This is the second of two articles on crowdsourcing. In the first article (Frewin and Church 2019), crowdsourcing was introduced as an innovative way to find solutions to issues in practice. Defined as a process by which problems can be solved by using ideas sourced from a group of people (Howe, 2006), crowdsourcing can be used to discover rich and relatively low-cost ideas to improve the maternity experience.
The need for improvement in maternity services has been highlighted in national enquires (Kirkup, 2015) and is the subject of regular review by the Care Quality Commission (CQC). Although there is no single definition of quality improvement, there is a general agreement that ‘improving quality is about making healthcare safe, effective, patient-centred, timely, efficient and equitable’ (The Health Foundation, 2013:3). Quality improvement methods should be systematic and robust, and able to focus on evaluation, action and change. This article will focus on two principles of quality improvement: engaging staff, and involving service users and in solutions (Department of Health, 2008).
The role of the midwife
Midwives should be supported to see innovation and improvement as a core part of their role. Although all members of staff can be involved in improving the quality of services, midwives are uniquely placed to identify areas in need of improvement, through their relationships with women and their families. Change requires collaboration and buy-in from the multidisciplinary team; therefore, it is crucial that midwives develop management skills to lead innovation and quality improvement in practice (Jameson, 2012). All midwives have the power to influence and change maternity services.
Wenzel and Jabbal (2016) emphasised the significance of receiving feedback from those who experienced care in maternity services, meaning that the relationship between service users and midwives is crucial. They suggested that feedback was central to quality and that obtaining feedback was a way of monitoring the quality of care. Service user feedback can be provided both verbally and in writing, in forms such as Friends and Family comments (NHS England 2014), social media posts and feedback produced by bespoke workshops.
Coulter et al (2014:3) have suggested that:
‘It is unethical to ask patients to comment on their experiences if these comments are going to be ignored … A more concerted attempt is now required to make use of the evidence. An institutional focus could prove to be the key to getting it taken more seriously.’
However, Granville (2006) stated that designing services with patients was a way to use feedback to improve care, which should be encouraged across organisations. Later, Better Births (National Maternity Review, 2016) focused on the personalisation of care and choice, ensuring that midwives are invested in every woman's unique maternity journey. As a result, midwives are perfectly placed to influence care through quality improvement activities such as crowdsourcing. Establishing a multidisciplinary crowdsourcing workshop to explore experiences and share ideas is crucial to improving the quality of care and services.
The workshop
In March 2016, Kingston Hospital NHS Foundation Trust won funding from the NHS England Challenge Fund to improve services for women as part of a project known as ‘Nobody's Patient’. Through social media, the change platform #MatExp (short for ‘maternity experience’) felt compelled to highlight concerns voiced by three groups that were seldom heard in maternity services. These groups included:
Organisers of the project held a Whose Shoes? workshop (Box 1) to crowdsource new ideas to improve the care of women in these three groups. Scenarios based on women's experiences generated through #MatExp were used during the workshop. The crowdsourcing workshop was attended by a multidisciplinary audience, including service users and 10 midwives with knowledge and understanding of women's experiences.
