Globally, cytomegalovirus is documented as the most frequently occurring congenital infection (Joseph et al, 2018). In the UK, approximately 1–2 of every 100 live births is affected by congenital cytomegalovirus (Griffiths et al, 2015). Gaur et al (2020) highlighted that it affects more newborn infants than many of the better-known congenital conditions, such as fetal alcohol syndrome, Downs syndrome and neural tube defects. Nevertheless, cytomegalovirus has continually experienced inattention from healthcare professionals and the public, with evidence suggesting it is the least well-understood infection affecting pregnancy (Alex, 2014).
As a result of the pathophysiological changes to the immune system that occur during pregnancy, pregnant women are susceptible to acquiring cytomegalovirus infection or experiencing a reactivation of a previous infection (Van Zuylen et al, 2014). Unfortunately, contracting either a primary or secondary cytomegalovirus infection during pregnancy can lead to transmission to the fetus, often resulting in congenital cytomegalovirus (Joseph et al, 2018).
Congenital cytomegalovirus can cause structural and neurological abnormalities, leading to hearing and vision impairment (Alex, 2014), seizures, cerebral palsy and generalised motor and cognitive deficits (McCarthy et al, 2011; Fowler and Boppana, 2018). It is difficult to diagnose congenital cytomegalovirus in newborns, as many infants do not display symptoms at birth (Joseph et al, 2018).
Diagnosing congenital cytomegalovirus antenatally also presents a challenge. Diagnosis during pregnancy is unusual, unless testing is carried out following suspicion of maternal infection, or the detection of fetal growth or structural abnormalities (McCarthy et al, 2011). To date, no newborn screening programmes have been introduced in the UK and prevention remains the overriding objective of addressing the condition (Fowler and Boppana, 2018; Joseph et al, 2018).
Research suggests that antenatal interventions based on behavioural modification of pregnant women could significantly reduce the burden of congenital cytomegalovirus (McCarthy et al, 2011; Griffiths et al, 2015). Preventive strategies for pregnant women include simple hygiene measures, such as hand washing, especially following exposure to children's saliva or urine, and avoidance of high-risk behaviours, which include sharing crockery, utensils or food and kissing children on the lips (Thackeray et al, 2018).
As midwives provide care for women across the childbearing continuum, they are ideally placed to provide preconception and antenatal advice relating to the prevention of maternal and fetal infections (Alex, 2014). Presently, in the UK, midwives offer advice on the prevention of teratogenic infections, such as listeriosis and toxoplasmosis, yet cytomegalovirus is not routinely discussed, despite evidence that it has a substantially greater burden (Griffiths et al, 2015; Vandrevala et al, 2019).
Before considering introducing antenatal interventions to reduce the burden of congenital cytomegalovirus, it is important to explore the background knowledge and understanding that midwives and childbearing women have of the condition (Schaefer et al, 2020). The present study aimed to address this, through a systematic review of the literature to explore midwives' and women's level of awareness and knowledge of cytomegalovirus infection, and its impact during pregnancy.
Methods
The electronic databases CINAHL, Maternity and Infant Care, EMBASE and PubMed were systematically searched using key words and terms, which included: midwife, midwives, woman, women, pregnant/expectant/childbearing woman, cytomegalovirus infection, CMV, congenital CMV, awareness and understanding.
‘Cytomegalovirus infection’ was searched as a subject heading, and the MeSH terms ‘nurse midwife’ and ‘midwifery’ were used during searches of EMBASE and PubMed. Supplementary searches included a search of the grey literature databases TRIP and Open Grey, and hand searching of reference lists. The searches of electronic databases and supplementary sources were carried out between 2 and 20 February 2021.
Inclusion and exclusion criteria
The included articles were required to have participants who were midwives, pregnant women, postpartum women or women who had at least one child under the age of 10 years. The articles must have been written in English, with the full text available and published after 2000. Their primary objective should have been understanding midwives or women's level of knowledge regarding cytomegalovirus infection and its impact on pregnancy.
Studies that included women who had never been pregnant, those that assessed knowledge of congenital cytomegalovirus across a range of different healthcare professionals, those that included attitudes towards cytomegalovirus preventative behaviours and those that included an intervention to improve women's knowledge of cytomegalovirus in pregnancy were all excluded.
