The provision of tongue tie services has previously been the subject of investigation by the parents’ charity, the National Childbirth Trust (NCT). In 2016, Fox et al (2016) reported the results of a survey undertaken of the 167 NHS acute trusts/boards across the UK and 20 community trusts available in the UK at the time. Their published findings were taken from 86 respondents, a 51% response rate. They concluded that tongue tie services were ‘a post code lottery’ and made several recommendations to help address variability and improve care for families (Fox et al, 2016). Their main findings included that 54% of respondents accepted referrals for bottle-fed babies (18% did not, the remaining trusts did not know), and most (88%) used oral assessment alone for referral criteria (assessment tools had not been generated at that time). The maximum age for referral ranged from 1–2 months to unlimited (limit of 1–2 months: 13%, limit of 2–3 months: 16%, limit of 3–4 months: 33%, no limit: 33%), and waiting time between referrals and receiving treatment varied (67% were given an appointment within 2 weeks). Reported barriers to setting up a service included funding, availability of staff, training and venue.
As the survey was conducted and published over 6 years ago, there was interest among tongue tie practitioners and the All-Party Parliamentary Group on Infant Feeding and Inequalities as to whether there had been any changes in provision and if the COVID-19 pandemic had affected existing provision. The group met to discuss this on 8 December 2021, and the survey described in this article was undertaken as a result.
Tongue tie or ankyloglossia
All babies are born with a lingual frenulum (mucous membrane tissue under the tongue) that is part of normal oral anatomy. Ankyloglossia is defined as ‘a congenital anomaly characterised by an abnormally short lingual frenulum, which restricts the mobility of the tongue’ (National Institute for Health and Care Excellence (NICE), 2005). If the tongue is restricted in its normal movement and function by being tethered to the floor of the mouth by a short frenulum, sucking is adversely affected. This function of the tongue and the appearance of the frenulum is described as ‘tongue tie’. The most recent incidence study (Knight et al, 2023) reports that 3–11% of babies can be diagnosed with tongue tie.
In the UK, when tongue tie is suspected or a diagnosis made, there is usually referral for treatment, which often involves frenulotomy. Frenulotomy is a surgical procedure that involves cutting (or dividing) the lingual frenulum with sharp, blunt-ended scissors (NICE, 2005). In babies, it is considered to be a simple and safe procedure, which can be safely undertaken in a variety of clinic settings or in the home and does not involve anaesthetics. Services offering frenulotomy are regulated by the Care Quality Commission.
Most aspects of tongue tie in infants (including definition, diagnosis, prevalence, effect or otherwise on infant feeding, assessment/diagnostic tools, quality of infant feeding support available, all aspects of treatment by frenulotomy and follow-up care afterwards) come under discussion and some disagreement among practitioners. For example, the term ‘posterior’ tongue-tie as a diagnosis is endorsed by some (Ghaheri et al, 2022), while others express doubt and reject the existence and diagnosis (Dhir et al, 2022). Laser versus scissors for performing frenulotomy is another example of difference of opinion between practitioners, although both are deemed safe and effective (Dell'Olio et al, 2022; Dhir et al, 2022; Murias et al, 2022; Hill and Pados, 2023). The evidence base for most of these aspects is not considered to be strong and much further research is needed. However, NICE (2005) state that babies assessed as having a tongue tie, who are struggling with breastfeeding after skilled support with positioning and attachment, may benefit from frenulotomy.
Methods
In 2021, a small working party from the Association of Tongue Tie Practitioners was set up to explore the possibility of using the original NCT survey as the foundation for a new survey. The NCT were approached and agreed to provide the team with the original questionnaire from Fox et al (2016). This was modified to form a new, shorter questionnaire, which included questions specific to the COVID-19 pandemic. The modified questionnaire excluded three of the original questions on how the tongue tie service was commissioned, how far away referrals were accepted and what barriers existed to having an external referral pathway for tongue tie. The survey was shorter because of restrictions from the team, who were completing the project voluntarily and in their own time; it was deemed more important to include questions on COVID-19 without extending the time taken to complete the survey. No budget or funding was obtained.
