The safest mode of birth for a breech-presenting fetus has been a topic for debate among researchers and clinicians for decades (Walker, 2012; Evans, 2013; Odent, 2013; Homer et al, 2015). Women with a cephalic fetus at term, in the absence of contraindications, are encouraged to have a vaginal birth, yet women with a breech-presenting fetus routinely undergo a caesarean section, even if their pregnancy has been otherwise uncomplicated (Banks, 1999).
The debate seemed to culminate with publication of the Term Breech Trial (Hannah et al, 2000), which concluded, after a randomised controlled trial, that caesarean section was the optimal mode of birth when compared to vaginal breech birth. This was suggested because of an increased risk of serious morbidity and mortality to infants born vaginally and, as a result, management of breech birth changed worldwide (Kotaska, 2011; Lawson, 2012; Odent, 2013; Sanders and Steele, 2014; Vlemmix et al, 2014).
Despite criticism of its validity (Goffinet et al, 2006; Lawson, 2012; Walker, 2012; Dresner-Barnes and Bodle, 2014; Vlemmix et al, 2014), the caesarean section rates in some settings escalated from 50 to 80% within 3 months of publication of the Term Breech Trial (van Roosmalen and Meguid, 2014). Table 1 demonstrates the varying rate of caesarean section for breech presentation between countries.
| Country | Rate of caesarean section for breech presentation (%) |
|---|---|
| Australia | 87.0 |
| China | 83.1–98.7 |
| Denmark | 88.6 |
| England and Wales | 88.0 |
| France | 75.2 |
| Italy | 93.3 |
| Malta | 96.1 |
| The Netherlands | 76.1 |
| Norway | 69.0 |
| Scotland | 100.0 |
| Switzerland | 95.4 |
Sources: National Collaborating Centre for Women's and Children's Health (2011); Australian Institute of Health and Welfare (2016); Cui et al (2016); Macfarlane et al (2016)
Concerns regarding the Term Breech Trial included the lack of a standardised measure of clinician competence. There is a known correlation between the safety of vaginal breech birth and the attending clinician's level of breech birth experience and confidence (Walker, 2012). The authors' definition of an experienced clinician was concerning:
‘A clinician who judged him or herself to be skilled at vaginal breech delivery, as confirmed by the head of department … or simply as a licensed obstetrician.’
As experience was self-determined, with or without endorsement from the head of department, there is great concern regarding actual levels of experience and competence of the clinicians attending vaginal breech births during the Term Breech Trial. A clinician having been involved in one vaginal breech birth has, comparatively, more experience than a clinician who has had no involvement in a vaginal breech birth; but it does not necessarily mean that they are competent in the skills needed to facilitate vaginal breech birth should complications occur.
The authors also violated the inclusion/exclusion criteria by including women whose babies were believed to have died before randomisation, or to have had a known abnormality, and women with multiple pregnancies (Hannah et al, 2000). Of the 16 neonatal deaths and stillbirths reported, more than 43% weighed ≤2500g (Pairman et al, 2014) and comments such as ‘difficult vaginal birth’ and ‘respiratory problems' (Hannah et al, 2000: 1379) were given as supporting information in regards to their deaths. This raises the question as to what constituted a ‘difficult vaginal birth’ and ‘respiratory problems’ (Hannah et al, 2000: 1379). It is unknown if the birth was difficult based on fetal heart rate abnormalities such as bradycardia; if the labour was obstructed; or the manoeuvres known to facilitate progress were unsuccessful. Low birth weight is often attributed to complications of pregnancy that cause poor placental function or perfusion, such as pre-eclampsia (Pairman et al, 2014), which may impact a fetus' ability to cope with the stressors of labour; the implication being these fetuses likely had a reduced capacity to compensate (i.e. maintain homeostasis) with the stressors of labour and birth due to an underlying condition, rather than mode of birth being the direct cause of their death.
Whyte et al (2004) conducted a 2-year follow-up study, and found no significant difference in long-term developmental outcomes, irrespective of birth mode; however, the researchers maintained that caesarean section was safer. The consequence of caesarean section persisting as the preferred mode of birth is the de-skilling of practitioners (Hunter, 2014), leading to a limitation of birth choice for women in most settings. Attempting to turn a breech into a cephalic position is one option.
