A sizable minority (10%–20%) of women describe their childbirth as a traumatic experience and have long-lasting negative memories of it (Olde et al, 2005; Bossano et al, 2017; Rijnders, 2011; Stramrood et al, 2011). Still, many women choose to give birth again. Previous research has aimed to understand what women actually mean by a traumatic childbirth experience. Answers include, for example, feeling neglected and experiencing loss of control during the birth, fear for their own or their baby's life, and a bad outcome (Beck, 2004; Thomson and Downe, 2008; Elmir et al, 2010; Henriksen et al, 2017; Hollander et al, 2017b). Traumatic birth experiences are therefore highly personal and subjective (Beck, 2004; Stramrood and Slade, 2017), meaning that a birth that seems normal and straightforward to a provider may be experienced as traumatic by the woman (Thomson and Downe, 2008).
Many previous studies have focused on self-defined traumatic birth (Greenfield et al, 2016; Leinweber et al, 2017; Fontein-Kuipers et al, 2018; Koster et al, 2019). The focus on women's subjective experiences has added value over studies using objective indicators, such as documented obstetric complications or Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria (American Psychiatric Association, 2013). First, factors associated with self-defined traumatic birth are distinct from factors associated with obstetric or neonatal complications (Harris and Ayers, 2012; Author, 2017b).
Second, even when mothers gave birth without being exposed to a threat to their or their baby's life, or to serious harm or violence (the ‘A criterion’ for post-traumatic stress disorder (PTSD) in DSM-5) (American Psychiatric Association, 2013), some of them still reported clinically relevant PTSD symptoms (Author, 2018c). Furthermore, women who self-identify with this label may make certain choices, and therefore it is important to understand their cognitions and emotions, irrespective of whether they may have symptoms that qualify for a clinical disorder. It should also be noted that in a previous study among women who self-identified as having had a traumatic childbirth experience, a majority of women met criterion A (ie exposure to actual or threatened death, serious injury or sexual violence) of the DSM-5 (75%) (van Heumen et al, 2018). For these reasons, the use of the term ‘traumatic childbirth experience’ throughout this paper, as well as for inclusion for this study, refers to women's subjective experiences.
A traumatic childbirth experience may lead to fear of another pregnancy, fewer subsequent births and a longer interval until the next pregnancy (Gottvall and Waldenström, 2002; Stramrood and Slade, 2017; Shorey et al, 2018). After a traumatic childbirth experience, the subsequent pregnancy may be filled with fear and mistrust in caregivers (Beck and Watson, 2010; Wijma and Wijma, 2017; Fairbrother et al, 2018; Greenfield et al, 2019) and in the subsequent pregnancy, women may focus on ‘resolving the past and preparing for the unknown’ (Thomson and Downe, 2010). Additionally, a previous traumatic birth experience may result in feelings of lack of control and, therefore, focusing on avoiding loss of control may become one of the main strategies that women have for the subsequent pregnancy and birth (Elmir et al, 2010; Greenfield et al, 2019). In the Netherlands, a majority of midwives screen pregnant women for fear of childbirth, offering then additional care to those in need, either by themselves or by referring to another specialist (eg to a specialised clinic at a local hospital) (de Vrie et al, 2018).
The subsequent birth itself has been suggested to either heal or re-traumatise women who have previous traumatic birth experiences (Beck and Watson, 2010; Thomson and Downe, 2010). A positive subsequent birth experience can offer a feeling of redemption, which supports women in overcoming their previous traumatic experience. Alternatively, a negative subsequent birth experience may cause re-experiencing the trauma. In contrast to women who also experienced their subsequent birth as traumatic, women with positive subsequent birth experiences attributed their positive experience to the fact that they felt connected with providers and experienced control over the birth process (Beck and Watson, 2010; Thomson and Downe, 2010).