A freedom of information request was sent to all 179 trusts or health boards in England, Scotland and Wales at the time, with 130 responses received, which equates to a 72.6% response rate. Trusts were given 6 weeks to return their responses.
Ethical considerations
As for the original survey (Fox et al, 2016), the present survey did not ask personal questions or for any patient details and the trusts were unnamed in reporting. Ethical approval from a research ethics committee was therefore not required.
Results
Overall, 74.6% (n=97) of the trusts had a tongue tie service. Of the remaining 25%, 24% referred babies elsewhere for treatment and 1% had no provision at all. The previous survey (Fox et al, 2016) showed 43% of trusts had a service. This is an overall increase in the proportion of tongue tie services among respondents by 32%.
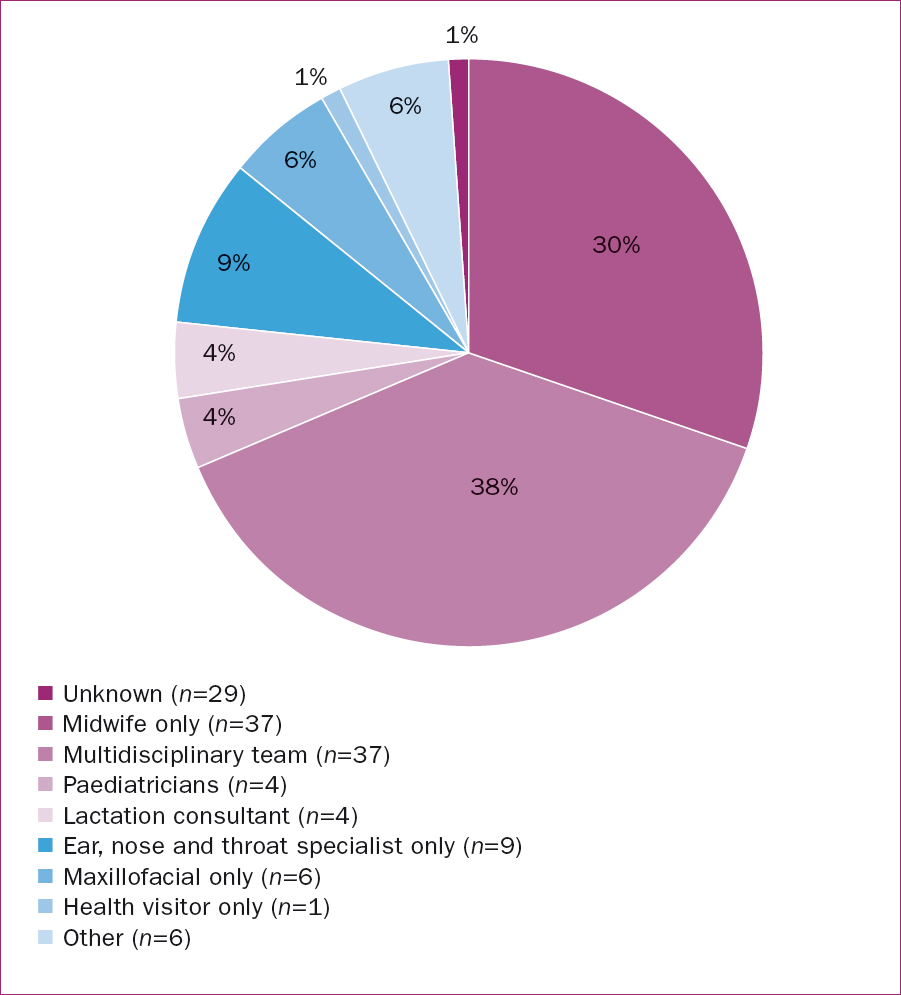
Healthcare professional(s) involved in care
As Figure 1 shows, when assessing the healthcare professionals involved in providing care at the point of contact with the mother and baby, most services involved a multiprofessional team, 38% of which included a midwife with a doctor. A further 30% were run by a midwife only, making a total of 68% of services that included a midwife, the largest single group of professionals involved. Where doctors provided services alone, they were either ear, nose and throat specialists (largest single group: 10%), Maxillofacial (6%) or paediatricians (4%). Lactation consultants (4%) were likely to be in a supporting role, rather than performing frenulotomy, as this is not deemed to be part of the lactation consultant's role. They will also have been registered nurses or midwives, as only a healthcare professional (who may also be a lactation consultant) would perform frenulotomy (NICE, 2005).
