Autonomy is not a new concept in midwifery. Although not explicit, the term autonomy has been embedded in the definition of a midwife (International Confederation of Midwives [ICM], 2011). Reiterated in the core document of the ICM, autonomy may be identified, such as through the words: ‘responsible’, ‘accountable’ and ‘midwife's own responsibility’.
Like ICM (2011) and the Nursing and Midwifery Council ([NMC], 2017) in the UK, the United Nations Population Fund ([UNFPA], 2011) also reports that midwifery has been positioned and proclaimed as an autonomous profession within the national legislation of Indonesia, Myanmar, India and a few African countries. The concept of autonomy also resonates with the concept of midwifery-led care that was promoted more than 25 years ago in the UK with the publication of the Winterton report (House of Commons Health Committee, 1992). Despite the aforementioned, exercising autonomy in midwifery remains a global challenge and Brunei is no exception.
Although there is substantial literature on autonomy, the definition and description of autonomy remain unclear. Very often, autonomy has been subjected to varying definitions. The difficulty in defining autonomy is also frequently documented in the midwifery literature (Pollard, 2003). Autonomy remains a vague term and what exactly constitutes autonomy is still not precise. It is often used interchangeably with the term ‘independent’. There are similarities in various dictionaries for definitions of autonomy that include: ‘a state of being independent, free and self-directing from the control or power of another’ (Merriam-Webster Dictionary, 2019); ‘freedom from external control or influence’; and ‘the capacity … to act following objective morality rather than under the influence of desires’ (Stevenson, 2010).
The concept of autonomy was historically derived from a Greek term known as ‘autonomous’, which means ‘make its own laws’ (Maier, 2014). In healthcare ethics, Kant's deontological theory highlighted autonomy as an action which is deliberately and self-consciously motivated by moral reasons (Kant and Ellington, 1993). In the contemporary time, Beauchamp and Childress (2012) positioned autonomy as one among the four principles of ethics that was defined as the right of an individual to resist coercion or compulsion in the context of the relationship of power.
Autonomy is frequently conceptualised and tied with the philosophical and moral concept of healthcare, and is a fundamental legal requirement in healthcare (Mellado, 2016). Indeed, not only in Brunei but also all over the world, autonomy has been identified as an essential component in the principles of healthcare ethics and professional practice (Baykara and Sahinoglu, 2014; Maier, 2014). It has also been embedded in professional regulatory documents. For example, in the UK, autonomy is reiterated in the code for professional standards of practice and behaviour for nurses and midwives (NMC, 2018), and the standards for competence for registered midwives (NMC, 2009). Likewise, the Nursing Board for Brunei ([NBB], 2010) fundamentally emphasised this term in the Code of Ethics and Core Competency Standards (NBB, 2013). Autonomy is documented as a legal requirement in regulatory documents and is defined as ‘having the ability to make decisions about what to do rather than being influenced by someone else or told what to do’ (NBB, 2013).
In respect to the professional role of an autonomous midwife, she must be able to control her practice by demonstrating her ability in exercising choices and making clinical decisions independently with women (Fleming, 1998; Perdok et al, 2016). Despite the assertion, autonomy has long been documented as problematic for midwives. Even with acknowledgement of the importance of autonomy, midwives are frequently faced with the difficulty to exercise full autonomy or experience minimal autonomy in midwifery practices (Dove et al, 2017; Fleming, 1998). There are arguments on the notion of control in view of what choices are available; how the choices are to be conveyed to pregnant women; and how the control should be exercised (Symon, 1996). In essence, Symon (1996) highlighted the importance of healthcare professionals possessing a significant degree of autonomy over their practice, hence, facilitating the ability to control their practice.
The degree of being autonomous in midwifery may depend on various factors. Our professional experience observed that the context of a healthcare setting might be socio-culturally and politically influenced that may either facilitate or hinder midwives' autonomy. In the same vein, various fields of healthcare may embrace autonomy in different degrees, depending on their status or position. For instance, an obstetric consultant may be more autonomous than a junior doctor; a registered nurse-midwife than a registered midwife; a doctor than a nurse-midwife or midwife, and so on.
Globally, maternity care systems evidently have undergone dynamic and continuous transformations which makes the systems vary and be unique from each other, depending on where each system is situated. Some of these transformations, especially in urban areas, are coupled with modernity and technological advancements. By contrast, maternity care systems in remote and rural areas may not be contemporary and equipped with high technology.