Aim of service evaluation project
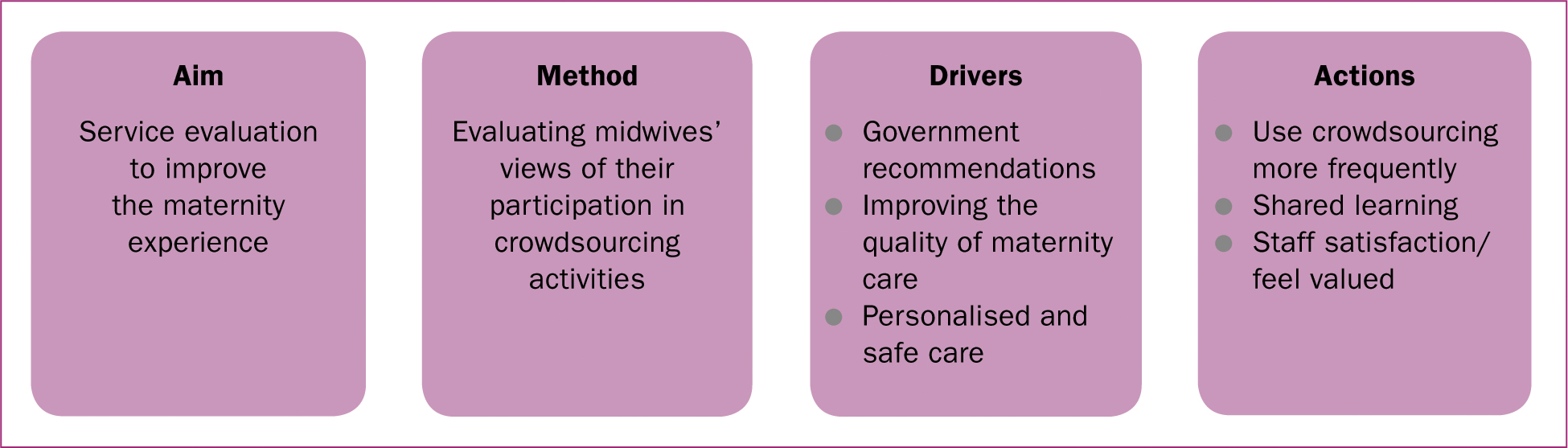
The service evaluation project focused on midwives who participated in the crowdsourcing workshop. The aim of this project was to:
It was important to discover how the midwife participants perceived their role in affecting change and the extent to which they felt they were successful in improving the quality of services (Figure 1).
Method
A service evaluation is a rigorous and systematic review of a service, and/or aspect of a service or care provided. The intention of this approach (as opposed to research) is to define care or activity, and to gather information as a means to inform decision-making (Gerrish and Mawson, 2005), rather than generating new knowledge, generalising findings, or measuring services against pre-existing standards such as in clinical audit. Although evaluations are limited to specific services, they provide information for service users and health professionals, and generate recommendations for improvement.
A generic qualitative approach (Cooper and Endacott, 2007) was used. This approach responds to experience-based questions relevant to a practice-based discipline such as midwifery (Kahlke, 2014). However, it is not guided by philosophical assumptions associated with known qualitative methodologies, such as phenomenology, grounded theory and ethnography, which focus on exploring in-depth experience, complexity of culture and theory building.
Two sub-categories of this generic method, qualitative descriptive approach (Bradshaw et al, 2017) and interpretive description (Thorne et al, 2004), are discussed in the literature. Caelli et al (2003: 4) define this generic approach as:
‘Those that exhibit some or all of the characteristics of qualitative endeavor but rather than focusing the study through the lens of a known methodology they seek to do one of two things: either they combine several methodologies or approaches, or claim no particular methodological viewpoint at all. Generally, the focus of the study is on understanding an experience or an event.’
It is argued that although generic approaches present an opportunity to develop new methodologies and new theoretical perspectives (Lim, 2011), they also offer researchers flexibility to explore questions from different perspectives (Kahlke, 2014). For this reason, a generic qualitative approach was considered appropriate to underpin this evaluation, since:
‘By and large, generic qualitative data collection seeks information from representative samples of people about real-world events and processes, or about their experiences. We want less to “go deep” and more to get a broad range of opinions, ideas, or reflections. Occasionally, a small, non-representative, but highly informed sample can provide rich information about the topic.’
However, concerns about the issue of rigour (Neergaard et al, 2009) focus on the absence of specific theoretical assumptions (where there may be incongruence between epistemological intent), the theoretical position of the researcher, and the methodological structure (Kahlke, 2014). Sandelowski (2010) suggested the need to apply theoretical frameworks that make sense in the context of the research questions and design, allowing the researcher to decide which theoretical perspective is the most appropriate. When illustrating the rigour of the decision-making process and research design, emphasis should be placed on the role of the researcher and their engagement with reflexivity, consideration of ethical issues and methodological challenges (Kahlke, 2014).
