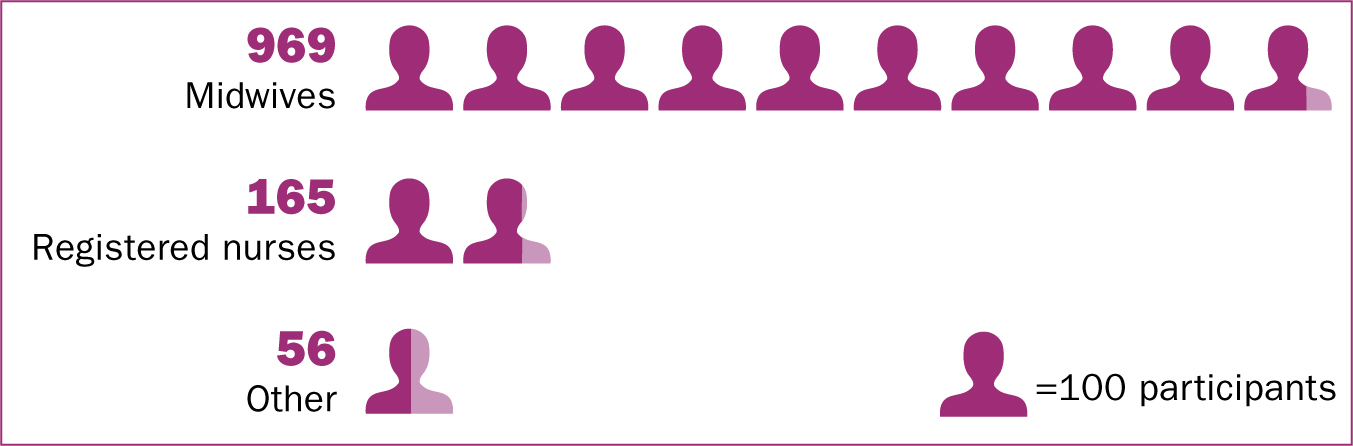
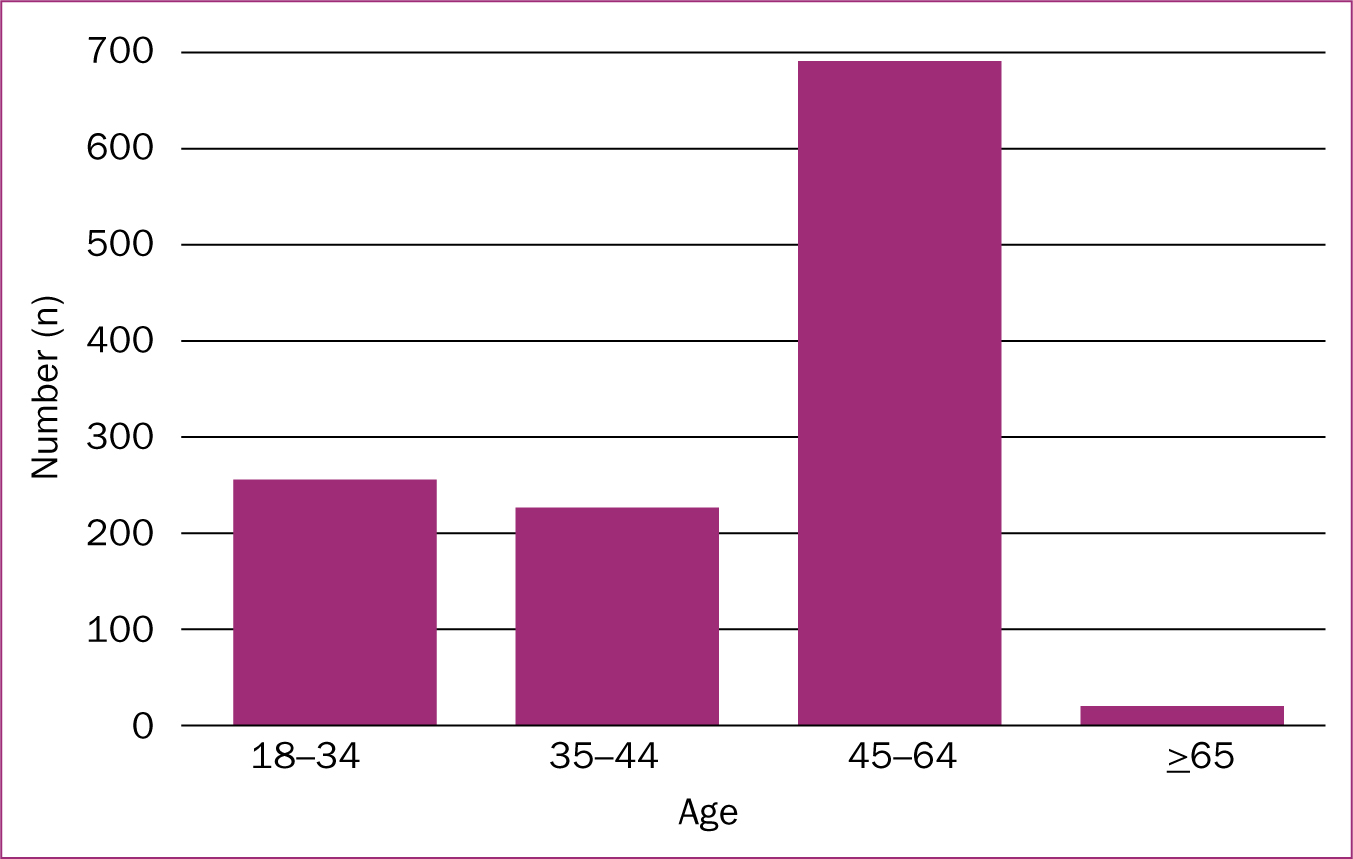
A total of 1695 HETI modules were completed between 31 March 2016 and 21 April 2017 from all districts in NSW. Of the estimated 3400 midwives employed in NSW public facilities (NSW Health state-wide payroll system, June 2017), 1144 (37%) completed the module. The remaining completions were performed by registered nurses (n=459) and other professionals (n=92).
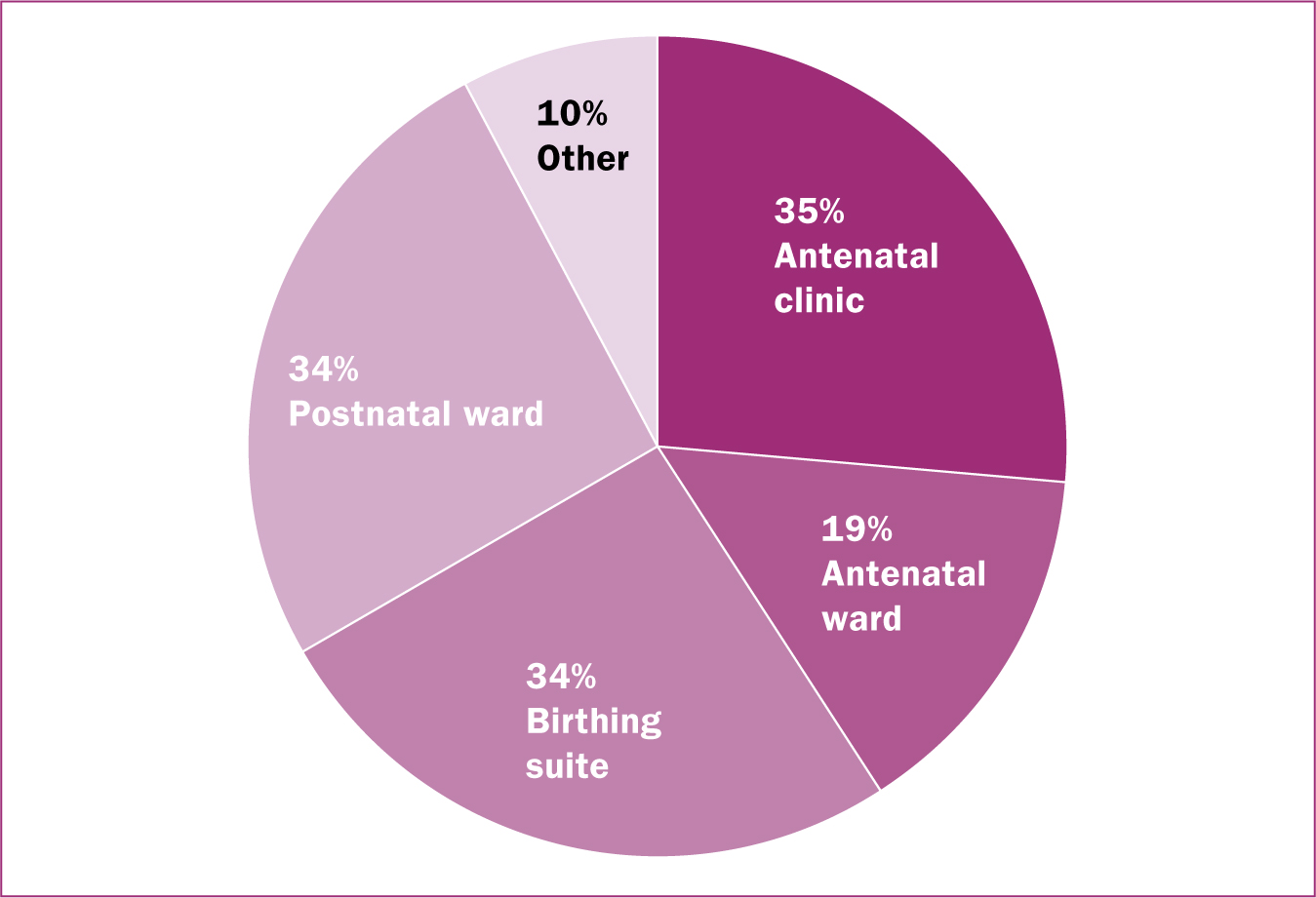
There was a wide variance in the pre- and post-survey completions by district, which ranged from 10–90% for pre-survey completions, compared to 45–96% for post-survey completions. The responses of both surveys are summarised in Table 1 and Figures 1–3.
| Confidence in performing immunisation encounter components | n (%) | Previous experience in vaccinating adults n=602 (86%) | Previous experience in vaccinating children n=495 (71%) | ||
|---|---|---|---|---|---|
| χ2 | P-value* | χ2 | P-value* | ||
| Pre-vaccination assessment | |||||