Search results
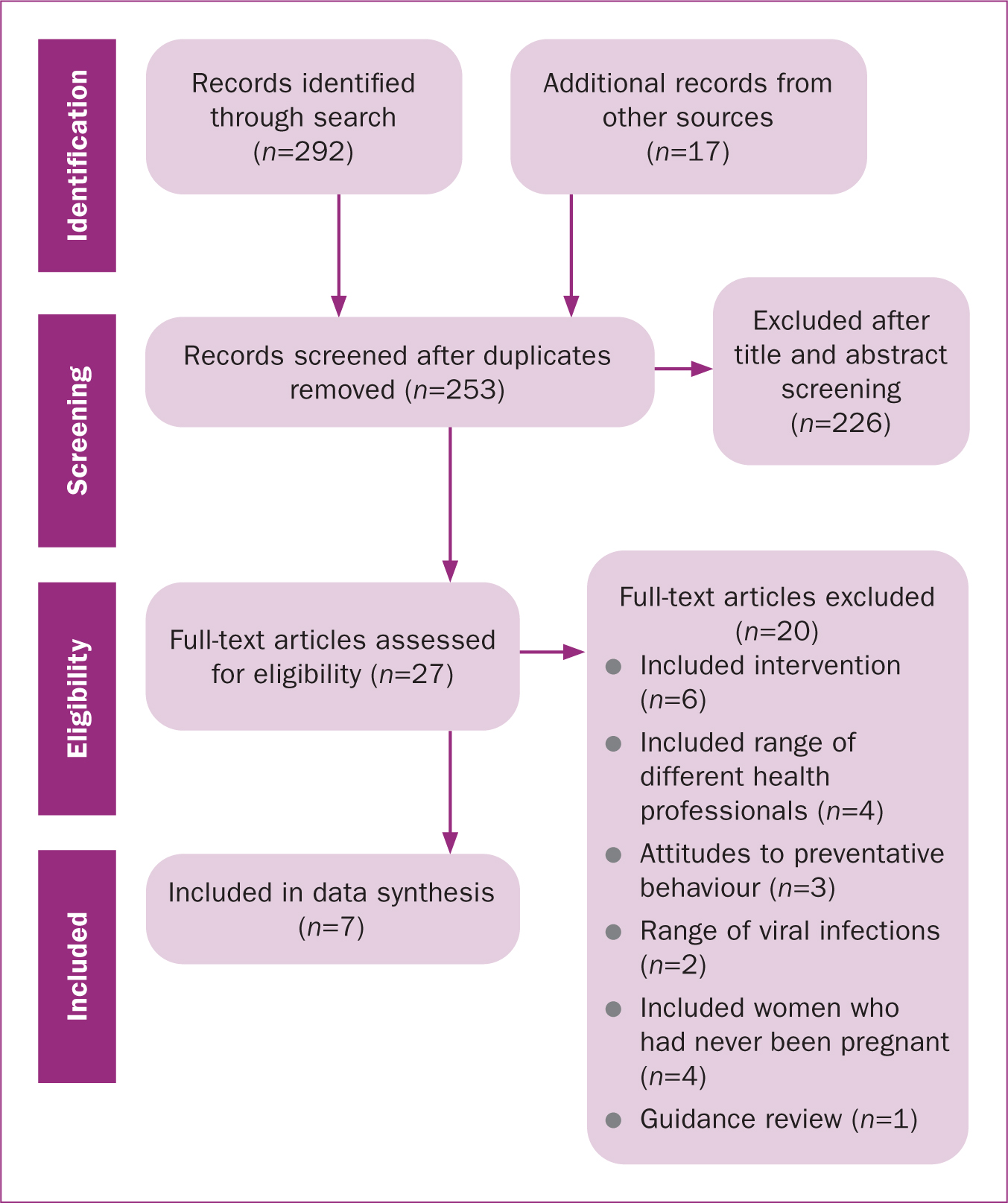
A total of 309 papers were identified through the search of all sources. Of these, 56 were discarded as duplicates and a further 226 were excluded after screening the title and abstract for relevance. The remaining 27 papers were examined in full, and seven papers met the eligibility criteria for inclusion. Figure 1 displays the search results.
Quality appraisal
The primary research articles all detailed descriptive cross-sectional studies using survey designs. Therefore, the AXIS critical appraisal tool was used to assess the quality of primary research. Each question on the checklist (Downes et al, 2016) was used, except questions 3, 7 and 14, which are not applicable to cross-sectional survey designs.