Whether rural or urban, modern or remote, unforeseen implications can possibly impact midwives' practices, the central and foremost impact being decision-making undertaken by the midwives, and responsibility and accountability as a result of the decisions made. Very often, rural geographies lead to decisions made by midwives without the presence of doctors (Harris et al, 2011). Similarly, in urban areas, there may be injudicious decisions on the utilisation of technology and domination of the medical personnel (Catling et al, 2017; Russell, 2007). Consequently, midwives' decision-making and accountability, hence autonomy, are affected (Catling et al, 2017; Russell, 2007).
The interest in conducting this literature review is fuelled by the authors' clinical experiences in their country: Brunei. Brunei is moving towards an expansion of maternity and child health services. These can be observed from erections of the women and children centre buildings in two main referral public hospitals and the mushrooms of new primary health centres. These recent developments raised the authors' interest to promote a midwifery-led care model. Our understanding of midwifery-led care is along with the notion that a midwife takes the lead in providing midwifery care, and only makes referrals to obstetricians and other inter-professional teams when medical and other interventions require it. The concept of autonomy gradually becomes visible to us and is identified to be one among the various issues that we may have to consider in our planning to initiate and facilitate midwifery-led care.
Aims and objectives
This review aims to explore the principles and concepts underpinning autonomy, and to gain an insight into the significant aspects of autonomy in professional midwifery practice. Data from this literature review would be useful to provide empirical knowledge as a foundation for future research. The following research questions are addressed in this review: (1) What is the meaning of autonomy? (2) Is autonomy essential to practice, particularly in midwifery? (3) What is the impact of autonomy on midwifery practice?
Methods
Literature search strategy
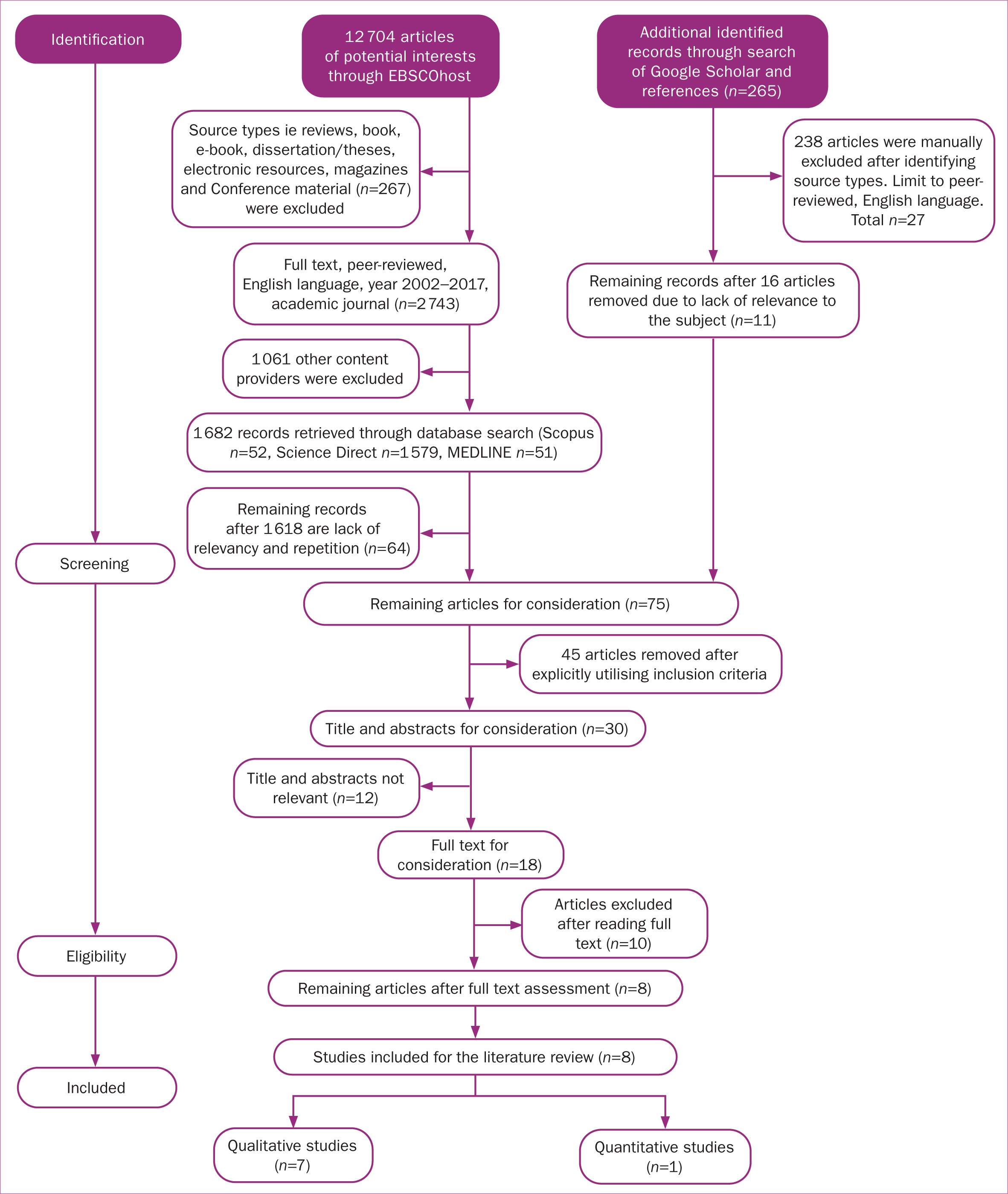
Existing research evidence from the perspective of midwifery and other maternity care providers associated with the concept of autonomy was searched. The electronic databases used for the search were Scopus, Science Direct and Medline within EBSCOhost, and Google Scholar. A broad range of search keywords aided by boolean operators such as definition, importance, impact, autonomy, autonomous were used in this search process.
The principal author conducted advance searching and screening for eligibility, guided by coherent inclusion/exclusion criteria in Table 1, where 10 potential studies were identified. Still, only eight were included in the review.
Table 1. Inclusion and exclusion criteria for selection of literature
| Feature | Inclusion | Exclusion |
|---|---|---|
| Language | Published in the English language |
|
| Date of Publication | January 2002 until November 2017 | |
| Type of studies |
|
Findings
Quality of the study
Eight studies (n=8) were finally included in the literature after being checked and reviewed by the co-authors (Table 2). The studies included in the review comprise a quantitative study and seven qualitative studies. All the studies focused on midwives, except for Perdok et al (2017) that focused on midwives, obstetricians and obstetric nurses. Two studies (Pollard, 2003; Perdok et al, 2017) were specific on midwifery autonomy and six studies were indirectly related to the concept of autonomy.
Table 2. Summary of studies included in the review