Women may thus experience different negative emotions during their subsequent pregnancy and birth, and they may use various coping behaviours like focusing on self-nurturing, planning, seeking support from providers, and avoiding thinking about the upcoming birth (Beck and Watson, 2010; Thomson and Downe, 2010; Fenech and Thomson, 2015; Greenfield et al, 2019). Women coping with negative emotions may also lead them to deviate from recommended care (Gardner, 2003; Cheyney, 2008; Hollander et al, 2017a; Hollander et al, 2018; Shorey et al, 2018). Women may, for instance, request a planned caesarean section (c-section), home birth in a high-risk pregnancy or an unassisted childbirth against the recommendations made by their care providers (Gardner, 2003; Hollander et al, 2018). Previous studies have suggested that one reason for this may be a need for control during pregnancy and childbirth (Hollander et al, 2017a; Greenfield et al, 2018; Hollander et al, 2018; Shorey et al, 2018). Therefore, after a previous traumatic birth experience, women may be afraid of experiencing a lack of autonomy and support again which might lead them making decisions on their own accord rather than following medical advice (van Heumen et al, 2018).
There is little insight in the links between previous traumatic childbirth experiences and how women experience the subsequent birth. This limits the current understanding of how care providers can support these women during a subsequent pregnancy and birth. Furthermore, it is unclear how coping strategies translate into behaviours that may either be beneficial or harmful for pregnant women with previous traumatic birth experiences. Therefore, this study explored subsequent birth experiences in women with a previous traumatic childbirth experience. The first study aim was to explore which characteristics of the previous birth and trauma-related factors were associated with the subsequent birth experience. The second study aim was to test the association between fear of childbirth and coping behaviour during the subsequent pregnancy with subsequent birth experience.
Methods
Participants
Inclusion criteria for participants were 1) being at least 18 years of age 2) being able to fill out the questionnaire in Dutch 3) having had a traumatic childbirth experience in or after 2008 4) having had at least one more birth after the traumatic experience and 5) all births having taken place in the Netherlands. ‘Traumatic childbirth experience’ refers to the woman's own subjective experience, as outlined in the introduction and in line with many previous studies (Greenfield et al, 2016; Leinweber et al, 2017; Fontein-Kuipers et al, 2018; Koster et al, 2019). The only exclusion criterion was being currently pregnant.
Currently, pregnant women were excluded to prevent confusion between feelings about the impending birth with the feelings that women may have had during their previous pregnancy. The required sample size was calculated with the G*power (Version 3.1). The expected effect size was set to small (f2=0.02) according to Cohen's (1977) criteria, given the retrospective and exploratory nature of the study. Thus, for alpha of 0.05 and 0.80 power the required minimum sample size was 395 participants.
Measures
Data were collected in 2018 through an online 41-item questionnaire which was designed for this study. The questionnaire was in Dutch. Items were drawn from the item bank of the Capture group (Childbirth and Psychotrauma Research Group) which has explored factors associated with traumatic childbirth over the years (Hollander et al, 2017b; van Heumen, et al, 2018). Additionally, two items on coping behaviours were designed for the purpose of this study based on the findings from previous qualitative studies (Beck and Watson, 2010; Fenech and Thomson, 2015). Importantly, all items were reviewed by research practitioners in the Capture group and modified to meet current scientific and clinical standards.
Information on demographic characteristics and subsequent family planning was collected with items that had been used also in previous studies (Table 1). In addition, six sets of items were used for the analyses: 1) characteristics of the traumatic childbirth (‘What happened during birth? In medical terms?’) 2) factors to which women attributed the trauma (‘What made you perceive the birth as traumatic?’) 3) fear of childbirth during the subsequent pregnancy (‘During pregnancy, how afraid were you of the subsequent birth?’) 4) preparation during the subsequent pregnancy (‘How did you prepare yourself for giving birth again?’) 5) strategies for coping with emotions during the subsequent pregnancy (‘How did you cope with any negative emotions during this pregnancy?’) and 6) decisions taken by women that were against medical advice regarding care during the subsequent pregnancy and birth (‘Did you make any of the following choices regarding preparation for this birth?’).