As a result of the limited number of papers obtained for the review, it was determined that all seven papers that met the eligibility criteria would be included. Overall, the risk of bias in primary studies was found to be high. Notwithstanding the identified risks of bias in the reviewed papers, the homogeneity in results across the studies indicated that the findings and recommendations of the researchers were likely to be valid (Bettany-Saltikov, 2012; LoBiondo-Wood, 2014), and they add important data for the evidence base relating to midwives and women's knowledge and understanding of cytomegalovirus and its impact on pregnancy.
Data analysis
To safeguard against bias, a data extraction tool was developed. It consisted of seven sections used to evaluate characteristics for each paper based on the objectives of the review and the questions outlined in the AXIS critical appraisal tool. The data extraction form was designed prior to data extraction and analysis being undertaken and the form was not amended following commencement of this stage of the review. Tables 1 and 2 display a summary of the extracted data from midwives and childbearing women respectively.
Table 1. Characteristics for included studies carried out among midwives
| Publication details | Main objectives | Design and population | Data collection and sampling | Main findings and recommendations | Strengths | Limitations |
|---|---|---|---|---|---|---|
| Pereboom et al (2014b) Netherlands | Primary: assess knowledge of Dutch primary care midwives relating to cytomegalovirus and level of information provided to pregnant women. Secondary: assess reasons for not providing pregnant women with information on cytomegalovirus | National cross-sectional survey with registered/practising midwives (n=330), 174 non responders, 15 excluded with reasons | Self-administered postal questionnaire developed by researchers; rationale for questions given. Not piloted or peer reviewed. Quota sampling | Midwives had limited knowledge/understanding, notably transmission routes and maternal infection. Majority did not provide women with information regarding prevention because of lack of knowledge. Further education and training on infection and prevention required | Representative sample, conduct and findings of study well reported | Inclusion criteria of one midwife per practice potentially biased results; midwife in each practice who had most knowledge or interest may have completed questionnaire |
| Von Gartzen and Hollins Martin (2013) Germany (Hannover) | Assess midwives' knowledge | Cross-sectional survey with registered/practising midwives (n=40), 111 non responders | Self-administered email questionnaire developed by researchers; peer reviewed prior to data collection. Purposive sample | Midwives had gaps in knowledge. Proposed education programmes for midwives | Questionnaire piloted and peer reviewed | Very small sample size (only 26.5% of target sample). Potential bias in sampling method. Limited discussion of findings |
Table 2. Characteristics for included studies carried out among childbearing women
| Study details | Main objectives | Design and population | Data collection and sampling | Main findings and recommendations | Strengths | Limitations |
|---|---|---|---|---|---|---|
| Cordier et al (2012) France (Paris) | Evaluate awareness and knowledge among pregnant women | Cross-sectional survey (n=362) (hospital A=234, hospital B=128). Multi-centre: Antoine Beclere Hospital (A), Foch Hospital (B), antenatal clinics | Written questionnaire based on survey from other researchers (Jeon et al, 2006); unable to ascertain survey validity as not disclosed in reference. Convenience sample | Greater awareness in hospital A. Overall, knowledge less than of other congenital conditions and knowledge of impact on fetus was poor. Women should be informed about congenital cytomegalovirus during antenatal period. Further research required on best way to educate women on prevention in pregnancy | Two settings for representation of different approaches to provision of information. Appropriate inclusion criteria determined | Small sample size, urban setting may not be representative of target population, bias possible from high percentage (47%) healthcare workers in sample and unequal weighting (64% hospital A, 36% hospital B) |
| Lim et al (2012) Singapore | Determine level of awareness and attitudes towards antenatal testing | Cross-sectional survey (n=200), 331 non responders. Single centre: Singapore General Hospital, antenatal clinic | Self-administered questionnaire designed by authors. Convenience sample | Limited knowledge prior to participation. Awareness largely restricted to healthcare employees | Context for study setting provided. Questionnaire piloted on pre-test sample (n=10) | Low response rate/small sample, potential for self-selection bias |