| Author/s, (country) | Design/study | Setting | Sampling method and participants | Data collection | Data analysis | Autonomy definition | Features of being autonomous individual | Impact of autonomy on the practice |
|---|---|---|---|---|---|---|---|---|
| Pollard, 2003 (UK) | Qualitative | Hospitals, community | Purposive and Snowball sample of midwives (n=27) [12 community midwives; 15 hospital-based midwives] | Semi-structured interviews | Thematic content analysis | Ability to make decisions, be responsible for actions and decisions | Preconditions of midwifery autonomy: midwives must have knowledge and authority or right to control of autonomy, scope of practice | The autonomous professional role, midwifery status, midwifery education and opportunities to control their autonomy and scope of practice |
| Hyde and Roche-Reid, 2004 (Ireland) | Qualitative | 3 maternity hospitals | Theoretical sample of midwives (n=12) | Semi-structured interviews | Grounded theory style of analysis | Relate autonomy with the concept of informed choice | Facilitative role for exercising choice and control for women during childbirth | Tension of modernity and its effects on the midwifery role and autonomy |
| Copeland et al, 2014 (Australia) | Qualitative, interpretative design | A variety of metropolitan hospitals | Purposive sampling of hospital-based midwives (n=12) | Photo elicitation during individual interviews | Thematic analysis | Not defined | Not identified | Lack of autonomy was affected by authoritarian leadership and obstetric knowledge |
| Hunter and Warren, 2014 (UK) | Exploratory qualitative descriptive | Professional online discussion group | Convenience, self-selected sample of midwives (n=11) | Closed online discussion using ‘light touch’ approach and vignette | Thematic analysis | Relate autonomy with being resilient midwives The ability to exercise choice and control to manage the challenges of practice | Self-awareness, self-knowledge | Workplace conditions, quality of care |
| Bedwell et al, 2015 (UK) | Hermeneutic phenomenology | Obstetric, alongside midwifery unit, freestanding birth centre and case-holding team at three hospital trusts | A purposive sample of midwives (n=12) who provide intrapartum care | Diaries and semi-structured interviews | Interpretive analysis | Relate autonomy to control over work | Not identified | Feeling helpless due to lack of control and lack of autonomy contribute to midwives losing confidence in their abilities |
| Davis and Homer, 2016 (Australia) | Qualitative, descriptive | Two continuity of midwifery care practices in a birth centre, home and labour ward | Midwives (n=12) | Focus group using semi-structured interviews | Thematic analysis | Relate autonomy with freedom to make own practice based decisions; ability to monitor progress and work | Not identified | Dominance of obstetric practice frameworks in the labour ward environment and surveillance of midwifery practice |
| Back et al, 2017 (Sweden) | Qualitative | 4 hospitals | Purposive sample of midwives (n=14) who works in labour wards | Focus group interviews | Content analysis | Not defined | Midwifery profession needs knowledge, competence, confidence and skills (personal qualities) | Not reported |
| Perdok et al, 2017 (Netherlands) | Cross-sectional survey | An email sent to a contact person of all 91 obstetric hospital departments, but 88 departments responded | Maternity care professional (n=799) [primary care midwives=362; obstetricians= 240; clinical midwives=93 and obstetric nurses=104] | Self-administered online: the Leiden Quality of Work Life questionnaire | SPSS, descriptive statistics and independent ANOVA | Not defined | Not defined | Job autonomy has positively and negatively impact on work-related condition and satisfaction; affect quality of care |
