The fundamental purpose of the statutory supervision of midwives has always been to protect the public. This is achieved in myriad of ways including; interfacing with an organisation's clinical governance processes, leading on initiatives for improving practice, promoting normal birth, delivering education, professional advice and guidance, developing and supporting midwives, and working with the women and families who use services as advocates, supporters and guides. The strength of the success of this work is often perceived to arise from supervision being objective and detached from any one organisation (Bacon, 2011). This allows the focus to remain on the promotion of excellence in midwifery practice and standards of care, without the representation or promotion of any vested interests other than the standards lain down by the Nursing and Midwifery Council (NMC) such as in the Midwives rules and standards (2012) and Standards for the preparation of supervisors of midwives (2014a). Such independence arises because the line of accountability of the supervisor runs to their Regional Local Supervising Authority (LSA) and not to the employer for supervisory matters (Box 1).
Questioning supervision
In recent months there have been significant challenges to the framework for supervision, and more could arise from both the planned NMC review of the framework of midwifery regulation and the recent Law Commission review of the regulation of health professionals (Law Commission, 2014) that may alter the statutory framework for midwifery and supervision.
The planned NMC review follows the Parliamentary Health Service Ombudsman (PHSO) questioning how the function of supervision is exercised in the wake of the tragic events in Morecombe bay (PHSO, 2013). The key concerns of whether investigations into fitness to practise should be carried out at ‘arms length’ from the NMC and whether the current arrangements allow for sufficient objectivity to produce robust outcomes, are core business for SoMs, therefore is appropriate that they should be examined carefully. Certainly the LSAMO UK forum has recognised some of the potential pitfalls within supervisory processes producing much guidance and support to address these, as well as the provision by individual LSAs of increasing amounts of training and development opportunities for SoMs in line with the Midwives rules and standards (NMC, 2012). However, although the LSAMO strategic direction is clear about the standards that it expects from supervisors, there is less detail on how the goal of ‘enabling supervisors to develop and build their competence’ (LSAMO forum, 2012) will be achieved.
Listening in
Developing relevant training and guidance and support structures involves the need to understand what the key issues in supervision are from the perspective of the contemporary supervisor. Maternity services are facing continual scrutiny and concern from all quarters (National Audit Office (NAO), 2013; Care Quality Commission (CQC), 2013; House of Commons, 2014); consequently, the expectations and demands made of supervisors are considerable.
There is little known of what supervisors specific needs may be for them to fulfil their role, but the significant challenges they continue to face in fulfilling their role are well documented (Henshaw et al, 2011; Rogers and Yearley, 2013) with each LSA having specific issues that influence the exercise of the statutory function.
London's unique challenges are driven by the combination of it's relatively tiny geography and vast and varied demographics. Despite being the geographically smallest of all the regions, in terms of births, midwives, and women, it is the largest and most complex. Nineteen percent of all the UK's births are in London, overseen by 5500 midwives who in turn are supported by 360 SoMs. The women who give birth in London are diverse, with only New York having a greater diversity in terms of ethnic mix; and more women over 40 giving birth in London than anywhere else in the UK (Read, 2013). This caseload means that working in London entails meeting a huge range of health and social needs. Supervisors, who fulfil the role in addition to their substantive posts, therefore have to work extremely hard to ensure the highest standards of midwifery care are pursued at all times.
In the face of such complexity it became increasingly important for London LSA to understand whether it was meeting the needs of its supervisors, monitor whether supervisors had sufficient resources to fulfil their role (NMC, 2012), and what future direction the strategic development of supervisory support should take to ensure high quality statutory supervision was enabled in London. This exercise also would also allow evaluation of the recently introduced London LSA link midwife role, which had been devised in order to better support Supervision in the Capital (Box 2).
Methodology
In view of the large population of SoMs in London, the decision was made to undertake an anonymous survey using an online tool. The 26 questions used were devised to gain insight into the views of SoMs on the statutory functions of the LSA, resources available to SoMs, the education and development provided and the quality of support, advice and guidance experienced. The survey was designed to elicit both quantitative and qualitative data with mostly closed questions used but the opportunity to add commentary on any response.