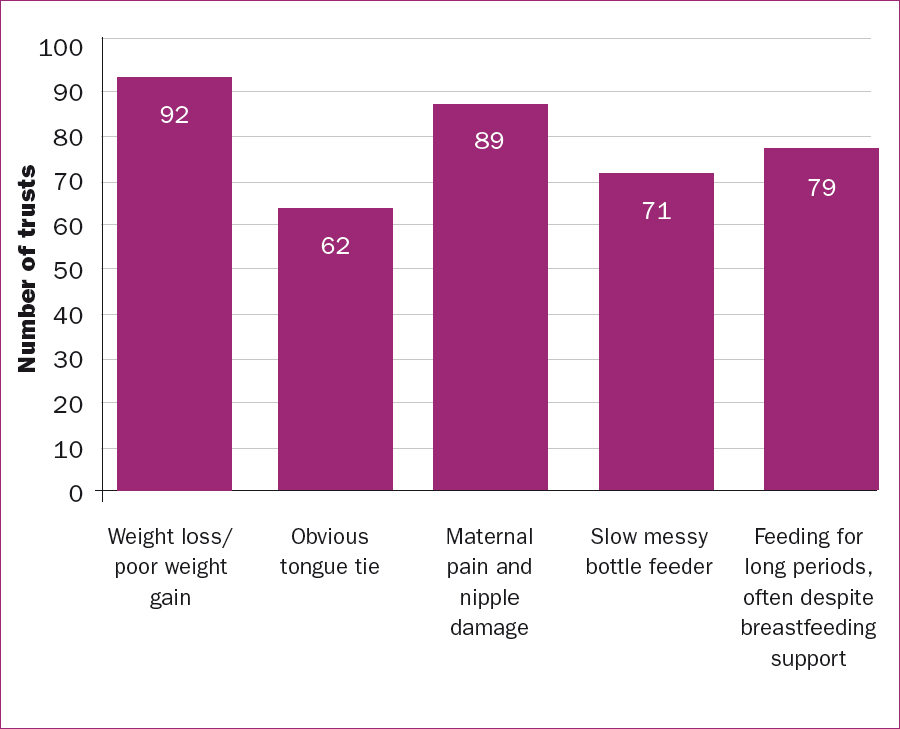
Referral criteria: symptoms, signs and cut-off age
Many symptoms and signs, and combinations of these, were cited as referral criteria to tongue tie services (Figure 2). The most common was infant weight loss or poor weight gain (92%) and maternal pain and nipple damage associated with breastfeeding (89%). Others included prolonged feed duration and increased frequency of feeds (79%), dribbling or ‘messy’ feeding (71%) or an obvious tongue tie being visible (62%).