Out of seven qualitative studies, only four reported trustworthiness (Back et al, 2015; Bedwell et al, 2015; Pollard, 2003; Hunter and Warren, 2014). Almost half of the reviewed articles in this paper used triangulation or multiple sources of data collection from the sample population and reflectivity. Majority of the qualitative researchers reported dependability in their findings, especially for confirming the consistency of results by the detailed description of research methods, code/re-code procedure and peer examination. The quantitative study also reported the validity and reliability of the instrument.
Data analysis
Descriptive thematic analysis was used to analyse the data. Selected studies were read to identify similarity in their findings. These findings were then coded and arranged thematically to answer and correspond to the research questions under the following headings; (1) definition of autonomy; (2) features of being an autonomous midwife; and (3) impacts of autonomy on midwifery practice.
Definition of autonomy
Autonomy remains a term which is very difficult to define; hence, the existence of various definitions in the selected literature. The common definitions and descriptions of autonomy were associated with being knowledgeable of the scope of midwifery practice; having authority and being able to make decisions; being accountable for consequences of any decisions made. Out of the eight studies included in this literature review, only the study by Pollard (2003) specifically documented the definition of autonomy from the midwives' perspective.
Autonomy was defined as being able to make decisions and being responsible or accountable for taking actions and making decisions, facilitated by recognition of the scope of midwifery practice (Pollard, 2003). On the other hand, Perdok et al (2017) featured autonomy in their study as a concept that was associated with the authority of a midwife in undertaking decision-making.
Similarly, autonomy was described as a concept which was associated with informed choices; freedom to make own clinical or practice-based decisions; ability to monitor progress of and having the power to control over a situation, work or practice (Hyde and Roche-Reid, 2004; Bedwell et al, 2015; Davis and Homer, 2016;). In addition, Hunter and Warren (2014) linked the concept of autonomy with ‘resilient midwives' who are capable of managing the challenges within the midwifery practice by way of utilising choices and control over their work.
Features of being an autonomous midwife
The literature shows evidence that autonomy may be exercised personally in our daily life or professionally in midwifery practice. Various significant features of being an autonomous individual in caring for others were highlighted in the selected studies. Autonomy has been characterised by ways of being knowledgeable of the scope of midwifery practice (Back et al, 2015; Pollard, 2003); by being competent and confident in midwifery practice; and in making decisions (Hunter and Warren, 2014; Back et al, 2015; Bedwell et al, 2015).
Personal qualities were also identified as a fundamental feature of autonomy whereby midwives should have personal awareness and responsibility in providing the best care to their clients. Personal qualities were also tied to awareness of developing oneself into a resilient individual who has a strong sense of responsibility and can deal with challenges effectively within the working environment (Hunter and Warren, 2014; Back et al, 2015; Bedwell et al, 2015). In other words, a midwife needs to have passion, knowledge and understanding of their practice; be skilful, competent, and confident within their scope of practice.