Ethics
Since this service evaluation was undertaken as part of a Master's degree, the project proposal was reviewed and approved by the School of Health and Social Care Ethics Committee at London South Bank University. Research governance approval was also granted from Kingston Hospital NHS Foundation Trust. Although ethical review for service evaluation projects is not considered necessary, (NHS Health Research Authority, 2013), there has been recent discussion about the ethics of conducting ‘research-like activities’ (Chen and Fawcett, 2017). For this reason, this project was carried out according to the principles of good ethical practice (NHS Health Research Authority, 2017). Written informed consent was acquired from all participants; maintaining confidentiality and protecting anonymity was paramount.
Sample
From the ten midwives who attended the ‘Nobody's Patient’ workshop, six were available and agreed to be interviewed as part of this service evaluation.
Data collection
Data were collected using face-to-face, semi-structured interviews (Parahoo, 2014) supported by the use of an interview guide. Participants' anonymity was enhanced by assigning each individual a number. All interviews were digitally recorded with consent.
Data analysis
Thematic analysis was used to uncover the descriptive phenomena within the interview process (Smith and Firth, 2011). Following the steps of Howitt and Cramer (2014), data were analysed by transcribing the material, coding the text and identifying themes that emerged. By transcribing the interviews verbatim, and re-reading the interviews, a deeper understanding and familiarisation of the data was achieved.
Findings
Four key themes emerged from analysing the data (Figure 2): improving communication, experience different perspectives, shared learning and positivity.
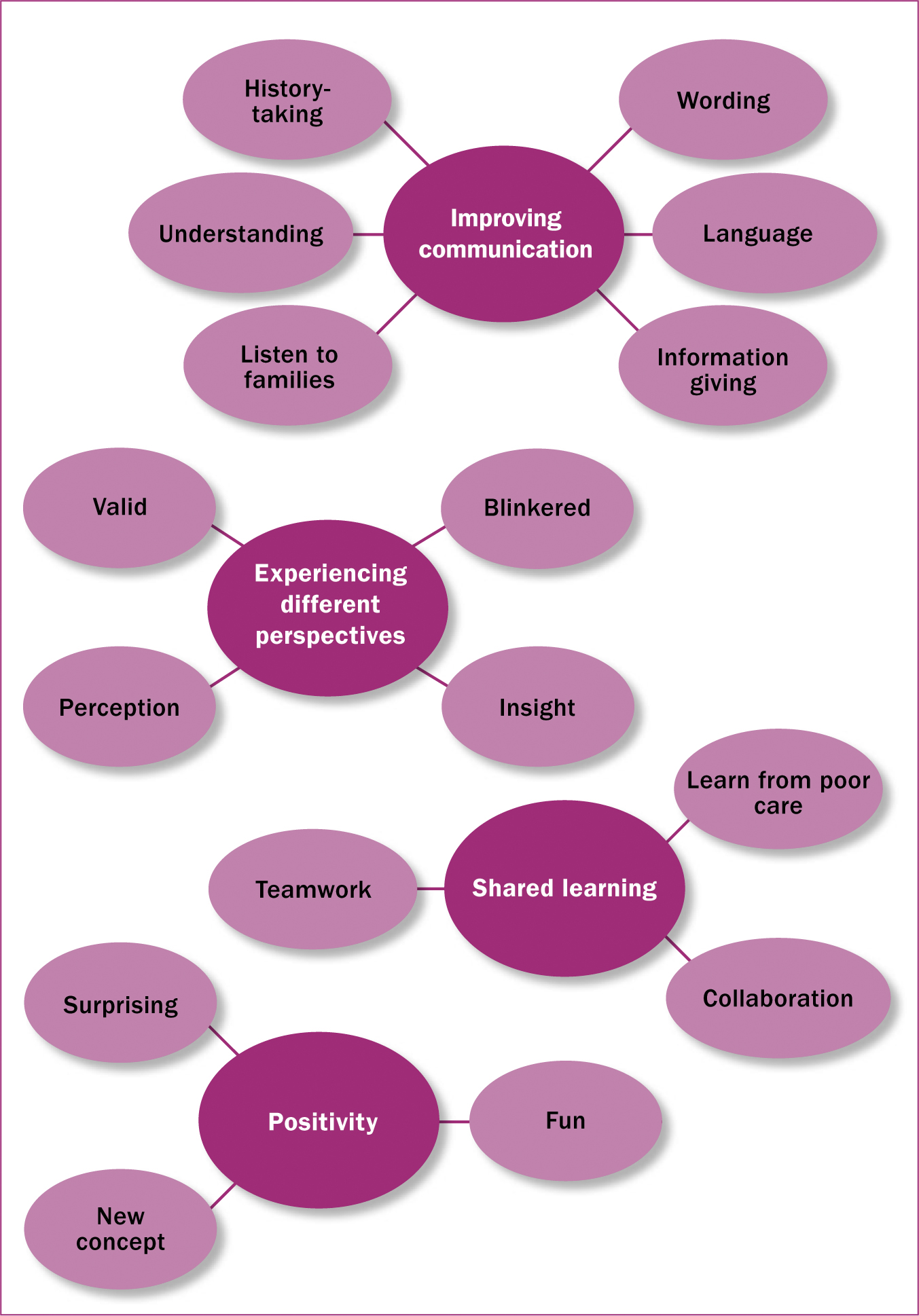
Improving communication
Participants agreed that communication was a major factor in achieving excellence in practice. During the interviews, midwives drew on personal experiences of poor communication to illustrate how communication had an effect on women's experiences of care and their relationship with health professionals.
One of the midwives reported that since she attended the workshop and participated in crowdsourcing, making simple changes in practice had resulted in a completely different relationship with service users, saying:
‘[Service users] want to tell us their side of the story … maybe we seem a bit more human or maybe it's just more approachable, it's definitely made a difference.’
Improvement in communication and language used in bereavement care was one specific area crowdsourced in the ‘Nobody's Patient’ workshop. Midwives expressed a need to learn which terms women experiencing bereavement might find more acceptable. As a result of participating in the crowdsourcing activity, one midwife reported learning a valuable lesson in communicating with families whose babies had died.