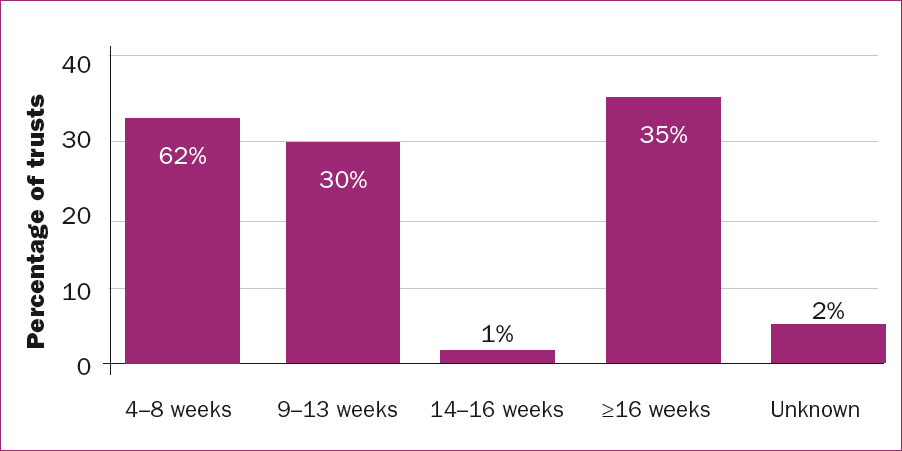
The maximum cut-off age for babies being referred, and thereby being able to attend a clinic, varied (Figure 3). The lowest maximum age was 4 weeks, and 31% of trusts with a service had a maximum age in the 4–8 week range. Almost a third (29%) had a maximum age in the of 9–13 week range, and some trusts (35%) took referrals for babies 16 weeks or over into their clinics.
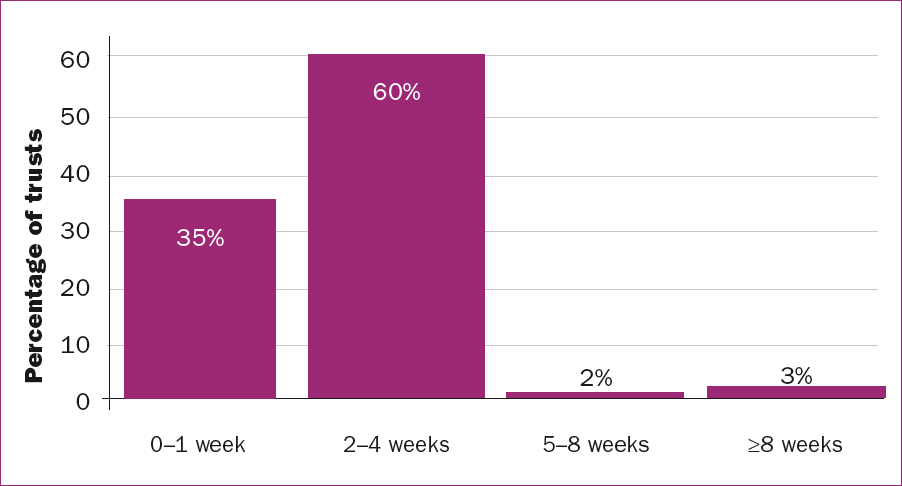
Waiting time between referral and appointment
Figure 4 shows the waiting time between referral and receiving an appointment. Over a third (35%) of trusts had a waiting time of up to 1 week. The majority cited a waiting time of 2–4 weeks (60%). A small number of services had wait times of up to 5–8 weeks (2%) and 3% cited 8 weeks or more.
Assessment tools
Different assessment tools were used across the tongue tie services (Figure 5). The Hazelbaker Assessment Tool for Lingual Frenulum Function (Hazelbaker, 2010) was the most commonly used (53% total), either as the only assessment tool (31%) or combined with another (22%).