This can facilitate the midwife to make appropriate decisions and be accountable for the consequences of the decisions they make in consultation with the women they care for. In other words, a midwife needs to understand their autonomous role within the scope of their practice (Pollard, 2003): what is meant by autonomy and how they can embrace it.
Impact of autonomy on midwifery practice
Being autonomous is viewed to have a significant impact on midwifery practice. The degree of being autonomous among midwives is identified to be influenced by their workplace (Pollard, 2003; Davis and Homer, 2016; Perdok et al, 2017). Midwives working in a primary health centre or a community health setting have a higher degree of autonomy than midwives working in a hospital setting (Pollard, 2003; Perdok et al, 2017). A decrease in autonomy among hospital-based midwives has been shown to have a negative impact on their job-related wellbeing and satisfaction; undermined the quality of midwifery care they provided (Perdok et al, 2017).
Hospital-based midwives were shown to experience minimal autonomy attributed by increased technological obstetric interventions that became a source of stress to them, that consequently attributed to more autonomy of the doctors (Hunter and Warren, 2014). Hospital-based midwives were also identified to have a low degree of autonomy due to numerous work-related responsibilities hindering them from undertaking an appropriate process of decision-making (Perdok et al, 2017). By contrast, some of the primary health centre midwives may experience a decrease in the degree of autonomy as a result of inadequate human resources and equipment that facilitate the provision of appropriate midwifery care (Hunter and Warren, 2014; Perdok et al, 2017).
A decrease of autonomy in midwifery practices may result in a reduction of midwives' confidence and their midwifery skills, and may induce the feeling of helplessness (Bedwell et al, 2015). Furthermore, Copeland et al (2014) claimed that midwives experience powerlessness because of dissatisfaction with the dominance of obstetric knowledge and overruling of the midwifery profession. Midwives become obliged to follow obstetric policies (Davis and Homer, 2016); the medical culture and norms (Bedwell et al, 2015) which may not always be appropriate in midwifery practice. Despite that, Hunter and Warren (2014) disagreed and asserted that midwives should view these as a professional challenge. A midwife who is knowledgeable, skilful, competent and confident, and utilises critical thinking abilities to cope and respond to these challenges more positively through working collaboratively with other healthcare professionals.
Discussion
On reviewing the literature, there have been very few studies that have adequately examined the meaning of autonomy in the context of midwifery. Despite the shortage of published articles in midwifery literature, nonetheless, there are three concept analyses by Ballou (1998), Keenan (1999) and Wade (1999) appearing in the nursing literature that would be useful to enhance the authors' understanding of the concept autonomy and its relationship to clinical practice. For example, Ballou (1998) used concept analysis to demonstrate that autonomy arises from an individual's characteristic who is influenced by the exposure of knowledge and ideas cultivated within the working environment. Whereas Keenan's (1999) analysis emphasised the importance of education and experiential knowledge that had enabled individuals to make an accountable judgement and decisions for their actions. Interestingly, Wade's (1999) analysis also regarded that pre-existing educational and personal qualities can foster professional autonomy. With these concept analyses, it provides valuable insight into guiding midwives and other MCPs about autonomous practices.
As mentioned above, although only half of the studies had narrated and clarified the meaning of autonomy, the existing evidence would be beneficial to facilitate directions or ways for the development of autonomy in midwifery practice. In fact, it has been consistently documented and emphasised in the literature that midwives are considered as autonomous practitioners. In this sense, it is essential for midwives who are registered under the national law as regulated health practitioners to understand their autonomous roles within the scope of midwifery practice. They are not only required to understand what autonomy is, but must also be able to become autonomous. Indeed, they must have the authority to make decisions. Furthermore, autonomy can only be embraced with the existence of adequate options for the availability of choices of care; knowledge on each option available; and have self-confidence in making decisions on the most appropriate option in providing the highest possible midwifery care. A midwife must also be accountable for the decisions she undertakes.
Midwives' attitudes may be shaped by their working environment, which directly affects their knowledge and autonomy. On that account, midwives must have a combination of knowledge and skill together with their extensive experience in caring for clients. A midwife should be acquainted with their scope of practice that, in turn, will enable her to make decisions and be accountable for the consequences of the decisions she makes. Uncertainty, limited or poor understanding of midwives' autonomous roles can hinder a midwife from embracing autonomy and thus weakens their status as professional midwives (Pollard, 2003).
