My first birth resulted in an unplanned caesarean section and it is my opinion that the lack of appropriate supervisory support contributed to the outcome. This article aims to outline how supervisory support can have a lasting impact on birthing outcomes, both negatively and positively. It is likely that the health of our nation is reliant on positive birthing and appropriate supervisory support plays an important role towards it.
Caesarean section is major abdominal surgery yet despite this, incidence is on the rise (Royal College of Obstetricians and Gynaecologists (RCOG), 2013). The morbidities associated with caesarean section make this birthing experience less than pleasant. The associated risks include (NHS, 2012; Baby Centre, 2014):
These short- to medium-term problems could have lasting adverse affects on the health of mother and baby in the long-term. Studies on this matter are hard to find, leaving the question wide open as to the long-term health effects of regular and over-used medical interventions on the birthing process.
In my experience, there is a stark different in the resulting birth outcome of one birth with proactive and positive supervisory support and one without. In 2013, I benefited from support by the Brighton and Sussex University Hospitals NHS Trust Supervisor of Midwives (SoM) for the birth of my second daughter. The lack of positive or proactive supervisory support for my first birth in 2009 provides insightful comparison and demonstrates the importance of the supervisory role to the user. Changes made since 2009 to the Brighton & Hove midwifery provision greatly improved the service and are to be commended for this. Proactive and positive supervisory support contributes to the health and wellbeing of mother and baby. Providing this insight into the user experience informs future services, ensuring the needs of mother and baby are central to service improvements.
Implications of supervisory support
From a user perspective, supervisory support can and should play a significant role in assisting a positive birthing experience. A lack of support will have the opposite effect and may contribute to a ‘cascade of intervention’ (Figure 1) that could result in a caesarean birth and associated problems for mother and baby. The cascade of intervention chart visually outlines medical protocol and procedure intervening in the natural birthing process with the resulting outcomes. There are many versions of this chart from a range of sources, based on a wide collection of research.
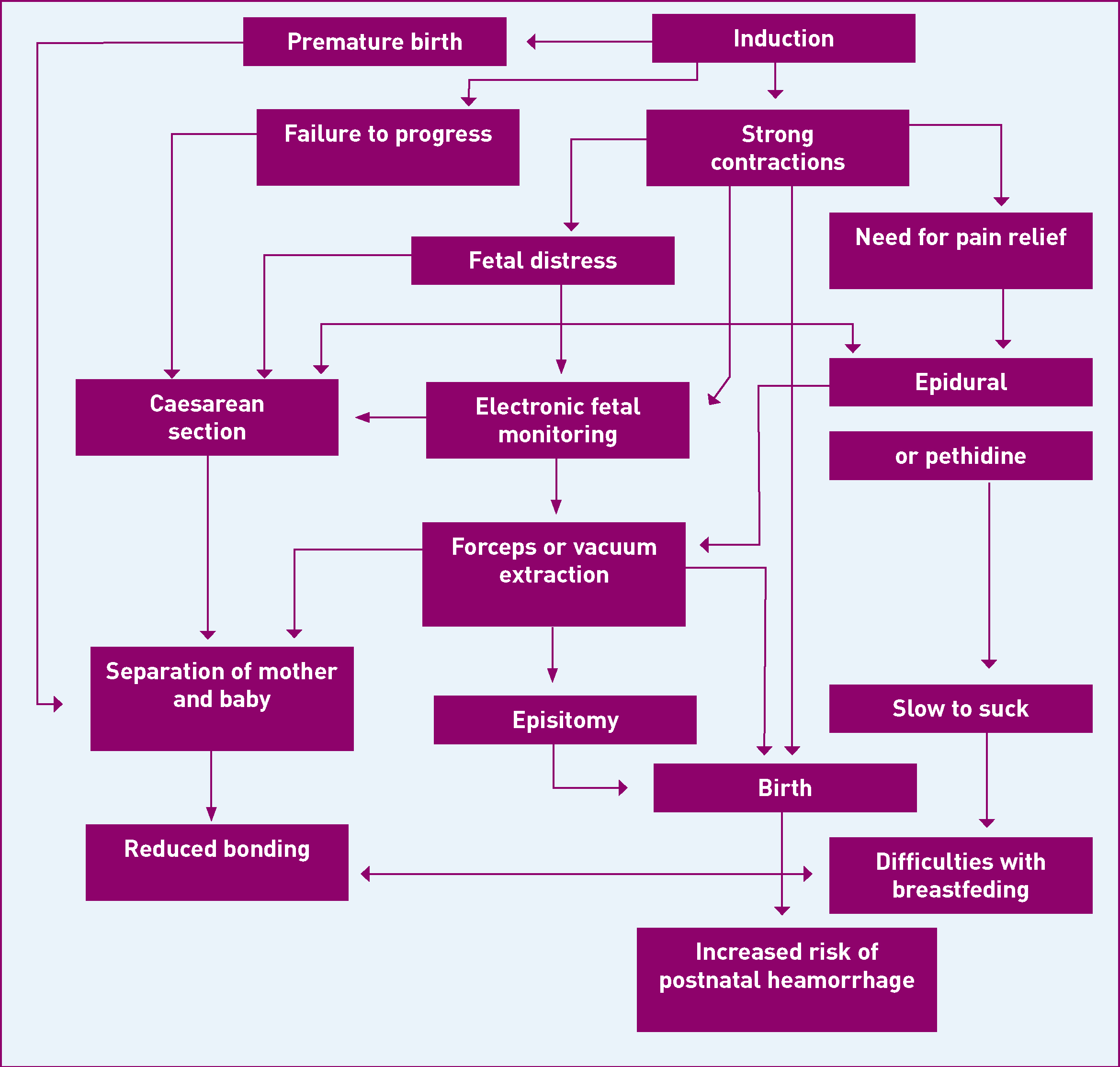
The National Childbirth Trust (NCT) states: ‘It is hypothesised that the use of routine medical interventions early in labour can lead to the need for further interventions that tend to be increasingly invasive’ (NCT, 2009). Every SoM needs to understand the gravitas of the role and its implications for the health and wellbeing of a mother and her baby.