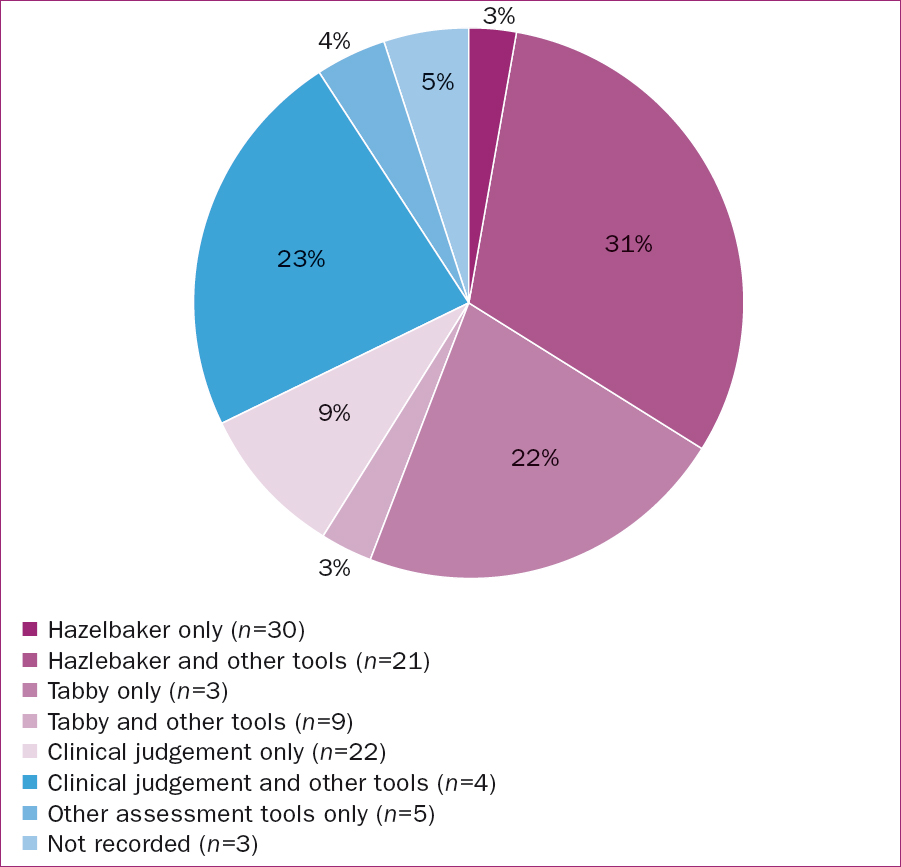
The next most common method of assessment was ‘clinical judgement alone’ (22%). It was not clear from the data what aspects were included in the clinical judgement, whether it included feeding observation, appearance of the frenulum and/or tongue function, or all three.
An assessment tool called ‘Tabby’ (Ingram et al, 2019) appeared to be gaining use in wider practice, in combination with other tools, with 10% of services incorporating this tool as a method of assessment. This tool was published in 2019, and was thus not available at the time of the previous survey.
Follow-up and recommended routine aftercare following frenulotomy
The majority of trusts provided no follow-up care unless requested by parents (45%), while 32% followed up via phone call or text. Other follow up may have been undertaken by midwives, health visitors or reviews in clinics, and some trusts may have used a combination of these methods, although exact data were not provided.
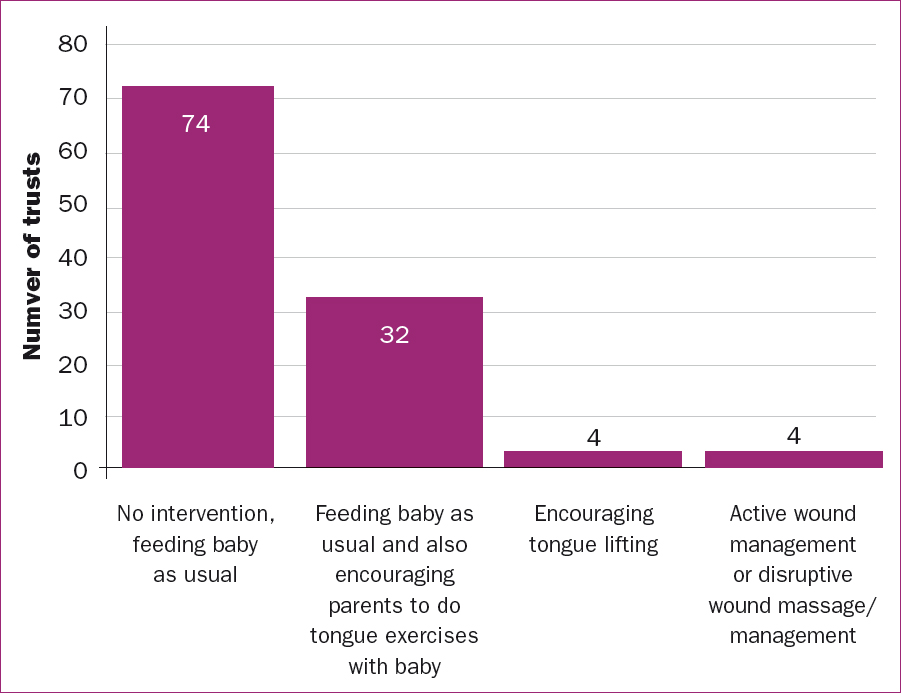
The most common recommended aftercare following frenulotomy was to feed the baby as usual (74%). Further aftercare was suggested by 32 of trusts in the form of ‘tongue exercises’ (such as encouraging the baby to stick their tongue out, by a parent encouraging the baby to suck on the adult's finger while it was being withdrawn from the baby's mouth, as in a ‘tug of war’ game). Four services encouraged parents to do either ‘tongue lifting’ or ‘active wound management’ or ‘disruptive wound massage’. These processes can involve placing fingers either side of the baby's tongue and ‘lifting’ the tongue up, in the case of active wound management, or putting fingers into the wound to massage or stretch it, for disruptive wound massage.
Effects of COVID-19
The survey asked general open questions and invited comments as to how tongue tie services had been affected during the height of the COVID-19 pandemic in 2020. The majority of trusts reported that they had stopped their services completely for most of the year. This was the result of discussion within trusts and the Association of Tongue Tie Practitioners (ATP) about whether frenulotomy was classed as an aerosol generating procedure or not. In view of this, many trusts deemed it ‘unsafe’ to continue.
Trusts gradually reinstated their services during 2021, although the survey respondents reported that frequency and duration of clinics was reduced because of staff sickness levels, staff being redeployed elsewhere or social distancing and cleaning measures. Many practitioners reported high levels of anxiety in parents.