The LSA database was used to give a current list of all practising SoMs in London, which totalled 360. An online link was sent to all SoMs and several reminders followed over the next 4 weeks using a variety of sources. Data analysis of quantitative data were achieved using the software provided by the online survey tool. The qualitative data were reviewed for each question to understand the key themes raised.
Results
Of the 360 surveys sent, 263 SoMs responded, giving a response rate of 73%. It was noted in the analysis that not all respondents answered all questions. The key findings are discussed here and all findings are available in the main report (Brintworth and Read, 2013).
Support and communication
Overall, SoMs rated the support they received from the LSA highly. Eighty nine percent of respondents rated the helpfulness of their interaction with the LSA as helpful or very helpful and 97% of SoMs knew who their link supervisor was and the majority liked the role and rated it highly The role of the link midwife was described as positive, helpful, and supportive and the majority of comments given expressed a desire for more time to be available from this role for general access to support, attendance at supervisory team meetings, support with investigations and having a higher profile in the provider unit.
‘Keep doing what you are doing; it works in that I feel supported and passionate about supervision’
There were few negative comments given and these were centred on wanting more support, a faster response to enquiries and getting consistency of response from different members of the LSA.
‘Is there enough LSA support for London as there are so many Trusts?’
Communication was highly valued with all the differing types (face-to-face and telephone contact, the website, newsletters, and annual report) well used and an enthusiasm for further development of these resources, especially about key LSA events and guidelines. When asked about how communication strategies might evolve, there was a clear desire for more face to face advice and guidance in the form of support groups and advice surgeries and with recruitment. Interestingly, there was little appetite for engaging with social media such as Twitter and Facebook.
Continuing professinal development
SoMs reported that over half had attended LSA training events in the previous year and a number had attended multiple events. When asked to elaborate about what further educational opportunities would support their role, 33% of comments related to investigation of fitness to practise. There was no other single area in the whole of the survey that was highlighted as being of such concern, and this links with the findings about LSA support that also highlighted this as an area of need for supervisors.
When asked about how the LSA could help teams in future, the biggest category of response from the comments made was in continuance and extension of the support offered by the link midwives and their attendance at team and sector meetings. This was followed by help with team building and once again fitness to practise matters.
Fitness to practise
To understand further the issues concerning SoMs with the conducting of investigations into fitness to practise, they were asked whether they felt that they had sufficient support, and if not, what areas could have been better supported. Overall, 30% of SoMs felt that they would have liked more support in general with their investigation, and that categories of specific concern were report writing and in the making of recommendations.
A further area highlighted was in the management of the investigation process. Fifty-four percent of SoMs reported that difficulties with the completion of investigations related to midwives being on leave once concerns were identified, and 45% found consequent difficulties in then arranging to meet and interview the midwife. Time to conduct the investigation was quoted as an additional problem. More than one third of respondents cited that if they undertook an investigation their substantive post would not be supported for the time they were involved in the investigation, as they were either in management or specialist roles. This may be a contributory factor to the finding that 1 in 5 supervisors stated that they found the report hard to write.