| Mazzitelli et al (2017) Italy (Cantanzaro) | Assess knowledge of infection, consequences and prevention in pregnant women | Cross-sectional survey (n=350). Single centre: Pugliese-Ciaccio Hospital, antenatal clinic | Questionnaire designed by researchers, non-validated; rationale for questions given. Convenience sample | Lack of awareness of infection and prevention (no difference in knowledge among backgrounds, high vs low education, primigravida vs parous). Information on virus and preventation should be provided. Suggestion: information campaigns in school-aged girls | Blinding of researchers (anonymity). 100% response rate | Small sample size, limited by time. Limited results reported in narrative form, little documentation in tables for reader's reference and appraisal of statistical analysis |
| Willame et al (2015) Switzerland (Geneva) | Evaluate knowledge of infection and prevention among pregnant women | Cross-sectional survey (n=314), 150 non responders. Single centre: University of Geneva Hospital, postnatal ward | Adapted questionnaire based on design by other researchers (Cordier et al, 2012). Convenience sample | Knowledge low (lower than other pregnancy infections). Knowledge higher among women employed as healthcare workers or with higher education. Women receiving antenatal care from midwives and general practitioners rarely informed, need to improve awareness | Recruitment anonymised, questionnaire in multiple languages (representative of population), flowchart of enrolment provided | Small sample, self-selection bias (participants); mentioned possible bias toward educated women |
| Wizman et al (2016) Canada (Montreal) | Primary: determine susceptibility and awareness. Secondary: determine risk factors for susceptibility and lack of awareness | Cross-sectional survey, postpartum women (n=491), 505 recruited, 14 excluded with reasons). Single centre: Hospitalier Universitaire, postnatal ward | Researcher administered questionnaire; designed by researchers, rationale for questions given Convenience sample | General lack of awareness. Education of health professionals may impact knowledge among population/pregnant women | Inclusion and exclusion criteria provided. Statistical results provided | Single centre study, may not be representative. Small sample size. Potential for selection bias. Background information only collected for one third of recruitment phase |
Results
Study characteristics
Overview
Two papers carried out research among a population of midwives (Von Gartzen and Hollins Martin, 2013; Pereboom et al, 2014a) and five among women (Cordier et al, 2012; Lim et al, 2012; Willame et al, 2015; Wizman et al, 2016; Mazzitelli et al, 2017). The studies were conducted internationally, representing research in seven different countries, including Germany (Von Gartzen and Hollins Martin, 2013), France (Cordier et al, 2012), Singapore (Lim et al, 2012), Italy (Mazzitelli et al, 2017), Switzerland (Willame et al, 2015), Canada (Wizman et al, 2016) and the Netherlands (Pereboom et al, 2014a). All studies were published between 2012 and 2017.
Methodology, sampling and data collection
Homogeneous methodologies were used, with all studies conducted using observational cross-sectional survey designs. Settings included antenatal clinics (Cordier et al, 2012; Lim et al, 2012; Mazzitelli et al, 2017) and postnatal wards (Willame et al, 2015; Wizman et al, 2016). Studies among women were conducted on single hospital sites, apart from the French study, which comprised a multicentre study with data collection carried out at two different hospital sites (Cordier et al, 2012).
The studies of midwives' views were conducted over larger geographical settings, with Pereboom et al (2014a) taking a national sample of midwives from across the Netherlands, and Von Gartzen and Hollins Martin (2013) sampling midwives practising in Hanover. The studies of women used convenience sampling, while Pereboom et al (2014a) obtained their sample of midwives through quota sampling, and Von Gartzen and Hollins Martin (2013) carried out purposive sampling. Data were collected via self-administered questionnaires, except for Wizman et al (2016), who opted for a researcher-administered questionnaire.
A total of 370 registered midwives and 1717 women were included across the seven studies.
Midwives' educational awareness
The studies with midwives revealed gaps in their knowledge of cytomegalovirus infection, with both studies reporting that participants lacked accurate knowledge of routes of transmission, preventive measures and maternal and neonatal symptoms. Von Gartzen and Hollins Martin (2013) documented that only eight midwives out of a sample of 40 felt that they were well informed in relation to cytomegalovirus infection, and Pereboom et al (2014a) reported that almost half of the midwives in their sample (45.7%) indicated the most common reason for not informing women about cytomegalovirus infection was a lack of knowledge about preventative methods and risk factors for contracting the infection.
Pereboom et al (2014a) described midwives obtaining knowledge of cytomegalovirus infection primarily from formal midwifery education (89.6%), the internet (63.2%) and professional literature (58.9%). Von Gartzen and Hollins Martin (2013) did not record sources of knowledge for their participants.