Anecdotally, the ATP reported that many private practitioners experienced a significant increase demand for their services, thought to be because of the reduced or absent NHS services.
Discussion
Since the NCT survey (Fox et al, 2016), there are 25 more NHS trusts providing tongue tie services. However, in common with the findigns from the previous survey, there is still great variability and inequity between services, and so the ‘postcode lottery’ still exists.
Although the previous survey identified that tongue tie services providers were a mixture of midwives and different specialist doctors, the present survey reported that midwives are now the usual lead health professional (68%, n=65) and ear, nose and throat specialists are the most commonly involved consultants. This is likely to be because midwives can provide the necessary infant feeding knowledge and skills. NICE (2005) state that frenulotomy must be performed by a ‘registered healthcare professional’ who has been ‘properly trained’. There is no guidance given by either the Nursing and Midwifery Council or the Care Quality Commission as to who else might be involved.
Referral criteria in terms of symptoms, signs and maximum referral age remains variable, with weight loss being the most common. This shows the lack of consistency in what is considered to be the most important sign or symptoms, and the rationale for ‘most important’ is not clear. For example, mothers might consider painful breastfeeding to be a major issue, whereas providers may regard a tongue tie being obviously visible or weight loss as more important. As weight loss is often regarded as significant, there may be cases where a mother adheres diligently to a feeding plan (which is not sustainable in terms of her lifestyle or enjoyment of breastfeeding), and therefore her baby does not lose weight and will not be referred. Evidence for this is largely anecdotal, as it is frequently reported by both NHS and private practitioners to the ATP.
A maximum cut off age can disadvantage mothers. Some mothers may find that their baby manages to breastfeed in the first few weeks before problems become apparent. This could be the result of hormonal changes during lactation, which affect flow and therefore transfer to the baby (Watson, 2013). This mother and baby may then pass the cut off age for referral to a local clinic and be left with no NHS service available.