Time for supervision
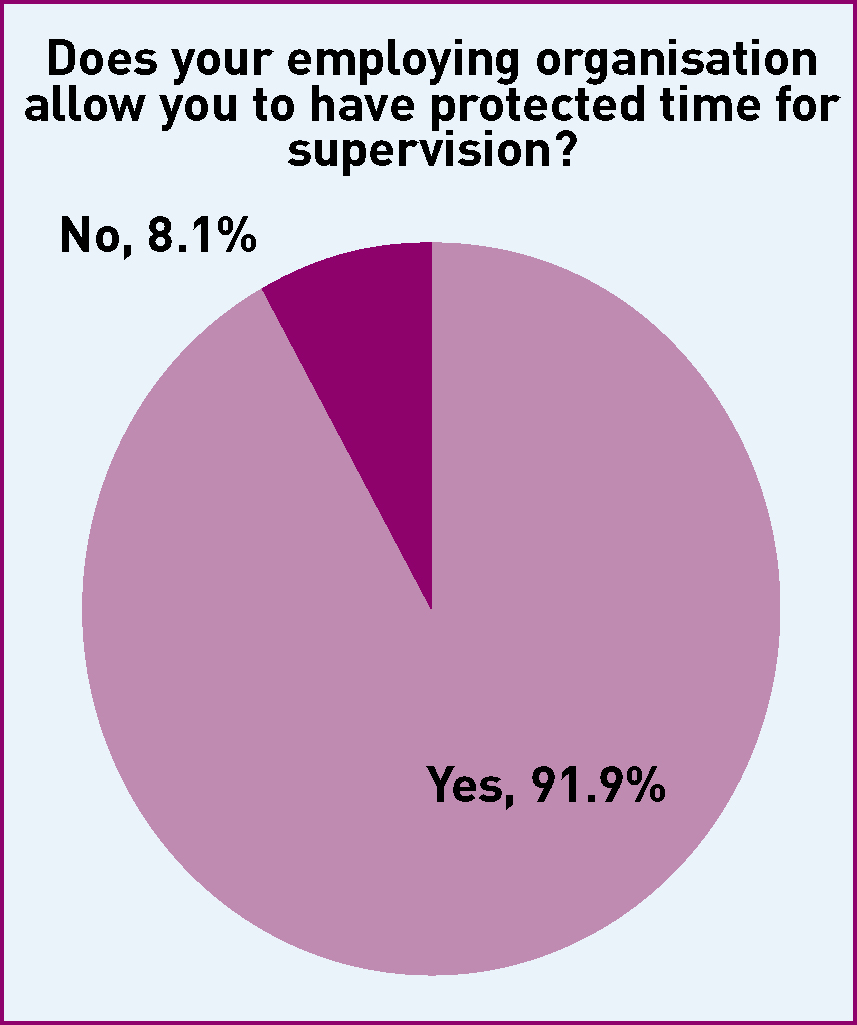
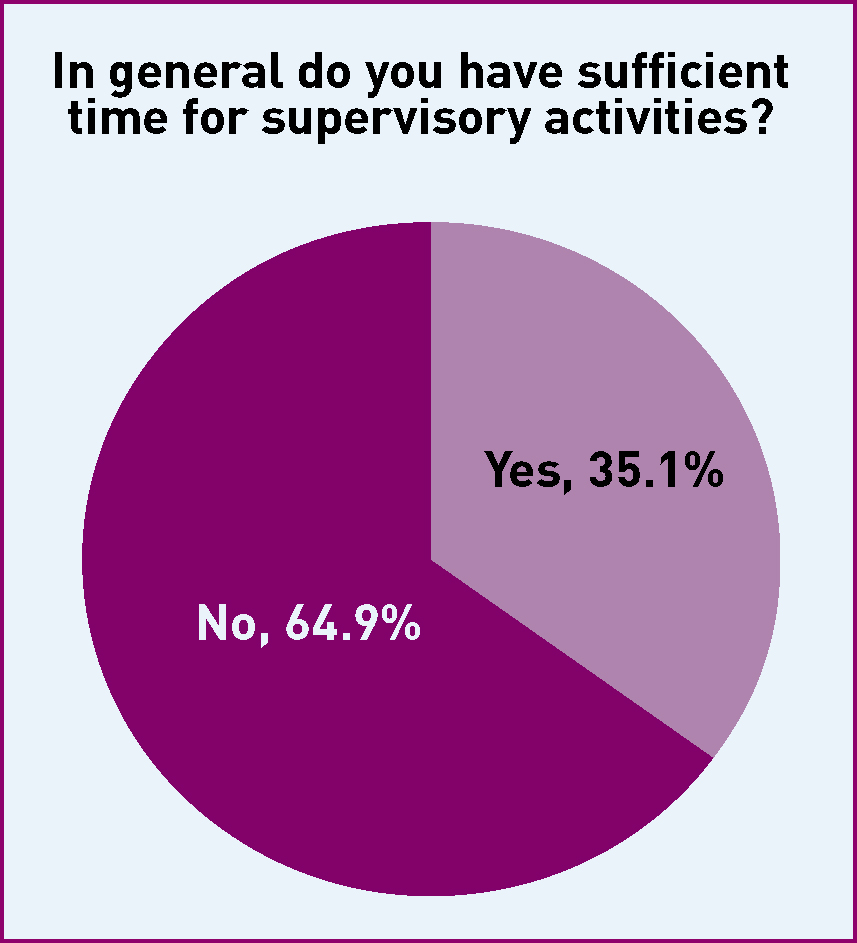
To understand the context in which SoMs practice, there was exploration of the time available to them to carry out the function. This revealed an interesting dilemma. While 92% said that their employing organisation allowed for protected time for supervision, only 35% felt that they had sufficient time to carry out the role (Figures 1 and 2).