Table 1. Information of the participants (N=474)
| Factor | Options / scale | Number (%) M (SD) | National number (%) |
|---|---|---|---|
| Education | Range: 1=basic education, 6=university | M=4.8, SD=0.9 | |
| Living situation | With partnerWithout partner | 97.3%2.8% | 1=67.2%a2=32.8% |
| Ethnicity | DutchOther | 93.2%6.8% | 1=74.3%b2=25.7%b |
| Age during traumatic childbirth | Range: 18−41 | M=28.9,SD=3.9 | M=31.1SD=4.8b |
| Parity at the time of the traumatic childbirth | 12> 3 | 86.5%11.8%1.7% | M=1.62a |
| Time between the births | Range: 0−10 years | M=2.8 yearsSD=1.6 | |
| Subsequent pregnancy planned | Wished for and plannedWished for, not plannedNot wished for and not planned | 83.8%15.6%0.6% | |
| Fear of childbirth during the subsequent pregnancy | Range: 1=no fear at all, 10=the worst fear you can imagine | M=6.8SD=2.5> 5=80.2% | |
| Subsequent childbirth experience | Very happySomewhat happyNo special feelingsNot very happyNot at all happy | 53.2%24.1%4.2%7.8%10.8% |
Note: National numbers are drawn from previous studies
a=CBS, 2014;
b=Perined, 2018
All answer options can be found in Table 2. All items were rated either ‘yes’ or ‘no’ with the exception of two items. First, ‘fear of childbirth’ assessed how afraid women were during pregnancy and was rated with one 10-point Likert-scale item. This item has been validated and a score of five or higher has been suggested to refer to clinically significant fear (Rouhe et al, 2009). Second, subsequent birth experience was measured with the following question: ‘How do you look back on the subsequent birth?’ and was rated on a five-point Likert-scale (1=very happy, 2=partly happy, 3=no special feelings, 4=not very happy, 5=not at all happy).
Table 2. Prevalence of the tested independent variables (N=474)
| Topic | Factor | Number (%) | National number (%) |
|---|---|---|---|
| Characteristics of previous traumatic birth | Spontaneous without interventions | 12 | 76 |
| Episiotomy | 42 | 22 | |
| Manual removal of placenta | 10 | 1 | |
| Induction of labour | 37 | 23 | |
| Labour augmentation | 46 | 20 | |
| Vacuum-assisted birth | 30 | 8 | |
| Planned caesarean section (c-section) | 2 | 8 | |
| Unplanned c-section | 26 | 8 | |
| Excessive blood loss (more than 1 000 ml) | 25 | 6 | |
| Shoulder dystocia | 6 | 1 | |
| Factors to which women attribute the trauma | Loss of control | 72 | |
| Medical complication for me | 54 | ||
| Pain | 50 | ||
| Fear for baby's life | 46 | ||
| Lack of communication | 44 | ||
| Long duration of the birth | 43 | ||
| No support from professionals | 40 | ||
| Lack of autonomy, involvement | 37 | ||
| A specific intervention | 37 | ||
| Medical complication for the baby | 30 | ||
| Lack of respect | 23 | ||
| Different than I expected | 21 | ||
| Bad ending | 17 | ||
| Lack of a specific intervention | 14 | ||
| Short duration of the birth | 8 | ||
| No support from my partner | 7 | ||
| Preparation during the subsequent pregnancy | Made a birth plan | 53 | |
| Wanted to know as much as possible | 53 | ||
| Support from professionals | 51 | ||
| Books, websites, social media | 35 | ||
| Support from my social network | 31 | ||
| Yoga, mindfulness etc | 18 | ||
| Support from other pregnant women | 14 | ||
| Pregnancy courses on physical health | 13 | ||
| Childbirth preparation classes | 9 | ||
| Hypnobirthing | 8 | ||
| Wanted to know as little as possible | 7 | ||
| Coping with emotions during the subsequent pregnancy | Positive thinking, encouraging myself | 57 | |
| Letting the emotions in | 30 | ||
| Avoiding, focussing on other topics | 29 | ||
| No negative emotions | 6 | ||
| Decisions against medical advice regarding care during the subsequent pregnancy and birth | Giving birth with my own midwife instead of under supervision of obstetrician | 8 | |
| Home birth instead of hospital birth | 5 | ||
| No diabetes test during pregnancy | 4 | ||
| No continuous fetal monitoring during birth | 3 | ||
| No IV access during birth | 3 | ||
| No ultrasound to calculate the due date | 1 | ||
| Unassisted pregnancy | 1 | ||
| Unassisted childbirth | 1 | ||