Being an autonomous practitioner gives midwife control over their work. It also improves their competence and confidence level in making decisions, and, reciprocally, this will enable the midwives to assume responsibility for and authority over their clinical practices (Hunter and Warren, 2014; Back et al, 2015; Davis and Homer, 2016). Autonomy in midwifery practice is complex in nature. The uniqueness of autonomy and decision-making in midwifery practice is that it is shared with the women. The pregnant woman is central to the provision of midwifery care and must also be appreciated as an autonomous individual (Nieuwenhuijze et al, 2014; Thompson et al, 2016).
The literature review evidenced that midwives have perceived autonomy in midwifery as having both positive and negative impacts on midwifery practice. In other words, a midwife who is capable of being autonomous may presume that autonomy can have a positive effect on her practice, whereas for those who are unable to possess autonomy may feel that their professional role is not entirely fulfilled. The higher the level of autonomy experienced by the midwives, the higher the substantial possibility for them to control and engage with their work. With a higher level of self-control, the midwives in return may gain job satisfaction and self-confidence over their practice and the care provided to their clients (Bedwell et al, 2015; Warmelink et al, 2015).
Negatively, midwives' autonomy may not be judiciously embraced, hence, the tendency of midwives to overpower the women. In such a case, midwives take for granted women involvement in shared decision-making and neglect women as autonomous individuals. Likewise, a lack of autonomy was identified to have been attributed by work-related stress or burnout, low self-confidence, lack of institutional and social support when providing care within the demanding environment in the obstetric unit (Hunter and Warren, 2014; Bedwell et al, 2015; Creedy et al, 2017). The current knowledge concluded that autonomy is indispensable in midwifery. A thorough, more comprehensive and in-depth understanding of midwifery autonomy; what strengthened it; what has not; and how to be an autonomous midwife requires further research to be undertaken. The authors intend to conduct an in-depth qualitative study to further explore autonomy in midwifery practice in Brunei.
Methodological considerations and limitations of this review
All the included studies in this paper originated from western countries. For that reason, the author assumed that there is a deficit of studies focusing on this concept from the Asian region, including Brunei. The contexts and culture of autonomy and the scope of autonomous midwifery practice are different from one setting to another, and from one country to another.
From the literature review, the definition of autonomy within midwifery is still very vague. Some articles include an explanation of the concept of autonomy based on their interpretation. Majority of the definition of autonomy is still a broad concept. The findings from this review may not be similar to those countries in the Asian region, in the light of this limitation.
Implications for practice
The reviewed literature indicates that there are various existing pre-conditions to enhance autonomy in midwifery practices. The central element that most frequently documented in the literature is the capacity for decision-making; hence, a midwife should have the knowledge and skills required for making decisions. Midwifery is unique in that decision-making is shared with women.
Thus, the midwife needs to involve women in the process of decision-making. For decision-making to be undertaken effectively, a midwife should know her scope of practice and choices available for making decisions. Decisions should be based on the best possible options and a midwife must be accountable for the consequences of the decisions she makes. Personal qualities such as self-awareness, confidence, competence, critical thinking, and collaborative skills are also essential to be acquired by the midwife.
Conclusion
There is limited literature on autonomy within the context of midwifery practice. This review has provided valuable insights into the significant features and impact of autonomy on the midwifery practice. Autonomy remains highly significant, albeit debatable in midwifery. There must be a consensus about what constitutes autonomy in midwifery; the importance of being an autonomous midwife and how a midwife can be an autonomous practitioner. The meaning of autonomy is still inadequately defined, particularly in midwifery practice.
Key points
- The various dictionary definitions of autonomy include: ‘a state of being independent’, ‘free’ and ‘self-directing from the control or power of another’
- The notion of autonomy has long been embedded in midwifery professional regulatory documents and organisational rules
- A midwife should acquire specific personal qualities, be knowledgeable and have critical thinking skills, facilitating her confidence in making decisions which control her practice
- An autonomous midwife is capable of making choices and clinical decisions independently with women
- Qualities of an autonomous midwife include being knowledgeable, competent and confident in the scope of midwifery practice. They should also be a passionate individual and have a sense of responsibility in providing the best care to their clients and can deal with challenges effectively within the working environment
CPD reflective questions
- What is autonomy? To what extent are you autonomous in your own practice setting?
- Why is autonomy important in midwifery?
- As midwives, how do we be autonomous in our practice?