‘I've used the term “loss” quite a lot, I thought it sounded better than using “death.”’
She then drew on a specific example to illustrate how many bereaved mothers objected to official letters from the hospital referring to their baby as ‘lost’. One bereaved mother was reported to have said that her six babies were not ‘lost’ and that she ‘knew exactly where they were’, illustrating how language that may seem correct and sensitive may be inappropriate and upsetting.
Similarly another midwife reported how she was made aware of using acceptable and appropriate terms with bereaved families.
‘I'm very careful now with the language that I use, when dealing with a sad case.’
Crowdsourcing encouraged discussions about communication, and midwife participants stated that the workshop highlighted the importance of language. Women who experienced insensitive care after emotional and potentially traumatic events believed that health professionals could benefit from learning how best to care for women who are bereaved and/or critically unwell in pregnancy. Midwife participants emphasised how bringing together service users and health professionals was a valuable learning opportunity:
‘Getting people to sit down and speak and listen to somebody who has had a really bad outcome, or somebody used a poor choice of language or words.’
Another midwife, discussing her role in caring for women outside normal midwifery pathway, recognised the need for good communication, which could help women to feel that their choices were respected while maintaining safety as the number one priority.
‘Communication is key to improving services … we are going to do what people want in a safe way.’
Communication is often highlighted as a vital area of concern from the maternity service user perspective (Rowe et al, 2002; Prosser-Snelling, 2015). Women have reported greater satisfaction of care when they are given adequate information in a way that they understand (Fowler and Patterson, 2013). Both service users and health professionals have also reported that hierarchy between professional groups can act as a barrier to communication and innovation (Royal College of Obstetricians and Gynaecologists, 2015).
Experience different perspectives
The importance of sharing experiences from different perspectives was common across the interviews. Since the workshop was multidisciplinary and also included service users, participation in crowdsourcing enabled the discussion of issues from different points of view.
Some midwives felt that participating in the discussion had enabled them to review how they delivered care in their particular areas, saying:
‘It was nice to see and hear other people's thoughts and experiences.’
One midwife participant felt that crowdsourcing enabled her to share her concerns of how midwives on the ‘shop floor’ were viewed by management. The midwife felt that the multidisciplinary approach of crowdsourcing could help managers to appreciate the complexities of the midwife's role and the dedication and passion that midwives invested.