My first birthing experience lacked positive or proactive support; the outcome of the birth was a caesarean section. My second birthing experience received both positive and proactive support; the outcome was a natural vaginal birth after caesarean (VBAC) home water birth. For me the supervisory support received in both birthing experiences contributed to each outcome.
The potential implications on the birthing outcome without supervisory support
My first birth was not what I wanted. I wanted a home birth; I had a caesarean section. Major abdominal surgery is not something I would elect for, it had lasting adverse affects for me mentally and physically. The supervisory support I received during pregnancy and at the point of going into labour was vastly lacking. I hoped for support from the professionals and carers to help me succeed in my first birth, instead my personal preferences went unsupported and gave me doubt in my ability to birth.
During the first stage of my labour, the SoM failed me, my baby and my husband. Initially when labour started, my choice to birth at home was refused because of training and staff shortages. Simon, my husband had to site law before a midwife was sent out to us: this shouldn't have been needed, for better or worse I was adamant I wanted a home birth. My preference needed to be treated with care and compassion with my views respected—I didn't receive this. I sensed that the attending midwife wasn't a willing participant. For us the cascade of intervention began when the SoM chose to decline us the support we needed.
I've been to the Birth Stories Service since the birth of my first child. Birth Stories explained the hospital's perspective of why I had a caesarean section, it was because my daughter was forehead presenting and got wedged on the pelvic bone. I have my own theories about this being the cause that made a caesarean section inevitable. Babies can, and are, born breech naturally, meaning position is not necessarily a conclusion requiring medical intervention. With the right knowledge and technique, babies can be moved back up the birth canal temporarily to encourage a required shift in position (breech or otherwise). My perception of birth was not a very positive one. I was brought up with my mother's horror story from her first birth, my brother, giving an unfavorable imprint of the birthing experience. The physiological impact of being in an environment I did not want to be in had a profound effect on my belief of whether I could birth, I gave in to what felt inevitable, I stopped trying. For me the barriers to birthing naturally were on the whole psychological, rather than physical. The events that took place during pregnancy and labour were compounded by the lack of supervisory support—the final straw.
The implications on birthing experience with supervisory support
My second birth was very close to my ideal birth: I had a natural home water birth, without any chemical input or intervention. The SoM supported my choice, apprehensively because of being VBAC at home, yet still supported it and that made a big difference to me. I received informative contact from the supervisory prior to going into labour.
The letter was formal and factual, which was hard to digest in my third trimester. It warned against VBAC at home, outlining the risks, highlighting the recommendations such a hospital birth, stating hospital protocol. I felt a little put out by the letter to begin with, even slightly angry: I was being provoked to deal with such formal and concerning matters in my third trimester when I needed to feel happy and secure and supported to develop the appropriate oxytocin levels to birth.
Once I put the contact into perspective by speaking to supportive professional such as my doula, the contact was appreciated because it acted as trigger for me to resolve issues left open from my previous birth experience. I researched popular risk concerns: VBAC, meconium in the water, VBAC at home and other related matters. I wrote back thanking the SoM for the letter, cited my own research with references and concluded that I was confident to birth at home. It did just that, obscurely it gave me confidence. The information helped me strengthen my belief that I could VBAC at home safely. And I did.
I had to accept the risks and make clear to the midwifery team that I did, verbally during meetings and in my medical notes. Once I did, those supporting me relaxed and everything went much smoother. I was able to birth my way and felt supported by the midwifery team.
The future of supervisory support
Being pregnant was a really emotional time for me. I needed to feel supported. Without family to turn to, I looked elsewhere for that support—the health professionals. After speaking to other mums in the area about their birthing experiences, many are in a similar situation without local family. There is a need and a big responsibility for appropriate maternal support from medical professionals. The service received by users leaves a lasting impression. It is vital to give a service that meets with expectations and supports choice.
What is needed from supervisory support today and tomorrow
Support from the SoM is beneficial and fundamental for positive birth experiences. The service needs to: be pro-choice, in that women can birth as they wish; informed about boundaries, restrictions and protocols to aid women's birthing decisions at an appropriate time to facilitate and not hinder the birthing process; enabling women to take control of their birth experience. Positive and proactive supervisory support is essential to the health and wellbeing of every mother and baby.
Conclusions
The challenge for SoMs is to provide a nurturing and caring support service for users, while managing insurance and legal risks bound by Trust protocol. It may be possible to meet the challenge by changing the way and timing of when users need to be informed of midwifery obligations and restrictions created from risk assessment. Whether this is the answer to remains open to debate.
For me, supervisory support is the tip of the iceberg relating to issues around positive birthing. The matter of supervisory support highlighted for me a far more pressing and serious matter: the long-term health implications from the cascade of intervention and that ‘normal birth’ is a very achievable physiological process.
This matter requires an innovative and pioneering Trust to take a stand, to research the long-term implications of medical intervention in the birthing process verses natural birthing, and maximising the potential for positive birthing with appropriate protocol—not laden with fear that comes from legal and insurance risk. The benefits could be: a reduction in costs associated with problems arising from medical intervention, a reduction in long term health costs to the NHS, a reduction in Trust insurance costs, as well as improved physical and mental health for mother and baby.