Pregnant women's educational awareness
The data collected among childbearing women identified that they had limited awareness of cytomegalovirus infection. Lim et al (2012) reported only 20% of women were aware of cytomegalovirus infection prior to participation in their study. Similarly, Wizman et al (2016) and Willame et al (2015) found that 85% and 61% of their respective samples of postpartum women were unaware of cytomegalovirus infection. Conversely, Mazzitelli et al (2017) and Cordier et al (2012) documented higher levels of awareness among their samples of pregnant women, reporting that over 50% of their participants stated that they had prior knowledge of cytomegalovirus infection. However, Cordier et al (2012) highlighted that awareness among women was significantly higher in the hospital with a policy for provision of information to antenatal women. Willame et al (2015) and Cordier et al (2012) reported that women were less likely to be aware of cytomegalovirus infection compared with other infections affecting pregnancy, such as rubella and Group B streptococcus.
Over three quarters (77.4%) of women in the sample obtained by Mazzitelli et al (2017) knew cytomegalovirus infection was potentially dangerous for the fetus; however, most women were unable to correctly identify how to effectively prevent cytomegalovirus in pregnancy. In Cordier et al's (2012) study, women at both hospital sites had a high level of knowledge regarding preventative measures against contracting cytomegalovirus, specifically, the need for frequent handwashing and avoidance of sharing food, utensils and crockery. However, knowledge of neonatal symptoms of congenital cytomegalovirus infection was low, with less than half of all participants correctly identifying common sequalae. Willame et al (2015) also investigated women's knowledge of the risks and possible outcomes of cytomegalovirus infection and found that women rarely identified common symptoms of congenital cytomegalovirus, such as deafness and neurodevelopmental delay.
Education and employment was reported to affect knowledge. Women's awareness of cytomegalovirus was better among those with a higher level of education, specifically, third level college or university attendance, with four of the five studies reporting statistically significant differences when compared with women who left education at secondary school level or lower (Cordier et al, 2012; Lim et al, 2012; Willame et al, 2015; Wizman et al, 2016). Willame et al (2015), Cordier et al (2012) and Lim et al (2012) stated that participants who were employed as healthcare workers were significantly more likely to have an awareness of cytomegalovirus infection compared with non-healthcare workers.
The association between women's parity and prior knowledge of cytomegalovirus infection was less clear, with Cordier et al (2012) reporting higher levels of awareness among women who had already experienced a pregnancy, whereas Mazzitelli et al (2017), Wizman et al (2016) and Willame et al (2015) observed no significant differences in level of awareness between primiparous and multiparous women.
Sources of knowledge for women
Common sources of information for pregnant women reported across the studies included their obstetricians, the workplace, media and family (Cordier et al, 2012; Lim et al, 2012; Willame et al, 2015). Willame et al (2015) compared sources of information, reporting that women who received antenatal care from general practitioners or midwives were less likely to have been informed of cytomegalovirus infection than women who received their care from an obstetrician. However, among participants who had knowledge of cytomegalovirus, only half had been informed about prevention during the antenatal period. Excepting Cordier et al (2012), active discussion by healthcare professionals relating to the prevention of cytomegalovirus infection in pregnancy was limited.
Discussion
For several decades, the literature has recognised that the most commonly occurring congenital infection is cytomegalovirus (Kadambari et al, 2020; Thigpen, 2020). Affected infants experience sequelae, which include bilateral sensorineural deafness, visual impairment and neurological and cognitive deficits (Fowler and Boppana, 2018; Schaefer et al, 2020). However, it has been suggested that congenital cytomegalovirus is an underappreciated condition among healthcare professionals and the public (Alex, 2014; Binda et al, 2016). The findings of this review support this observation, revealing that midwives and childbearing women lacked awareness and knowledge of cytomegalovirus infection, and subsequently misunderstood the risks in pregnancy, notably the potential consequences of congenital cytomegalovirus.
The National Institute for Health and Care Excellence (2021) recommends that pregnant women should be offered all available information and advice regarding their health and wellbeing and that of their unborn baby. Consequently, midwives, who comprise the lead healthcare professionals for pregnant women in the UK (Midwifery 2020 Programme, 2010), have a duty to inform women about infections that could have implications for maternal or fetal health (Nursing and Midwifery Council, 2019). Midwives practising in the UK routinely offer information and advice regarding prevention of infectious diseases in pregnancy, including listeriosis, toxoplasmosis and rubella (Griffiths et al, 2015). However, despite the risks to the fetus, studies reveal that women are not routinely informed about cytomegalovirus infection (Vandrevala et al, 2019; 2020).