| Very confident/confident | 353 (50.6) | 55.0 | P<0.01 | 33.1 | P<0.01 |
| Somewhat confident/slightly confident | 307 (43.9) | ||||
| Not confident at all | 38 (5.5) | ||||
| Managing vaccine storage and cold chain | |||||
| Very confident/confident | 410 (58.8) | 49.1 | P<0.01 | 31.3 | P<0.01 |
| Somewhat confident/slightly confident | 259 (37.1) | ||||
| Not confident at all 29 | (3.7) | ||||
| Administering vaccines to pregnant women | |||||
| Very confident/confident | 471 (67.5) | 87.3 | P<0.01 | 30.8 | P<0.01 |
| Somewhat confident/slightly confident | 185 (26.5) | ||||
| Not confident at all | 42 (6.1) | ||||
| Post-vaccination care | |||||
| Very confident/confident | 346 (49.5) | 46.3 | P<0.01 | 29.7 | P<0.01 |
| Somewhat confident/slightly confident | 307 (43.9) | ||||
| Not confident at all | 45 (6.4) | ||||
| Immunisation advice to mother regarding her and her infant's immunisations after birth | |||||
| Very confident/confident | 413 (59.1) | 63.1 | P<0.01 | 44.5 | P<0.01 |
| Somewhat confident/slightly confident | 245 (35.1) | ||||
| Not confident at all | 40 (5.7) | ||||
Before undertaking the module, participants were asked to state their perceived level of confidence in various aspects of the vaccination encounter. Overall, 57% (n=398) reported feeling ‘confident’ or ‘very confident’ in all aspects of vaccination management. When asked to report their confidence in the various aspects of the vaccination appointment, 67.5% (n=471) reported feeling ‘confident’ or ‘very confident’ in administering a vaccine to a pregnant woman; 43.9% (n=307) reported feeling ‘somewhat or slightly confident’ in performing a pre-vaccination assessment and providing post-vaccination care. Just over one-third reported feeling only ‘somewhat or slightly confident’ in managing vaccine storage requirements (n=259; 37.1%) and providing immunisation advice to the woman regarding her and her infant's future immunisations (n=245; 35.1%). Respondents who reported previous experience in vaccinating adults and/or children were significantly associated with being confident in vaccination management (Table 1).