External cephalic version
In mainstream maternity care, external cephalic version (ECV) is the most accepted method of turning a breech baby (Lewis, 2012; Pairman et al, 2014). It involves the use of a tocolytic and the physical manipulation of the fetus into a cephalic presentation (Walker, 2014), a method that has been subjected to rigorous scientific examination and has been shown to reduce the rate of caesarean section without substantially impacting on perinatal morbidity and mortality (Menakaya and Trivedi, 2013; Hutton et al, 2015). A small study by Kathpalia et al (2012) stated that ECV was a safe option when performed by an experienced clinician on women at term with no contraindications, and with the use of a tocolytic, ultrasound and cardiotocography (CTG).
A Cochrane systematic review (Hutton et al, 2015) reported that ECV performed between 34-36 weeks gestation significantly increased the incidence of a cephalic presentation at birth. ECV is recommended from 36 or more weeks gestation in green-top guidelines (Impey et al, 2017) and by the National Institute for Health and Care Excellence (NICE) (2017) because as few as 3% of babies revert to breech presentation after a successful ECV at this time. ECV conducted before 36 weeks considerably increases the risk of preterm birth (Hutton et al, 2015), although gestation does not seem to affect the success of the procedure (Kok et al, 2008). Nevertheless, compared to no intervention, ECV decreased the chance of a non-cephalic presentation at birth (Hutton et al, 2015). A total of five trials were examined, consisting of 2187 women across more than 20 countries. Only two of the published trials had been conducted in the last 10 years.
While being accepted as a safe practice, ECV is not without risk (Walker, 2014). Vaginal bleeding, placental abruption (Acosta, 2012), cord complications (entanglement), rupture of membranes (Kathpalia et al, 2012), fetal bradycardia necessitating caesarean section (Hyde et al, 2012), and fetal death are rare but associated risks with this procedure. These risks make ECV an unacceptable option for some women (Do et al, 2011). A retrospective population study (Bin et al, 2017) reported that, of 32 321 women with a single breech fetus at term, only 10.5% of women underwent an ECV over a 12-year period. It was not conclusive whether this was due to the procedure's unacceptability or an issue with service provision (Bin et al, 2017). Regardless of the reason for the low uptake of ECV, it demonstrates a need for alternative options.
Moxibustion and acupuncture
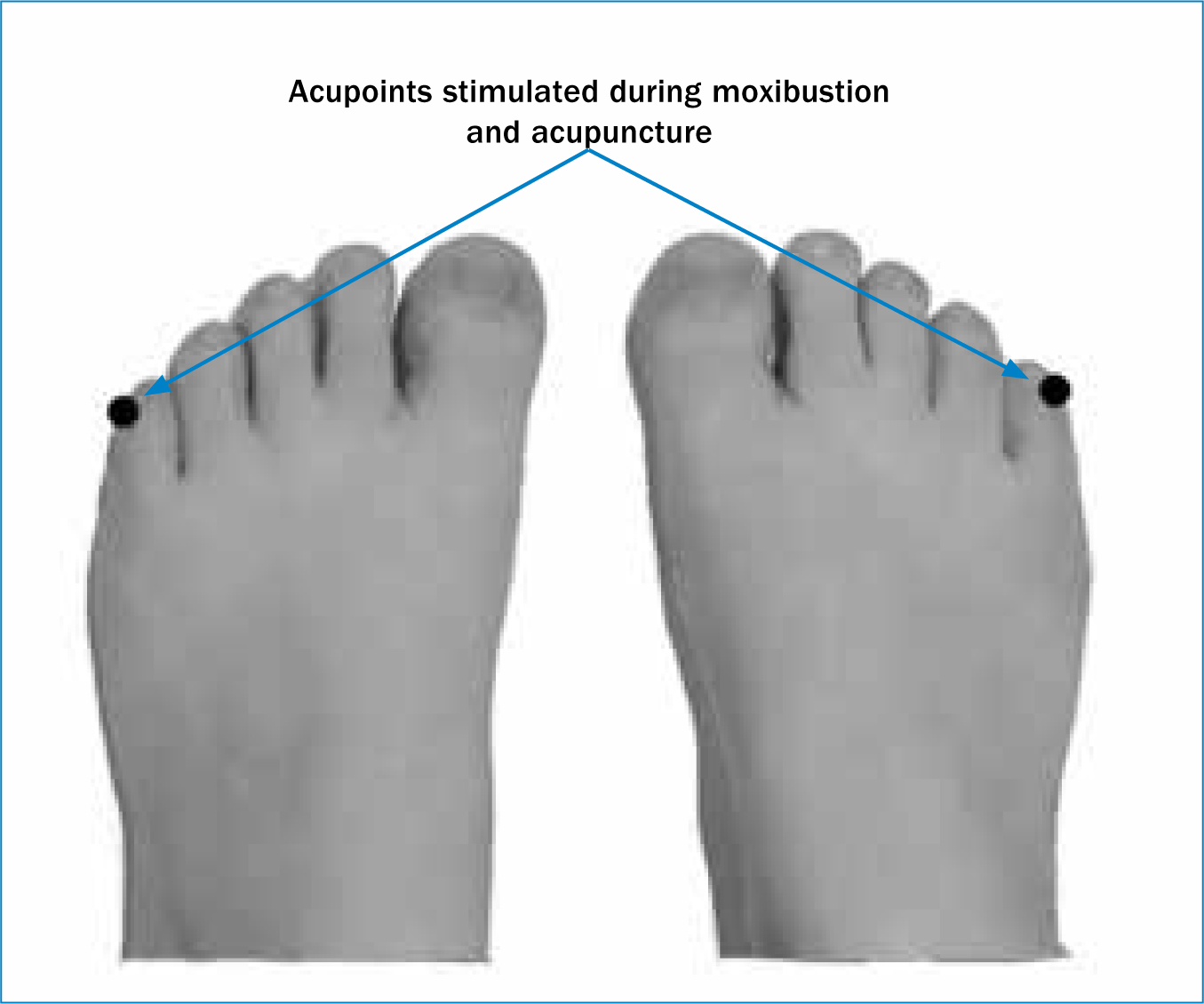
Moxibustion is a traditional Chinese medicinal practice that has been used for approximately 1300 years. It entails burning moxa (mugwort) close to acupoints, specifically bladder 67 (BL67) for cephalic version (Do et al, 2011) and should be considered between 33-35 weeks gestation as per the green-top guidelines (Impey et al, 2017) (Figure 1).