| More medical check-ups than recommended | 25 | ||
| Extra appointments to discuss my wishes regarding pregnancy and/or childbirth | 10 | ||
| Elective induction of labour | 5 | ||
| Planned caesarean section | 7 | ||
| Support from doula | 3 |
Note: National numbers are drawn from a previous study (Perined, 2018)
The study was aimed to comprehensively explore associated factors of birth experience. For example, the item asking about the decisions that women had made regarding care during the subsequent pregnancy and birth aimed at covering most choices that care providers see women making in clinical practice. Therefore, not all investigated factors have previously been shown to affect women's birth experience. Noteworthy is that all answer options were given in the questionnaire as they are listed in Table 2. That means that the interpretation of what, for example, ‘bad ending’ means, was done by participants.
Recruitment
The study was judged to be non-medical by the Medical Research Ethics Committees United (reference number W18.020) and to meet the ethical standards of the VU Amsterdam ethical review board for psychological research (VCWE-2018-075). Data collection took place between 11 April 2018 and 1 May 2018. Participants were recruited via online advertisements posted on social media forums related to traumatic childbirth experiences.
Similar recruiting procedures have been used before by the Capture group (Hollander et al, 2017b; van Heumen et al, 2018). The online advertisement included the following invitation: ‘Have you had a traumatic childbirth experience and had at least one other birth after that? If so, we hope that you will take part in this study’. The advertisement included a link to the study website which offered more information about the study and a link to the online questionnaire. Before answering the questions, participants were asked to provide digital informed consent.
Data analysis
The analyses for this study were performed using SPSS version 26 (IBM Corporation, Armonk, NY, US). Because the subsequent birth experience (the dependent variable) was ordinal, both research questions were analysed by using ordinal regression. All independent variables were dichotomous (‘yes’ or ‘no’ to the characteristics and behaviours presented in Table 2), apart from one ordinal variable (fear of childbirth). Given the exploratory nature of the study (ie testing a large number of independent variables), the Benjamini-Hochberg (B-H) procedure (Benjamini and Hochberg, 1995) was used to keep the false discovery rate (FDR) within 10%.
Results
A total of 474 Dutch women with previous traumatic childbirth experiences took part in this study. Women had been on average 28.9 years old at the time of the traumatic birth (SD=3.9) and for majority of them (86.5%) it had been their first childbirth. On average, the time between the traumatic birth and the subsequent birth was 2.8 years and majority of the subsequent pregnancies were wished for and planned (83.8%). Most women (80.2%) reported having experienced clinically significant fear of childbirth during the subsequent pregnancy. Of the descriptive characteristics, only the time between the previous traumatic birth and the subsequent birth was significantly associated with the subsequent birth experience (OR 0.86, SE=0.06, p=0.013, 95% CI 0.76–0.97). The longer the time between the two births, the more positive the subsequent birth experience. Descriptive characteristics of the participants are presented in Table 1.
Of the women, 53% were very happy, 24% somewhat happy, 4% had no special feelings, 8% were not very happy, and 11% were not at all happy with their subsequent birth. To reduce the skewness of the distribution, raw scores were inverted. The first research question investigated whether birth-related factors during the previous traumatic childbirth were associated with women's subsequent birth experiences. After adjusting p-values to control for false positive effects, none of the predictors showed a significant association with the subsequent birth experience.