After completing the module, 94.7% (n=1128) reported that they were ‘confident’ or ‘very confident’ in conducting all aspects of vaccination management in pregnant women, while 4.8% (n=58) reported feeling ‘somewhat or slightly confident’ and 0.5% (n=4) reported that they did not feel confident at all. When asked to rank the components of the module, the majority of respondents scored all components in the top two ranks (4 and 5) (Table 2).
| Programme component | Ranking of programme components (1=lowest to 5=highest) n (%) | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Introduction and rationale for maternal vaccination | 7 (0.6) | 5 (0.4) | 60 (5.4) | 331 (27.8) | 787 (66.1) |
| Pre-vaccination assessment | 8 (0.6) | 11 (0.9) | 83 (6.9) | 364 (30.5) | 724 (60.8) |
| Managing vaccine storage and cold chain | 6 (0.5) | 5 (0.4) | 62 (5.2) | 324 (27.2) | 793 (66.6) |
| Administering vaccines to pregnant women | 7 (0.6) | 9 (0.7) | 71 (5.9) | 336 (23.2) | 767 (64.4) |
| Post-vaccination care | 7 (0.6) | 13 (1.1) | 68 (5.7) | 342 (28.8) | 760 (63.8) |
| Documentation related to the immunisation encounter | 11 (0.9) | 13 (1.1) | 111 (9.3) | 360 (30.2) | 695 (58.4) |
| Immunisation advice to mother regarding her and her infant's immunisations after birth | 10 (0.8) | 8 (0.6) | 75 (6.3) | 363 (30.5) | 734 61.6) |
A respondent's age was significantly associated with being employed in a birthing suite (χ2=22.612; P<0.001), but no associations were found between other employment locations and age. A respondent's confidence in vaccination management was not found to be significantly associated with their clinical role or age, and there were no significant associations found between a respondent's role and satisfaction with the components of the module.
Discussion
All seven components of the module were rated highly, which suggests it has been an effective intervention. In total, 57% of respondents reported feeling ‘very confident’ in all aspects of vaccination management before completing the module, compared to 94.7% after the module. This key finding suggests that the educational module was pitched appropriately to the needs of participants and will lead to consistent and effective vaccination implementation throughout NSW.
Provider recommendation is the most important factor in improving vaccine uptake in pregnant women (Healy, 2016). Vaccination rates during pregnancy have been reported to be low in Australian women (Webb et al, 2014), while a study in Belgium reported that 64% of women received a pertussis vaccine during pregnancy compared to 45% who received the influenza vaccine. The main reason for pregnant women not receiving pertussis or influenza vaccines was that they were not offered—or were even discouraged—by health professionals (Maertens et al, 2016b). In a cross-sectional survey of 815 pregnant women in Australia, most (80%) were willing to receive the pertussis vaccine if it was recommended by a health professional (Wiley et al, 2013b) and interim maternal pertussis vaccination rates have been reported at around 55% in Western Australia and 40-50% in Queensland (Beard, 2015).