The absence of national guidelines or recommendations relating to prevention of maternal cytomegalovirus infection may be a barrier to midwives caring for women in the UK (Griffiths et al, 2015; Rawlinson et al, 2017). In the USA and Australasia, public health organisations recommend antenatal discussions inform women of the risks of contracting cytomegalovirus infection (Adler and Nigro, 2013; Diener et al, 2020). Similarly, in many European countries, midwives are encouraged to discuss prevention of cytomegalovirus infection with pregnant women (Pereboom et al, 2014b; Griffiths et al, 2015).
Studies reveal that despite the international recommendations, healthcare professionals, including midwives, do not commonly discuss cytomegalovirus with pregnant women (Pereboom et al, 2014b; Rawlinson et al, 2017; Pesch et al, 2020). A notable exception can be found in France, where the provision of antenatal information regarding prevention of maternal cytomegalovirus infection is a policy advocated by the National College of French Gynaecologists and Obstetricians (Fellah et al, 2020). The study by Cordier et al (2012), which was based in France, reflected increased levels of awareness among pregnant women compared with other studies. This suggests that the implementation of a national policy could result in a greater impact on improving awareness of the significance of cytomegalovirus infection among pregnant women.
A prerequisite to increasing awareness among pregnant women is ensuring that midwives have adequate knowledge and understanding of cytomegalovirus and its impact on pregnancy (Alex, 2014). Pesch et al (2020) highlighted that if a midwife's knowledge is low, then they are less likely to inform women and effectively counsel them regarding prevention of cytomegalovirus infection. Midwives included in the reviewed studies indicated that they had acquired their limited knowledge of cytomegalovirus infection from a combination of professional education and resources, and publicly accessible information on the internet. Thus, researchers recommended that midwives require additional education on cytomegalovirus and its significance in the antenatal period (Von Gartzen and Hollins Martin, 2013; Pereboom et al, 2014a).
Despite many of the surveyed women having limited knowledge of cytomegalovirus infection, four of the five studies reviewed found that two distinct subsets of women had a slightly increased level of awareness and understanding, including women with a high level of education and women who had been employed as healthcare workers. This suggests that information on cytomegalovirus infection is likely to have been obtained from formal educational settings; however, the women who participated in the studies disclosed that their main sources of information were healthcare professionals, specifically obstetricians, friends, family and the media (Cordier et al, 2012; Lim et al, 2012; Willame et al, 2015).
Education of pregnant women is relatively inexpensive (Van Zuylen et al, 2014; Griffiths et al, 2015), and in the context of preventing congenital cytomegalovirus, it could have significant economic savings for health and social care services (Retzler et al, 2019). Griffiths et al (2015) highlighted that pregnant women are often motivated to modify their behaviours to prevent fetal exposure to harm, such as not consuming alcohol or cigarettes while pregnant. McCarthy et al (2011) cautioned that behavioural interventions can be difficult to monitor and time consuming to implement. Antenatal education represents the most readily accessible method to communicate information and advice and subsequently reduce the risk of fetal exposure to cytomegalovirus infection (Levis et al, 2017).
Education of the general population could also be of benefit, as research has consistently shown that in addition to maternity populations, general awareness of cytomegalovirus infection is low (Manicklal et al, 2013; Vandrevala et al, 2020). Binda et al (2016) highlighted that the lack of attention given to congenital cytomegalovirus by the media, and the absence of health education campaigns, has intensified the lack of awareness of the condition in populations. Pereboom et al (2014a) recommended that public health organisations should develop resources to inform the public. Von Gartzen and Hollins Martin (2013) advocated for the introduction of public health messaging to prevent ongoing transmission of cytomegalovirus in the population.
Mazzitelli et al (2017) and Cordier et al (2012) advocated for raising awareness of cytomegalovirus infection among teenagers and women who may not enter higher education. As with many other infectious diseases, cytomegalovirus is more prevalent among younger populations and women with lower socioeconomic status (Navti et al, 2016). Perinatal mortality reports and national guidelines consistently identify social deprivation and maternal vulnerability, such as teenage pregnancy, as risk factors for poor fetal and neonatal outcomes (National Institute for Health and Care Excellence, 2010; Perinatal Institute for Maternal and Child Health, 2011; Draper et al, 2020). Improving awareness of cytomegalovirus infection among these vulnerable groups may reduce the spread of the virus among the population (Mazzitelli et al, 2017; Kadambari et al, 2020), with consequential reduction in rates of congenital cytomegalovirus.