As with investigations, the most common difficulty faced by SoMs with time management was that their role was not back filled when they devoted time to supervisory duties, with 52% of SoMs describing this difficulty, and a further 41% of responses cited lack of administrative support. Only 1 in 5 SoMS found no problem in taking the time needed, with just over 1 in 5 reporting that they were asked to work clinically when they were supposed to be focussed on supervisory issues. This pressure on the role led to some SoMs describing quite considerable stress:
‘I for one am feeling very despondent and regularly questioning if I wish to remain in a role that I do not feel I am doing justice to’
Discussion
This survey of SoMs in London was responded to by nearly three quarters of all practising SoMs in the capital, which offers a significant degree of confidence in the results. The over-arching finding was that SoMs demonstrated great commitment to their role, a desire to engage and learn more about supervision, improve the function and engage positively with London LSA.
The primary way in which they reported the desire to develop their skills was through personal interaction and face-to-face support, and training and development primarily through the LSA link midwife role. Meeting SoMs support needs has long been recognised as important to maintaining the quality of supervisory functions, not least because in the absence of this being achieved it is questionable what levels of support can be available to midwives from the supervisors themselves (Stapleton and Kirkham, 2000). This is critical, as the effects of poor supervisory processes can be damaging and long lasting for both midwives (Demilew, 1996; Stapleton et al, 2000; Henshaw et al, 2011) and crucially women and their families (CQC, 2011; NMC, 2011).
The LSAMO role has partly evolved in to a source of support for SoMs (Duerden, 2000; Bacon, 2011) but it is questionable how much can be achieved by any one individual LSAMO. Part of the LSAs obligations involves ensuring that they ‘provide sufficient resources to enable a local supervising authority officer to discharge the statutory supervisory function’ (NMC, 2012: 10). Currently, considerable variation exists as to how resources are distributed to LSAMOs; the London region has one LSAMO and two support midwives whereas the North, Midlands, South regions each have three LSAMOs and a variety of LSA support midwives. Such variation has been recognised as creating a risk of inequity and lack of consistency in the function (Richards, 2012). Consequently, at the time of writing, a review of the structures and resources of all English LSAs is underway, and it will be important for that review to recognise the potential impact of the support LSAs provide to supervisors.
The area of support that SoMs indicated that they had the most need in was investigations into fitness to practise, which was referenced in multiple areas of the survey. Investigations represent one of the most significant ways that supervision contributes to the clinical governance agenda and protection of the public with the standards required being detailed and clear (NMC, 2012; LSAMO forum, 2013). There is considerable debate, however, as to whether these standards are actually being achieved in all cases (PHSO, 2013; NMC, 2014b) and midwifery commentators have discussed the destructive potential of this function being exercised poorly for both midwives and woman (Lewis, 2011; McHugh et al, 2013).
There was no sense from the results that SoMs did not recognise the importance of this aspect of their role, rather what emerged was that SoMs took fitness to practise matters very seriously and wished to improve their skills and outcomes, a recognised way of improving consistency (NMC, 2014b). They did, however, detail a number of significant challenges to managing the process, which despite concerns raised were not focused on matters of objectivity but on finding the time to undertake the investigation.
The conduct of a thorough investigation takes a considerable amount of time (NMC, 2014b). Although the amount of time varies according to the complexity of the case, it has been estimated by one LSAMO to take around 60–80 hours (Kirby, 2013, personal communication). The average SoM is generally allowed 1 day per month to attend to supervisory matters (Rogers and Yearley, 2013) and so immediately here the mismatch between demand and resource becomes apparent.