The maternity information system in NSW, eMaternity, records meetings between pregnant women and health professionals, from the first antenatal visit through to their postnatal care. Data extracted from eMaternity for 12 facilities in three local health districts (Central Coast, Northern Sydney and Northern NSW) indicated that on average, 71% of pregnant women were vaccinated between 1 January to 30 April 2017. Although there are no pre-programme baseline data with which to compare this vaccine uptake rate, it is encouraging that almost three-quarters of pregnant women in NSW consented to pertussis vaccination, particularly in Northern NSW and Northern Sydney, which have been identified as having low childhood immunisation rates (National Health Performance Authority, 2014). As the roll-out of the eMaternity database progresses in NSW, data will be available for all districts from early to mid-2018 onwards.
In the pre-survey results, previous experience in vaccinating adults and children was found to be significantly associated with respondents' confidence in vaccination management. This is consistent with an Australian study, which found that, when providing postpartum pertussis booster vaccinations to women, midwives reported that the most important factor was their own perceived self-efficacy in conducting the appointment (Robbins et al, 2011). Although this educational module has shown to increase health professionals' confidence in conducting a vaccination appointment, there are a number of other obstacles that need to be considered to improve maternal vaccine uptake in any new vaccination programme. As part of the module, health professionals were provided with information on aspects that represented common questions for women, which included the effectiveness of antenatal pertussis vaccination; including international data on similar programmes; answering vaccine safety concerns; lack of information by the health professional; and lack of awareness of the severity of the disease on the woman and her unborn child (Blanchard-Rohner et al, 2012). Other obstacles for women that were not addressed by this module included fear of liability following an adverse event; the wish to reduce the number of interventions during pregnancy (Blanchard-Rohner and Siegrist, 2011); the pregnant woman's ethnicity and the level of education and parity (Maertens et al, 2016b). A survey of New Zealand mothers' attitudes towards immunisation (Petousis-Harris et al, 2002) implied that the quality and types of information offered by midwives could be improved; however a Canadian study (Tong et al, 2008) found that there was confusion among maternity care providers regarding whose responsibility it was to recommend and administer vaccinations. The pre- and post-surveys did not elicit any responses regarding confusion or delineation of roles; however, future educational modules should clarify roles and responsibilities in any new maternal vaccination programme, particularly where there are shared care arrangements or when a pregnant woman sees a different health professional at each visit (Webb et al, 2014).
Data showed that 37% of midwives employed in NSW Health public facilities completed the education module, a finding that can be expected, as it may not have been viewed as essential for midwives who were not employed in antenatal care areas. The training was, however, completed by staff employed in other clinical areas, such as birthing and postnatal wards, and not just antenatal units, which were the main target. This is a positive outcome as, in many public health facilities, maternity staff rotate through clinical areas, so staff in postnatal and birthing units who completed the module will have gained essential knowledge and skills in advance of their next antenatal clinic rotation.
Limitations
The educational module was only made available to staff employed in NSW Health public facilities and the pre- and post-surveys were only offered to this group. Although the overall response rates were high, they varied greatly within districts and may not be representative of the NSW Health workforce or maternity care providers in particular. The pre- and post-survey responses were not matched as they were completed anonymously. A pre-test/post-test design may have provided a more robust research approach to determine the direct effects of this educational intervention (Knapp, 2016).
Conclusion
This research provides evidence that a maternal pertussis vaccination educational module increased confidence among midwives and maternity staff in vaccination management for pregnant women and that all components of the module met their needs to support them to effectively and consistently conduct an immunisation appointment with a pregnant woman. Despite the high ranking of module components, it will be necessary to continually evaluate the training to ensure that it continues to meet the needs of future users. Additionally, although maternal pertussis vaccine uptake after the implementation of the educational module has been reported to average 71% in three districts in NSW, it needs to be much higher than this in order to protect vulnerable infants, and must be sustained for all future pregnancies. An informed and confident maternity workforce will maintain high vaccine uptake in pregnant women to ensure that pertussis vaccination is entrenched in routine antenatal care in NSW, to protect vulnerable infants in their first few weeks of life from life-threatening diseases such as pertussis and influenza.