Limitations
The methods of convenience sampling used by most of the researchers risked bias of atypical participants (Polit and Beck, 2018), as did the researcher-selected participants of Wizman et al (2016) and Von Gartzen and Hollins Martin (2013). The method of quota sampling used by Pereboom et al (2014a) had the potential to randomly select participants, which may increase representativeness of the sample; however, the researchers noted that midwives who had the most knowledge or interest in cytomegalovirus may have chosen to participate, which could have over-represented midwives' knowledge in relation to cytomegalovirus infection.
The most significant limitation of the reviewed studies was the potential bias resulting from non-responders in each of the eligible participant populations (Bowling, 2014). Non-response rates for the surveys conducted by the researchers were generally high, apart from Mazzitelli et al (2017) and Wizman et al (2016) who achieved a 100% and a 97.2% response rate respectively. Generally, in quantitative research, the larger the sample, the greater the chance of representing the target population (Bowling, 2014). Therefore, the high levels of non-response from eligible participants, and the consequent small sample sizes obtained by the researchers, may have resulted in significant non-response biases (Kunaviktikul et al, 2020). Nonetheless, it is not uncommon for non-response rates to be high for survey research, especially if the topic under investigation is not widely known or understood (Polit and Beck, 2018).
A significant limitation of this systematic review is that it was conducted by a single individual. To account for this limitation, the review was supervised by an independent university lecturer, who offered guidance and critical feedback throughout the data gathering and analysis processes. A further limitation resulted from restricting the search of the literature to English language papers and full-text articles.
Although this review presents evidence relating to midwives and women's combined awareness and understanding of cytomegalovirus infection during pregnancy, the findings are limited by the small number of primary research papers that were eligible for inclusion.
Recommendations
Further research is required to investigate knowledge and understanding of maternal cytomegalovirus infection among larger populations of midwives and childbearing women. Pregnant women need to be provided with information about cytomegalovirus, including how it may affect the fetus and how to reduce the risk of exposure during pregnancy. Midwives require additional educational sessions to increase their knowledge and understanding of maternal cytomegalovirus infection and congenital cytomegalovirus. Additionally, public health organisations should aim to increase population awareness of cytomegalovirus infection and the significance of contracting the infection during pregnancy.
Conclusions
Congenital cytomegalovirus is the most commonly occurring congenital infection worldwide, affecting more neonates and children than many other widely recognised congenital conditions. However, the available evidence suggests that there is a lack of awareness among populations concerning congenital cytomegalovirus. Furthermore, to date, congenital cytomegalovirus has received inadequate attention from healthcare professionals and policy commissioners.
In the UK, there are no screening programmes for either maternal or neonatal cytomegalovirus, and the objective remains prevention of maternal infection. Midwives have a significant role in the prevention of maternal and fetal complications that can result from exposure to infectious agents during pregnancy. This systematic review found that midwives have a restricted knowledge and understanding of how cytomegalovirus infection can affect pregnancy. Midwives were found to have a limited understanding of antenatal transmission of the virus, maternal and neonatal symptoms and measures to reduce the risk of maternal infection. Likewise, many childbearing women included in the studies displayed a limited awareness of cytomegalovirus infection and lacked knowledge of the risks of congenital cytomegalovirus and how to avoid cytomegalovirus infection during pregnancy.
Key points
- Congenital cytomegalovirus is the most common global congenital infection.
- Maternal infection with cytomegalovirus can be prevented through simple behavioural changes in pregnancy.
- Cytomegalovirus is identified as the least well understood infection affecting pregnancy.
- In many countries, midwives do not routinely discuss cytomegalovirus with women attending for antenatal care.
- The findings of this review reveal many midwives and childbearing women are unaware of the significance of cytomegalovirus infection during pregnancy, leading to subsequent misunderstanding of the risks and potential consequences of congenital cytomegalovirus.
CPD reflective questions
- What are the most common complications of congenital cytomegalovirus?
- What behavioural changes can pregnant women implement to prevent antenatal infection with cytomegalovirus?
- Do midwives in your workplace routinely discuss cytomegalovirus infection with antenatal women?
- What sources of information are available in your workplace for parents following a diagnosis of congenital cytomegalovirus for their infant?