Time is an acknowledged and long standing source of tension in supervision (Halksworth et al, 2000; NMC, 2014b) especially when it has been estimated that the real time required to be spent on supervision as a whole is estimated to be 1 day per week (Mead and Kirby, 2006). Supervisors in London repeatedly said that they have insufficient time for their role, spending considerable amounts of their own time fulfilling the function, particularly in conducting investigations. Many also made reference to the lack of ‘back fill’ for their role if they were a manager or specialist midwife. Such substantive posts will inevitably be more difficult to support and add a further hue to the long running debate around managers being SoMs (Stapleton and Kirkham, 2000; Henshaw et al, 2011; Rogers and Yearley, 2013).
The manager/supervisor debate has mainly been framed by the risk of blurring boundaries, over punitive approaches and insufficient challenge by supervision to the employing organisation. The requirement to challenge the employer around systemic influence on safe practice is shared with those working in the risk and clinical governance frameworks of any organisation, but has been highlighted most recently primarily as an issue in supervision. This work suggests that that is not the issue SoMs perceive to be the most difficult issue but that the issue of lack of resources and concomitant burden to working and personal lives is more complex and influential on the quality of supervisory function.
Reliance on what appears to be good will for the exercise of a statutory function that contributes to most organisations clinical governance agenda in multiple ways is undesirable and of significant concern to all of those involved in supervision. The annual audits that LSAs undertake demonstrate that supervisors often fulfil their role to a high standard with innovation and energy (Read, 2013). It is questionable how reliable and sustainable this will be as pressure increases in maternity services and the SoM continues to struggle to fit supervision into an already busy working life; with questions being asked what impact on the quality of the function this has.
One impact that this continual pressure has produced is in the area of recruitment of new supervisors. This was rated as a significant concern in the review and risk assessment of the LSAs (NMC, 2013; NMC, 2014b). The current suggested ratio of one supervisor to every 15 midwives is not one that has a basis in research but is generally used as a proxy indicator for sufficient supervisory presence and resources in any organisation. In Rogers and Yearly's 2013 national survey of contact supervisors, only 48% reported their organisation met that ratio. Reasons cited by participants for difficulties with recruitment were; the demands of the substantive post, balancing home life, and being on-call. This echoes the finding of a small survey of midwives in one sector of London who were identified as potential supervisors. All cited time for the role on both their substantive post and personal lives as a major deterrent to undertaking the role (Read, 2013).
One other way in which this is affecting ratios from the perspective of appointed SoMs is that increasingly they are choosing to opt for periods of leave from Supervision (NMC, 2014b). London LSA had more SoMs make this request last year than in any previous year (Read, 2013), and reasons cited include the challenge of finding time to meet conflicting demands, and the inability to do justice to the supervisory role.
An innovative way that has been taken to meet these challenges head on is in the post of the full time SoMs. This was introduced in London in 2012 (Nipper and Roseghini, 2014) and involves an organisation paying a midwife to work full time in supervision. What has been apparent from early indications is that the quality of the function of supervision is significantly enhanced when this approach is taken, (Read, 2014). Supervisors in one organisation have described this innovation as hugely beneficial to supporting the quality of the work they undertake so improving services safety and particularly patient experience (Nipper and Roseghini, 2014; NMC, 2014b). This approach is being taken further in Wales with their complete re-organisation of supervision so that only full time supervisors are appointed (Richards, 2014).
Conclusion
‘The Committee notes that statutory SoMs is a tried and trusted means of assuring the quality of midwifery practice’ (House of Commons, 2011: 11). In order for supervision to continue to hold this reputation and continue to move away from that engendered in the PHSO report (2013) there needs to be a clear assessment of the structures of support required for supervisors of midwives. This report has shown that they value their role and personal support from the LSA to fulfil it. Equally, they have significant anxieties about the resources available to them to fulfil the role, and the impact that has on the safety of women and their families when they are insufficient. There is some evidence that innovations such as LSA support midwives and full time supervisor roles may well support best practice, and, in common with many areas in supervision this would benefit from further research. Therefore, the commissioned NMC review becomes extremely timely to ask the difficult questions about what supervision should look like in the future to promote the best in midwifery practice.