In a recent study (Do et al, 2011), pregnant women with a breech presentation were supervised by a research midwife and received instruction on moxibustion in order to self-administer the treatment for 10 minutes twice a day. The results revealed that women in the treatment group had increased incidence of cephalic presentation at birth and greater success with version following an ECV (Do et al, 2011). The researchers of this study discovered that most clinicians supported moxibustion for cephalic version, as it offered a gentle, non-invasive alternative that women found acceptable, although the authors also agreed that more research was required to determine the overall safety of the treatment (Do et al, 2011).
Limitations of the study included a small sample size, a lack of ethnic diversity, the potential for the researchers' biases to influence participants' responses and the potential for differences in treatment delivery to affect outcomes (Do et al, 2011). As a result, the most recent Cochrane review on moxibustion (Coyle et al, 2012) concurred that further research was needed to confirm (or contradict) the benefits of moxibustion use for cephalic version.
In order to establish a protocol to guide self-administration of moxibustion, Smith and Betts (2014) conducted a study to determine what experienced acupuncturists and researchers considered crucial components of treatment to encourage cephalic version. The authors aimed for consensus of around 70% between experts as to the best protocol for moxibustion use. Consensus was reached on the majority of issues: 80% of respondents agreed that moxa should commence between 34-35 weeks' gestation; 90% agreed to the use of smokeless/unscented sticks by self-administration, examining safety and correlating side-effects such as fetal and maternal outcomes (e.g. burns); and 70% agreed to a minimum of 10 days' treatment of 30 minutes once a day (Smith and Betts, 2014).
Acupoints stimulated during moxibustion and acupuncture
Acupuncture is most often referenced concurrently with moxibustion (Smith and Betts, 2014) and sometimes used interchangeably. Practice involves stimulation of acupoints by inserting fine needles into the target area (Sananés et al, 2010). For breech presentation, the BL67, like in moxibustion, is stimulated. In the midwifery context, acupuncture is not only used to turn a breech presentation (Walker, 2012) but also for relieving pregnancy symptoms such as nausea, vomiting (Jewell and Young, 2000) and pelvic pain (Pennick and Young, 2007) and for the induction or management of labour pain (Cho et al, 2010).
Discussion
Maternity services are one of the most highly litigated areas in healthcare in terms of clinical negligence claims (Anderson, 2013). To put the cost of claims into perspective, in England alone between 1 April 2000 and 31 March 2010, a total of £3.1 billion was paid out for the 5087 maternity clinical negligence claims (Anderson, 2013). After the assertions of Hannah et al (2000), it is not surprising that clinicians proceed with caution when faced with a breech presentation.