The second research question investigated whether fear of childbirth and coping behaviour during the subsequent pregnancy were associated with the subsequent birth experience. Three of the coping behaviours were significantly associated with a more positive subsequent birth experience. Making a birth plan (OR 1.77, SE=0.21, p=0.006, 95% CI 1.18–2.66), choosing a home birth in a high-risk pregnancy against medical advice (OR 9.40, SE=0.79, p =0.005, 95% CI 2.00–44.17) and having a planned c-section (OR 2.82, SE=0.40, p=0.009, 95% CI 1.29–6.12) were all related to a more positive subsequent birth experience. Table 2 presents the incidence of all factors included in the questionnaire and Figure 1 contains the odds ratios per tested variable (eg odds for having a more positive subsequent childbirth experience if making a birth plan or choosing a home birth instead of hospital birth in a high-risk pregnancy).
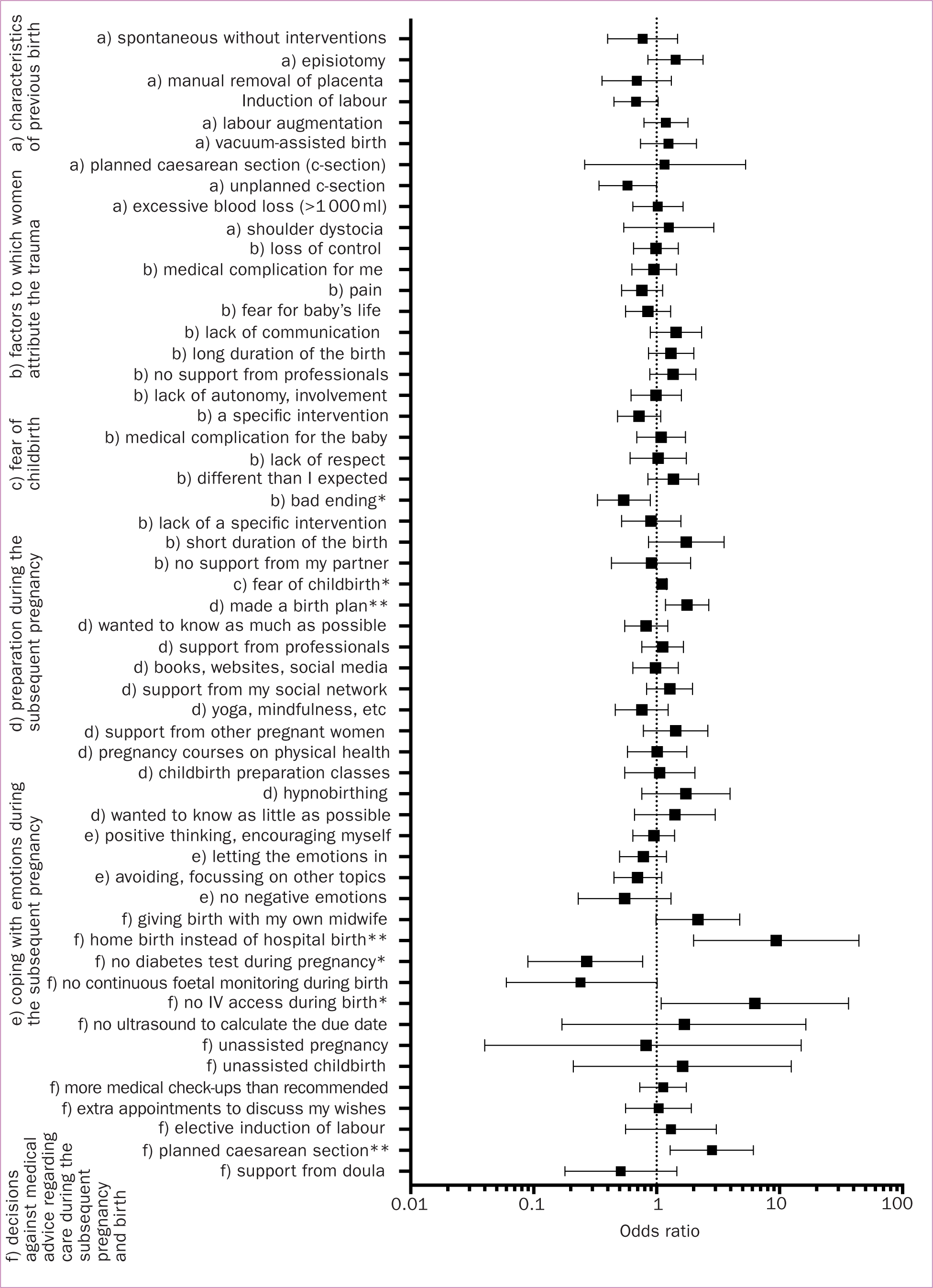 Figure 1. Odds ratios for a positive subsequent birth experience per all tested variables. *=p<0.05 but did not pass the B-H correction, **=p<0.05 and passed the B-H correction
Figure 1. Odds ratios for a positive subsequent birth experience per all tested variables. *=p<0.05 but did not pass the B-H correction, **=p<0.05 and passed the B-H correction
Discussion
In the subsequent pregnancy and birth, making a birth plan, choosing a home birth in a high-risk pregnancy against medical advice and having a planned c-section were all related to a more positive subsequent birth experience. Previous studies have suggested that because a previous traumatic birth experience may result in feelings of lack of control, women may focus on preparing for the unknown and avoiding loss of control during the subsequent pregnancy and birth (Elmir et al, 2010; Thomson and Downe, 2010; Greenfield et al, 2019). Making a birth plan is one strategy for doing this. Women with previous traumatic birth experiences may start writing their birth plan very early in pregnancy which is much earlier than the average pregnant woman (Greenfield et al, 2019). Making a birth plan may offer them more than just a way to communicate their wishes to care providers: it may have a psychological role in helping women with previous traumatic birth experiences to process their trauma, build trust in what is coming and, most importantly, offer a feeling of being in control of what is going to happen.