‘People that make big decisions sometimes aren't aware of what goes on at ground level and the pressures we are under.’
This midwife shared her thoughts on the relationship between the provision of care and the experience of care. Every pregnancy and birth experience is unique; therefore, care should be personalised and not prescriptive, and the midwife participants firmly believed this.
‘So, for me, it was important to gain people's perspectives of their level of care so that we could improve care as service providers.’
Shared learning
All midwife participants shared what they had learnt with their peers almost immediately.
‘After the workshop, I went back to the labour ward and discussed what we'd learnt with people who hadn't been at the workshop.’
Through the shared experiences of the service user, the ‘crowd’ was able to collectively suggest ways of improving specific aspects of care, so that issues in the provision of care could be addressed.
‘I shared some of the stories I had heard because they were really heartfelt and really important to share.’
One of the slogans used by #MatExp and Whose Shoes? is ‘no hierarchy, just people’. This emphasises how all people present at the workshop, regardless of their position in the Trust, had a maternity experience story. One midwife reported a general atmosphere of gratitude for the opportunity to share personal stories, which not only came from the service users, but also from health professionals, who had sad and emotive stories of their own maternity experiences.
‘It was good to be in a small group … so you share your ideas intimately … everyone was very welcoming and appreciative that you were there and sharing your views.’
Midwives admired the women who attended the workshop for sharing their stories so that others could learn. Midwives described the impact of listening to women's experiences face-to-face, and considered this more effective than crowdsourcing online. One said:
‘I tried to speak with the mums who had a bad outcome that had the courage to share their stories.’
Positivity
Four out of the six midwife participants rated crowdsourcing positively.
‘It was really sort of happy … a positive experience.’
Midwives enjoyed being included in pioneering a different approach to improving care, with the variety of attendees adding an extra dimension to the experience:
‘I just felt really proud to be involved … and we were using a different method … and all those different people involved.’
Midwives and other health professionals strive to ensure that women arrive at a mutually agreeable, personalised plan of care, using open discussions between the health disciplines (National Maternity Review, 2016; Coxon et al, 2017). As a service provider, the NHS has a duty not only to provide safe care, but a quantifiable service (Redshaw and Henderson, 2015). This was a daily challenge for participants, who nevertheless felt that making steps to ensure that women received personalised care was a positive experience.
Collating information
Developing and testing bespoke crowdsourced material at the ‘Nobody's Patient’ workshop resulted in many ideas to improve care for women and their families across the three groups (families with babies in the neonatal unit and in paediatric care; women who developed unexpected serious illness in pregnancy and the postnatal period; and women who had experienced a mid-trimester loss). The ideas from the workshop were written onto ‘pledge cards’ and followed up by the project midwife to put them into practice. These solutions (Box 2) could be replicated by other Trusts and have been discussed in detail elsewhere (NHS London Clinical Networks, 2017).
Implications of findings
Crowdsourcing is an innovative, simple, cost-effective and easily adaptable way of finding solutions to improve care (NHS London Clinical Networks, 2015). This study has shown that midwives were able to implement small changes and that by learning with colleagues through a crowdsourcing activity, midwives had a greater understanding of what women wanted from maternity services. This service evaluation highlighted the positive effects of crowdsourcing, for both midwives and service users. Midwife participants appreciated the shared knowledge of the crowd, whether service users or health professionals, and went on to share their learning with colleagues. Midwife participants felt that their input was valued, and appreciated the opportunity to improve care.
Recommendations for practice
Recommendations for policy
Recommendations for research
Further exploration of the views of members of the multidisciplinary team and more senior healthcare colleagues would add a another dimension to the analysis.
Conclusion
Crowdsourcing can be fun and creative. The findings of this service evaluation indicate that involving stakeholders as a ‘crowd’ to find solutions was successful and highly rewarding. Midwife participants took pride in sharing their ideas, especially when they were put into practice, and this ownership of ideas added an extra dimension to their role. Midwives realised that small, no-cost improvements were easily achievable, fun and acceptable to women and families.