Although some evidence reports that caesarean section is safer for the fetus (Hannah et al, 2000; Kemfang Ngowa et al, 2012; Berhan and Haileamlak, 2016; Bin et al, 2016), these studies fail to fully acknowledge the implications of a caesarean section for both the neonate and mother. Vaginal birth stimulates essential physiological pathways in the neonate (Hyde et al, 2012). The consequences for the neonate of forgoing this stimulus include impaired lung function, decreased thermogenic response and altered metabolism, feeding, immune phenotypes and blood pressure. Indeed, altered blood pressure is not just limited to the neonatal period but can have effects that last into adult life (Hyde et al, 2012). The implications for women who have a caesarean section include higher risk of infection and deep vein thrombosis (DVT), greater postpartum blood loss, longer hospital stays, the risk of uterine rupture in subsequent pregnancies and complications such as placenta accreta, increta or percreta (Acosta, 2012; Macdonald and Magill-Cuerden, 2012; Pairman et al, 2014). Medical models of care may over-exaggerate risks regarding pregnancy and birth choices, as a way of reducing the chance of litigation. A model of risk management can create fear and have women doubting their body's ability to give birth to a breech baby vaginally (Lothian, 2012). Research suggests that if clinicians attending vaginal breech births are well experienced and competent, and strict criteria are adhered to, there are insignificant differences in neonatal outcomes (Walker, 2012; Homer et al, 2015).
Despite the global trends for caesarean section, research shows that 40% of women with a breech presentation at term would like the opportunity to have a vaginal birth (Vlemmix et al, 2014), even when procedures such as an ECV have failed (Homer et al, 2015). Some clinicians believe that breech presentation is a variation of normal, and midwifery models of care favour providing continuous, high-quality, low-intervention care where possible (Hastings-Tolsma and Goodman, 2012). Do et al (2011) demonstrated that midwives favoured complementary and alternative medicine interventions, but for women to make an informed choice, they need to be aware of all the care options available to them, not just those preferred by their caregiver (Kerridge et al, 2013). Clinicians therefore need to be aware of the alternative methods of cephalic version.
The emergence of specialty breech clinics in the UK and Australia (Catling et al, 2016) offers hope to women desiring a vaginal birth. In these clinics, women are given evidence-based, unbiased information on the implications of a breech presentation and are supported in their choice of birth, be it caesarean section or vaginal breech birth (Walker, 2012). Specialised, unbiased care is required for women with a breech presentation; unfortunately, many women find themselves needing to travel long distances to find such care (Homer et al, 2015), despite the benefits of continuity of care and carer being well established in the literature (Forster et al, 2016, Homer, 2016; Sandall et al, 2016).
Breech births will inevitably occur in clinical practice; therefore, clinicians need to consider up-skilling in order to facilitate vaginal breech birth safely (Walker, 2013). Simulation-based training has been suggested (Dresner-Barnes and Bodle, 2014) as a way of rectifying a lack of confidence and/or skills among clinicians. Some view vaginal breech birth as an obstetric skill (Kotaska, 2011), while others believe that an experienced midwife is the most appropriate health professional to oversee a vaginal breech birth (Walker, 2012; Odent, 2013). The issue is that, given the risks associated with vaginal breech birth and the well documented ‘safety’ of caesarean section, vaginal breech birth is not encouraged, especially since any ensuing negligence suit has the potential to be an expensive litigation case. A lack of knowledge and clinical expertise, in conjunction with the medico-legal implications, may be barriers to clinicians offering women with a breech-presenting fetus the opportunity to give birth vaginally.
Conclusion
The literature emphasises the need for clinicians to up-skill on vaginal breech birth techniques and for them to be able to mention alternative cephalic version techniques, even if they may not recommend them, so that the women in their care are able to make an informed decision. There is a need for further research into alternative methods of cephalic version, such as moxibustion and acupuncture, as these techniques offer a less aggressive approach than mainstream interventions, which appear to carry a greater risk to the fetus. In addition to the risks posed to the fetus, mainstream interventions may also be unacceptable to some women and contraindicated for others. Women should therefore be given the opportunity to explore all cephalic version options in order to increase the likelihood of a cephalic presentation and potentially avoid a caesarean section. Specialty breech clinics will provide more birth options for women and provide a platform for clinicians to obtain the skills lost in the post-Term Breech Trial era.