Around a third of trusts who responded to the survey achieved a waiting time of only 1 week between referral and appointment. If a mother can be seen within a week, she is more likely to continue with breastfeeding, as compared to a mother who has to wait 2 or more weeks for an appointment (Finigan and Long, 2013). Longer waiting times may therefore encourage women to switch to bottle feeding for a baby who is not feeding properly, and be excluded from referral to clinics on that basis. This is common in NHS clinic referral/acceptance criteria (Fox et al, 2016).
The survey showed that the Hazelbaker (2010) assessment tool was most commonly used. Many practitioners find it helpful in its assessment of both function and appearance; however others conclude there are limitations with achieving inter-examiner reliability (Madlon-Kay et al, 2008). A systematic review noted that there is, as yet, no validated tool for diagnosis (Emmerson, 2018). Differences between assessment tools in practice is likely to continue until there is clear evidence, for example from a randomised controlled trial, as to which achieves optimal results.
To an extent,‘clinical judgement’ will always form part of any assessment, but whether this should be used alone without a more formalised assessment tool is still open to professional discussion. Many argue that diagnosis cannot be made by assessment of the baby alone (NICE, 2005; Oakley, 2021). Instead, they feel that a mother and baby dyad must be assessed together when feeding for more accurate diagnosis, which means the professional providing the assessment must have appropriate infant feeding knowledge and skills (Dixon et al, 2018; Oakley, 2021).
There does not appear to be much need for clinic-based follow-up appointments or specific aftercare routines or regimes, based on feedback given by practitioners (ATP members) in both the NHS and private practice, as well as practice audits. Most services only encouraged non-invasive approaches (regular feeding and/or tongue exercises), leaving the wound undisturbed to heal. Only 4% of services suggested the more invasive techniques of disturbing the wound in some way during healing. This aspect of clinical practice appears to provoke strong reactions among practitioners. Those advocating for active wound management or disruptive wound massage argue that it prevents ‘re-growth’ or scar tissue forming, thereby lessening the need for a second frenulotomy. Others argue that this disturbance of a healing wound could in fact increase the likelihood of re-growth or scar tissue formation. Bhandarkar et al (2022) stated massage following frenulotomy does not add benefit and therefore should not be advised. Dhir et al (2022) was less clear and stated that further research is needed before optimal post-frenulotomy care can be established. An ATP position statement on routine post frenulotomy care can be viewed on its website, but until there is more evidence, no firm conclusion can be drawn.
Conclusions
The results of this survey provided an interesting summary of current tongue tie services and insight into how they were affected by the COVID-19 pandemic. The authors would echo many of the same conclusions of the previous 2016 survey: tongue tie services in the UK are inequitable for mothers and babies and much further research is needed.
Key points
- This survey of UK NHS tongue tie service provision was based on the previous National Childbirth Trust survey, which concluded that access to services in the UK was a postcode lottery.
- The present survey included questions about the effect of the COVID-19 pandemic on provision of tongue tie services, as well as on the health professionals involved, referral times, and the signs and symptoms used to refer babies to services.
- The majority of tongue tie services involved midwives as the key professional, either working alongside medics or on their own.
- The most common waiting time was 2–4 weeks from referral to receiving an assessment and treatment.
- Although there has been an overall increase in the number of NHS services since the 2016 survey, there is still inconsistency in access, referral, provision and care offered.
CPD reflective questions
- In your experience, is information about tongue tie in babies given to parents at any stage of the childbirth continuum? Should information be given and, if so, what and when?
- Have you seen women and babies who have experienced difficulties with breast or bottle feeding because of tongue tie? How was the situation managed?
- When do you think is the optimal time to diagnose tongue tie: within 24 hours of birth, 1 week of birth or later? What are the advantages and disadvantages of the different timings?