Furthermore, previous qualitative studies have found that after a previous traumatic birth experience, women may experience mistrust in caregivers (Greenfield et al, 2018) and women with positive subsequent birth experiences may attribute their positive experiences to the fact that they felt connected with providers (Beck and Watson, 2010; Thomson and Downe, 2010). Furthermore, women may even have a feeling that they do not have any option than to decide for home birth in a high-risk pregnancy because they have lost trust in providers (Hollander et al, 2019). These findings may explain why women who, against medical recommendations, chose to have a home birth in their subsequent pregnancy, had a more positive subsequent birth experience. More precisely, a subsequent home birth may offer women a feeling of control and intimacy (Cheyney, 2008; Beck and Watson, 2010), especially if the traumatic birth had taken place in a hospital setting (van der Garde et al, 2019). Taken together, the positive effect of a home birth is not necessarily about the place of giving birth but more about the one-on-one relationship that the women have with the providers when giving birth in a home setting.
In addition, previous research had already suggested that a planned c-section may help to prevent further trauma in women with previous traumatic birth experiences (Gardner, 2003). Gardner (2003) also suggests that whenever a multiparous woman decides to have a planned c-section without a medical reason, care providers ought to consider the possibility of a previous traumatic birth experience. This would enable them to better assist women in processing their previous trauma's and help them to take more control in planning the coming birth. In addition, being able to retain autonomy may be an important factor in explaining the positive effect of a planned c-section on the subsequent birth experience (Hollander et al, 2018). More precisely, if a woman has experienced not being in control during her previous traumatic birth process, making the decision regarding a planned c-section herself may offer her a sense of control over the coming birth.
In light of the positive effects of decisions made against medical advice found in this study, it is important to consider what providers could do to decrease the number of situations where women decide to go against medical advice but to also simultaneously offer women a more positive subsequent birth experience. One reason for decisions against medical advice may be women's need for control during the subsequent pregnancy and childbirth (Hollander et al, 2017a; Greenfield et al, 2018; Hollander et al, 2018; Shorey et al, 2018). Holten et al (2018) emphasise that the goal of women feeling in control during pregnancy and childbirth can be achieved by care providers ensuring a respectful, trustworthy and equal relationship with women. Greenfield et al (2019) also emphasise providers' role in promoting women's sense of control as their previous traumatic birth experience may have led them to mistrust all care providers.
Strengths and limitations
One strength of this study is that it investigates a variety of factors that may influence the subsequent childbirth experience after a traumatic birth experience. This broad search for associated factors indicates which areas might be more fruitfully investigated in future and which areas look less promising. Importantly, to the best of our knowledge, these are the first quantitative, large sample findings of subsequent childbirth experiences after a previous traumatic birth experience.
However, this study also has a few limitations. There was no control group of women without previous traumatic childbirth experiences. In addition, participants answered the questionnaire retrospectively which may have affected their recollection of their previous traumatic childbirth experience. In generalising these findings, one ought to consider that recruitment was done through social media and that this study was conducted in the Netherlands where maternity care is characterised by a high percentage of home births and independent midwifery. Finally, due to the hypothesis-generating, exploratory nature of the current study, more definitive insights await advancing the operationalisation of the construct of exercising control around childbirth, as well as future research that focuses on hypothesis testing.
Implications for practice
The most important message that the current study offers to care providers is to be aware of the potential importance that having control of the birthing process may have for women. Furthermore, women with a previous traumatic childbirth experience may struggle with trusting providers, especially if they meet them the first time only when giving birth. Therefore, focusing on enabling women to trust in providers, who assist them during birth, is of the utmost importance. Although a birthing process may include aspects that the woman had not planned for or wanted, respectful communication between providers may enable women to retain a sense of control. Feeling in control should, however, be considered important, not only for women with previous traumatic childbirth experiences but for all women giving birth.
As an explorative and correlational study, this study contributes to the current knowledge by focusing on identifying and eliminating possible related and unrelated predictors for the subsequent birth experience after a previous traumatic birth. Accordingly, future research is still needed to verify and strengthen these findings, as covering a large number of possible predictors limited the possibility of using widely used, validated instruments, as these were often too long and required too much time from the participants. Future studies can use these findings to help focus research efforts into preventing traumatic childbirth experiences.
Conclusion
This study investigated women's subsequent birth experiences after a previous traumatic childbirth experience in a sample of 474 Dutch women. Making a birth plan, choosing a home birth in a high-risk pregnancy against medical advice and having a planned c-section in the subsequent pregnancy were related to a more positive subsequent birth experience. Having control over the subsequent birth seemed to be the most important factor related to a more positive subsequent childbirth experience. These findings ought to be considered as a starting point for future research aimed at providing evidence-based support for pregnant women with previous traumatic birth experiences.
Key points
- After a traumatic childbirth experience, women are often afraid to become pregnant again, and may be at risk for also experiencing their subsequent childbirth as traumatic
- Based on an online survey filled out by 474 Dutch women, a majority (53%) of women had experienced their subsequent birth as very positive
- Making a birth plan, choosing a home birth in a high-risk pregnancy against medical advice and having a planned caesarean section in the subsequent birth were associated with their subsequent childbirth being experienced as more positive
- The issue of control over the subsequent birth may need to be pursued further in understanding practices that benefit childbirth in women with a history of traumatic birth
CPD reflective questions
- How can care providers use the data of this study to increase their client's chances of a better subsequent birth experience during pregnancy?
- Which factors are assumed by providers to promote positive birth experiences by women with a history of traumatic birth?
- Is making a birth plan enough?
- How will providers negotiate birth plans that are against medical advice, such as a home birth in a high-risk pregnancy or a caesarean section without medical reason?


